阿茲海默症:修订间差异
无编辑摘要 标签:移除或更換文件 |
|||
| 第1行: | 第1行: | ||
{{medical}} |
|||
{{noteTA |
{{noteTA |
||
|T=zh-cn:阿尔茨海默病; zh-tw:阿茲海默症; zh-hk:阿茲海默症; |
|T=zh-cn:阿尔茨海默病; zh-tw:阿茲海默症; zh-hk:阿茲海默症; |
||
|1=zh-hans:恋恋笔记本; zh-hant:戀戀筆記本; zh-hk:忘了、忘不了; zh-tw:手札情緣; zh-mo:忘了、忘不了; |
|||
|G1=Medicine |
|||
| |
|2=zh-hans:依然爱丽丝; zh-hant:我想念我自己; zh-tw:我想念我自己; zh-hk:永遠的愛麗絲; zh-sg:我想念我自己; |
||
|3=zh-hans:柳暗花明; zh-hant:妳的樣子; zh-hk:妳的樣子; |
|||
}}'''{{medical}} |
|||
|G1 = Medicine |
|||
{{Infobox Disease |
|||
| Name = 阿茲海默症 |
|||
| Image = Alzheimer's_disease_brain_comparison.jpg |
|||
| Caption = 正常人的大腦(左)與阿茲海默症病患的大腦(右),標識處為相異的特徵。點圖可放大。 |
|||
| DiseasesDB = 490 |
|||
| ICD10 = {{ICD10|G|30||g|30}},{{ICD10|F|00||f|00}} |
|||
| ICD9 = {{ICD9|331.0}},{{ICD9|290.1}} |
|||
| ICDO = |
|||
| OMIM = 104300 |
|||
| MedlinePlus = 000760 |
|||
| eMedicineSubj = neuro |
|||
| eMedicineTopic = 13 |
|||
| MeshID = D000544 |
|||
}} |
}} |
||
{{Infobox medical condition (new) |
|||
[[File:Alzheimer disease video.webm|thumb|upright=1.4| |
|||
阿茲海默症 |
| name = 阿茲海默症 |
||
| image = Alzheimer's_disease_brain_comparison.jpg |
|||
<!-- 定義與症狀 --> |
|||
| caption = 比較正常(左)和阿茲海默症(右)患者的腦部。 |
|||
'''阿茲海默症'''({{lang-la|Morbus Alzheimer}},{{lang-de|Alzheimer-Krankheit}},[[縮寫]]:{{lang|de|AK}},{{lang-en|Alzheimer's disease}},[[縮寫]]:{{lang|en|AD}})或稱'''腦退化症'''。舊稱為{{lang-en|Senile Dementia of the Alzheimer Type}},[[縮寫]]:{{lang|en|SDAT}} 、奥茨海默症、老人失智症;俗稱早老性痴呆、老人痴呆(但醫界不建議使用此名稱{{備註|1=在香港,Dementia已經由「老人癡呆症」改名為「認知障礙症」;而Alzheimer’s Disease則命名為「阿爾茲海默氏症」。[http://www.hkada.org.hk/tc/?page_id=1840 認知障礙症成因及分類]鑑於「老年癡呆症」的歧視成分及標籤效應,有礙及早求診,由十個醫學及服務團體(包括香港認知障礙症協會在內)組成的專家聯盟於2012年進行了公眾諮詢。結果顯示市民與專業團體均普遍認同「認知障礙症」更能中立、準確地反映疾病的症狀(記憶與其他認知功能問題)、不局限於成因(退化與非退化性)、較易明白且不含歧視意味。}}),是一種發病進程緩慢、隨著時間不斷惡化的持續性[[神經]]功能障礙<ref name=WHO2014/>,此症佔了[[失智症]]中六到七成的成因<ref name=BMJ2009>{{cite journal|last1=Burns|first1=A|last2=Iliffe|first2=S|title=Alzheimer's disease.|journal=BMJ (Clinical research ed.)|date=5 February 2009|volume=338|pages=b158|pmid=19196745}}</ref><ref name=WHO2014>{{cite web|title=Dementia Fact sheet N°362|url=http://www.who.int/mediacentre/factsheets/fs362/en/|website=who.int|accessdate=28 November 2014|date=April 2012|deadurl=yes|archiveurl=https://web.archive.org/web/20150318030901/http://www.who.int/mediacentre/factsheets/fs362/en|archivedate=18 三月 2015}}</ref>。最常見的早期症狀,是難以記住最近發生的事情<ref name=BMJ2009/>,早期症狀還應該增加行為或性格的改變,「輕微行為能力受損」(Mild Behavioral Impairment, MBI)<ref>{{Cite web |url=http://www.alz.org/aaic/releases_2016/sun_445_ET.asp# |title=Beyond Memory Loss, Behavior Changes Are Often First Signs of Dementia. |access-date=2016-07-26 |archive-url=https://web.archive.org/web/20160728140931/http://www.alz.org/aaic/releases_2016/sun_445_ET.asp# |archive-date=2016-07-28 |dead-url=yes }}</ref>,對平日最喜歡的活動失去興趣、對人物冷感、對日常作息焦慮、無法控制衝動、多侵略性、挑戰社會規範、對食物失去興趣、事事疑心,突然經常動怒爆[[粗話]]。隨著疾病的發展,症狀可能會包含:[[譫妄]]、易怒、具攻擊性、無法正常言語、容易迷路、{{link-en|情緒不穩定|mood swing}}、喪失[[動機|生存動力]]、喪失[[長期記憶]]、難以自理和行為異常等<ref name=BMJ2009/><ref name=WHO2014/><ref name="pmid17222085"/><ref name="pmid17823840">{{cite journal |language=en |author=Tabert MH, Liu X, Doty RL, Serby M, Zamora D, Pelton GH, arder K, Albers MW, Stern Y, Devanand DP |title=A 10-item smell identification cale related to risk for Alzheimer's disease |journal=Ann. Neurol. |volume=58 |issue=1 |pages=155–160 |year=2005 |pmid=15984022 |doi=10.1002/ana.20533 |accessdate=2012-11-28}}</ref>。當患者的狀況變差時,往往會因此脫離家庭和社會關係<ref name=BMJ2009/><ref name="pmid17222085">{{cite journal |language=en |author=Waldemar G |title=Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline |journal=Eur J eurol |volume=14 |issue=1 |pages=e1–e26 |pmid=17222085 |doi=10.1111/j.1468-1331.2006.01605.x |author2=Dubois B |author3=Emre M |display-authors=3 |last4=Georges |first4=J. |last5=McKeith |first5=I. G. |last6=Rossor |first6=M. |last7=Scheltens |first7=P. |last8=Tariska |first8=P. |last9=Winblad |first9=B.|accessdate=2012-11-28|date=January 2007}}</ref><ref name="pmid17823840"/>,並逐漸喪失身體機能,最終導致死亡<ref name="nihstages">{{cite web|title=About Alzheimer's Disease: Symptoms|url=http://www.nia.nih.gov/alzheimers/topics/symptoms|publisher=National Institute on Aging|accessdate=28 December 2011}}</ref>。雖然疾病的進程因人而異,很難預測患者的[[預後]],但一般而言,確定診斷後的平均餘命是三到九年<ref name=NEJM2010>{{cite journal|last1=Querfurth|first1=HW|last2=LaFerla|first2=FM|title=Alzheimer's disease.|journal=The New England journal of medicine|date=28 January 2010|volume=362|issue=4|pages=329-44|pmid=20107219}}</ref>,確診之後存活超過十四年的病患少於3%<ref name="pmid7793228">{{cite journal |language=en |author=Mölsä PK, Marttila RJ, Rinne UK |title=Long-term survival and predictors of mortality in Alzheimer's disease and multi-infarct dementia |journal=ActaNeurol Scand |volume=91 |issue=3 |pages=159–64 |doi= |pmid=7793228 |accessdate=2012-11-28|date=March 1995}}</ref>。 |
|||
| field = [[神經內科]] |
|||
| synonyms = 老年痴呆症 |
|||
| symptoms = 短期記憶喪失、{{tsl|en|primary progressive aphasia|原發性進行性失語症|語言障礙}}、{{tsl|en|Orientation (mental)|定向障礙}}、{{tsl|en|mood swing|情緒不穩}}<ref name=BMJ2009/><ref name=WHO2017/> |
|||
| complications = |
|||
| onset = 大於65歲<ref name=Mend2012/> |
|||
| duration = 慢性<ref name=WHO2017/> |
|||
| causes = 瞭解有限<ref name=BMJ2009/> |
|||
| risks = [[遗传学|遺傳]]、[[頭部外傷]]、[[重性抑郁障碍|憂鬱症]]、[[高血壓]]<ref name=BMJ2009/><ref name=Lancet2011/> |
|||
| diagnosis = 排除其他可能原因後基於症狀和{{tsl|en|cognitive test|認知測試}}診斷<ref name=NICE2014Diag/> |
|||
| differential = 正常老化<ref name=BMJ2009/> |
|||
| prevention = |
|||
| treatment = |
|||
| medication = {{tsl|en|Acetylcholinesterase inhibitor|乙醯膽鹼抑制劑}}、{{tsl|en|NMDA receptor antagonist|NMDA受體拮抗劑}}(稍有幫助)<ref name=Pres2012/> |
|||
| prognosis = 餘命3至9年<ref name=NEJM2010/> |
|||
| frequency = 2.98億人(2015) |
|||
| deaths = 190萬人(2015) |
|||
}} |
|||
<!-- 定義和症狀 --> |
|||
'''阿茲海默症'''({{lang-en|Alzheimer's disease}},[[縮寫]]:{{lang|en|AD}}),俗稱早老性痴呆、老人痴呆(但醫界不建議使用此名稱{{備註|1=在香港,Dementia已經由「老人癡呆症」改名為「認知障礙症」;而Alzheimer’s Disease則命名為「阿爾茲海默氏症」。[http://www.hkada.org.hk/tc/?page_id=1840 認知障礙症成因及分類]鑑於「老年癡呆症」的歧視成分及標籤效應,有礙及早求診,由十個醫學及服務團體(包括香港認知障礙症協會在內)組成的專家聯盟於2012年進行了公眾諮詢。結果顯示市民與專業團體均普遍認同「認知障礙症」更能中立、準確地反映疾病的症狀(記憶與其他認知功能問題)、不局限於成因(退化與非退化性)、較易明白且不含歧視意味。}}),是一種發病進程緩慢、隨著時間不斷惡化的[[神经退行性疾病|神經退化性疾病]]<ref name="BMJ2009">{{Cite journal|title=Alzheimer’s disease|author=|url=https://www.bmj.com/content/338/bmj.b158|last=Iliffe|first=Steve|last2=Burns|first2=Alistair|date=2009-02-05|journal=BMJ|issue=|doi=10.1136/bmj.b158|others=|year=|volume=338|page=|pages=b158|language=|issn=1468-5833|pmid=19196745}}</ref><ref name="WHO2017" />,此病症佔了[[失智症]]中六到七成的成因<ref name=BMJ2009/><ref name=WHO2017/>。最常見的早期症狀為喪失[[短期记忆|短期記憶]](難以記住最近發生的事)<ref name="BMJ2009" />,當疾病除見進展,症狀可能逐漸出現,包括{{tsl|en|primary progressive aphasia|原發性進行性失語症|語言障礙}}、{{tsl|en|Orientation (mental)|定向障礙|}}(包括容易迷路)、{{tsl|en|mood swing|情感不穩|情緒不穩}}、喪失[[动机|動機]]、無法[[日常生活活動|自理]]和許多{{tsl|en|challenging behaviour|挑戰性行為|行為問題}}<ref name=BMJ2009/><ref name=WHO2017/>。當情況惡化時,患者往往會因此和家庭或社會脫節<ref name=BMJ2009/>,並逐漸喪失身體機能,最終導致死亡<ref name="nihstages">{{cite web|title=About Alzheimer's Disease: Symptoms|url=http://www.nia.nih.gov/alzheimers/topics/symptoms|publisher=National Institute on Aging|access-date=28 December 2011|deadurl=no|archive-url=https://web.archive.org/web/20120115201854/http://www.nia.nih.gov/alzheimers/topics/symptoms|archive-date=15 January 2012}}</ref>。雖然疾程因人而異,但診斷後的平均餘命約為三到九年<ref name=NEJM2010>{{Cite journal|title=Alzheimer's Disease|url=https://doi.org/10.1056/NEJMra0909142|last=Querfurth|first=Henry W.|last2=LaFerla|first2=Frank M.|date=2010-01-28|journal=New England Journal of Medicine|issue=4|doi=10.1056/NEJMra0909142|volume=362|pages=329–344|issn=0028-4793|pmid=20107219}}</ref><ref>{{Cite journal|title=Survival in dementia and predictors of mortality: a review|author=|url=https://onlinelibrary.wiley.com/doi/abs/10.1002/gps.3946|last=Todd|first=Stephen|last2=Barr|first2=Stephen|date=2013|journal=International Journal of Geriatric Psychiatry|issue=11|doi=10.1002/gps.3946|others=|year=|volume=28|page=|pages=1109–1124|language=|issn=1099-1166|pmid=|last3=Roberts|first3=Mark|last4=Passmore|first4=A. Peter}}</ref>。 |
|||
<!-- |
<!-- 病因、診斷和預防 --> |
||
阿茲海默症的真正成因至今仍然不明<ref name=BMJ2009/>。目前將阿茲海默症視為一種[[神經退行性疾病|神經退化的疾病]] |
阿茲海默症的真正成因至今仍然不明<ref name="BMJ2009" />。目前將阿茲海默症視為一種[[神經退行性疾病|神經退化的疾病]],並認為有將近七成的風險因子與[[遺傳]]有關<ref name="Lancet2011">{{Cite journal|title=Alzheimer's disease|url=https://linkinghub.elsevier.com/retrieve/pii/S0140673610613499|last=Ballard|first=Clive|last2=Gauthier|first2=Serge|date=2011-03|journal=The Lancet|issue=9770|doi=10.1016/s0140-6736(10)61349-9|volume=377|pages=1019–1031|issn=0140-6736|last3=Corbett|first3=Anne|last4=Brayne|first4=Carol|last5=Aarsland|first5=Dag|last6=Jones|first6=Emma}}</ref>;其他的風險因子還有[[頭部外傷]]、[[憂鬱症]]和[[高血壓]]<ref name="BMJ2009" />。疾病的進程與[[大腦]]中的{{link-en|纖維狀類澱粉蛋白質斑塊沉積|Senile plaques}}和[[Tau蛋白]]有關<ref name="Lancet2011" />。要診斷阿茲海默症,需根據病人病史、行為評估、{{link-en|認知測驗|Cognitive tests}}、腦部[[醫學影像|影像]]檢查和血液採檢來排除其他可能的因素<ref name="NICE2014Diag">{{cite web|url=https://pathways.nice.org.uk/pathways/dementia/dementia-assessment-and-diagnosis.pdf|title=Dementia diagnosis and assessment|accessdate=|author=|date=|publisher=National Institute for Health and Care Excellence (NICE)|access-date=2018-12-22|deadurl=|archive-url=https://web.archive.org/web/20141205184403/http://pathways.nice.org.uk/pathways/dementia/dementia-diagnosis-and-assessment.pdf|archive-date=2014-12-05}}</ref>。疾病初期的症狀常被誤認為是正常老化<ref name="BMJ2009" />。確診則需藉助腦部組織檢驗<ref name="Lancet2011" />。{{tsl|en|Mental exercise|腦力運動|身心}}和身體[[運動]]、避免[[肥胖症|肥胖]]都有助於減少罹患阿茲海默症的風險<ref name="Lancet2011" /><ref>{{cite web|url=https://www.nia.nih.gov/alzheimers/publication/preventing-alzheimers-disease/so-what-can-you-do|title=So, What Can You Do?|date=29 July 2016|publisher=National Institute on Aging|deadurl=yes|archive-url=https://web.archive.org/web/20170403110434/https://www.nia.nih.gov/alzheimers/publication/preventing-alzheimers-disease/so-what-can-you-do|archive-date=3 April 2017}}</ref>。目前沒有實證證明特定藥物或營養補充品對疾病治療有效<ref name="nonprevention">{{Cite journal|title=Primary and Secondary Prevention Trials in Alzheimer Disease: Looking Back, Moving Forward|author=|url=https://www.ncbi.nlm.nih.gov/pubmed/27697063|last=Hsu|first=David|last2=Marshall|first2=Gad A.|date=2017|journal=Current Alzheimer Research|issue=4|doi=10.2174/1567205013666160930112125|others=|year=|volume=14|page=|pages=426–440|issn=1875-5828|pmc=5329133|pmid=27697063}}</ref>。 |
||
<!-- 處置 --> |
<!-- 處置 --> |
||
目前並沒有可以阻止或逆轉病程的治療,只有少數 |
目前並沒有可以阻止或逆轉病程的治療,只有少數方法或許可以暫時緩解或改善症狀<ref name="WHO2017" />。疾病會使患者會越來越需要{{link-en|他人的照護|Caring for people with dementia}},這對照護者是一大負擔;這樣的照護壓力涵括了社會、生理、精神和經濟等各個層面<ref name="pmid17662119">{{Cite journal|title=Systematic review of information and support interventions for caregivers of people with dementia|url=https://doi.org/10.1186/1471-2318-7-18|last=Thompson|first=Carl A.|last2=Spilsbury|first2=Karen|date=2007-07-27|journal=BMC Geriatrics|issue=1|doi=10.1186/1471-2318-7-18|volume=7|pages=18|issn=1471-2318|pmc=1951962|pmid=17662119|last3=Hall|first3=Jill|last4=Birks|first4=Yvonne|last5=Barnes|first5=Colin|last6=Adamson|first6=Joy}}</ref>。運動計畫能改善病人的[[日常生活活動|日常生活]]功能,並可能可以改善預後<ref name="Forb2015">{{Cite journal|title=Exercise programs for people with dementia|url=http://dx.doi.org/10.1002/14651858.cd006489.pub4|last=Forbes|first=Dorothy|last2=Forbes|first2=Scott C|date=2015-04-15|journal=Cochrane Database of Systematic Reviews|doi=10.1002/14651858.cd006489.pub4|issn=1465-1858|last3=Blake|first3=Catherine M|last4=Thiessen|first4=Emily J|last5=Forbes|first5=Sean}}</ref>。由失智症狀引起的行為異常和[[思覺失調]]常以[[抗精神病藥]]治療,惟其效益不高且可能增加死亡率,因此通常不建議使用<ref>{{cite web|url=https://www.nice.org.uk/advice/ktt7/resources/non-guidance-lowdose-antipsychotics-in-people-with-dementia-pdf|title=Low-dose antipsychotics in people with dementia|author=National Institute for Health and Clinical Excellence|publisher=National Institute for Health and Care Excellence (NICE)|access-date=29 November 2014|deadurl=yes|archive-url=https://web.archive.org/web/20141205183329/https://www.nice.org.uk/advice/ktt7/resources/non-guidance-lowdose-antipsychotics-in-people-with-dementia-pdf|archive-date=5 December 2014|df=}}</ref><ref>{{cite web|url=http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124830.htm|title=Information for Healthcare Professionals: Conventional Antipsychotics|date=16 June 2008|publisher=US Food and Drug Administration|access-date=29 November 2014|deadurl=no|archive-url=https://web.archive.org/web/20141129015823/http://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm124830.htm|archive-date=29 November 2014}}</ref>。 |
||
<!-- 流行病學、歷史、社會 |
<!-- 流行病學、歷史、社會和研究--> |
||
2015年,全球大約有2980萬人罹患阿茲海默症<ref name="WHO2017">{{Cite web|url=https://www.who.int/news-room/fact-sheets/detail/dementia|title=Dementia|accessdate=2018-12-21|author=|date=|work=www.who.int|publisher=World Health Organization|language=}}</ref><ref name="GBD2015Pre">{{Cite journal|title=Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015|url=https://linkinghub.elsevier.com/retrieve/pii/S0140673616316786|last=Vos|first=Theo|last2=Allen|first2=Christine|date=2016-10|journal=The Lancet|issue=10053|doi=10.1016/s0140-6736(16)31678-6|volume=388|pages=1545–1602|issn=0140-6736|pmc=5055577|pmid=27733282|last3=Arora|first3=Megha|last4=Barber|first4=Ryan M|last5=Bhutta|first5=Zulfiqar A|last6=Brown|first6=Alexandria|last7=Carter|first7=Austin|last8=Casey|first8=Daniel C|last9=Charlson|first9=Fiona J}}</ref>。患者的發病年齡一般在65歲以上,但大約有4%到5%的患者會在65歲之前就發病,屬於{{link-en|早發性阿茲海默症|Early-onset Alzheimer's disease}}<ref name="Mend2012">{{Cite journal|title=Early-onset Alzheimer's Disease: Nonamnestic Subtypes and Type 2 AD|url=https://www.sciencedirect.com/science/article/abs/pii/S0188440912003372|date=2012-11-01|journal=Archives of Medical Research|issue=8|doi=10.1016/j.arcmed.2012.11.009|volume=43|pages=677–685|issn=0188-4409|pmc=3532551|pmid=23178565}}</ref>。65歲以上的盛行率約為6%<ref name="BMJ2009" />。2015年,失智症造成約190萬人死亡<ref name="GBD2015De">{{Cite journal|title=Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015|url=https://linkinghub.elsevier.com/retrieve/pii/S0140673616310121|last=Wang|first=Haidong|last2=Naghavi|first2=Mohsen|date=2016-10|journal=The Lancet|issue=10053|doi=10.1016/s0140-6736(16)31012-1|volume=388|pages=1459–1544|issn=0140-6736|pmc=5388903|pmid=27733281|last3=Allen|first3=Christine|last4=Barber|first4=Ryan M|last5=Bhutta|first5=Zulfiqar A|last6=Carter|first6=Austin|last7=Casey|first7=Daniel C|last8=Charlson|first8=Fiona J|last9=Chen|first9=Alan Zian}}</ref>。1906年,德國精神學家與病理學家[[愛羅斯·阿茲海默]]首先描述並隨後命名了阿茲海默症<ref name="pmid9661992">{{Cite journal|title=Evolution in the Conceptualization of Dementia and Alzheimer’s Disease: Greco-Roman Period to the 1960s|url=https://www.sciencedirect.com/science/article/pii/S0197458098000529|date=1998-05-01|journal=Neurobiology of Aging|issue=3|doi=10.1016/S0197-4580(98)00052-9|volume=19|pages=173–189|issn=0197-4580}}</ref> 。在[[已開發國家]]中,阿茲海默症是耗費最多社會資源的一種疾病<ref name="pmid15685097">{{vcite journal | vauthors = Bonin-Guillaume S, Zekry D, Giacobini E, Gold G, Michel JP | title = Impact économique de la démence (English: The Economical Impact of Dementia) | language = French | journal = Presse Médicale | volume = 34 | issue = 1 | pages = 35–41 | year = 2005 | pmid = 15685097 | issn = 0755-4982 | month = January | doi=10.1016/s0755-4982(05)83882-5}}</ref><ref name="pmid9543467">{{vcite journal | vauthors = Meek PD, McKeithan K, Schumock GT | title = Economic Considerations in Alzheimer's Disease | journal = Pharmacotherapy | volume = 18 | issue = 2 Pt 2 | pages = 68–73; discussion 79–82 | year = 1998 | pmid = 9543467 | doi = 10.1002/j.1875-9114.1998.tb03880.x}}</ref>。 |
|||
{{TOC limit|3}} |
|||
== |
==症狀和徵候== |
||
{{quote box |
|||
阿兹海默症是一组病因未明的原发性退行性脑变性疾病。多起病于老年期,潜隐起病,病程缓慢且不可逆,临床上以[[智力]]损害为主。病理改变主要为[[皮质]]弥漫性萎缩,沟回增宽,[[脑室]]扩大,[[神经元]]大量减少,并可见[[老年斑]](SP),[[神经原纤维结]](NFT)等病变,[[胆碱乙酰化酶]]及[[乙酰胆碱]]含量显著减少。起病在65岁以前者旧称老年病前期痴呆,或早老性痴呆,多有同病家族史,病情发展较快,[[颞叶]]及[[顶叶]]病变较显著,常有[[失语]]和[[失用]]。 |
|||
|title=阿茲海默症的分期<ref name="BBDAlzheimers">{{cite news | work = [[消费者报告|Consumer Reports]] {{tsl|en|Drug Effectiveness Review Project||Drug Effectiveness Review Project}} | date = May 2012 | title = Evaluating Prescription Drugs Used to Treat: Alzheimer's Disease Comparing Effectiveness, Safety, and Price | publisher = Consumer Reports | url = http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/AlzheimersFINAL.pdf | format = PDF | access-date = 1 May 2013 | deadurl = no | archive-url = https://web.archive.org/web/20120905164340/http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/AlzheimersFINAL.pdf | archive-date = 5 September 2012 | df = dmy-all }}</ref> |
|||
| |
|||
;{{tsl|en|Memory and ageing|記憶與老化|正常老化}}而非阿茲海默症造成的影響 |
|||
*有時會[[遗忘]]東西 |
|||
*有時會把物品放錯地方 |
|||
*輕微的[[短期记忆]]喪失 |
|||
*不記得確切的細節 |
|||
;阿茲海默症早期 |
|||
*不記得自己有遺忘事情 |
|||
*忘記家人或朋友的名字 |
|||
*可能只有密友或家人會發現變化 |
|||
*在不熟悉的情境下出現部分的意識混亂 |
|||
;阿茲海默症中期 |
|||
*更難記起新學到的資訊 |
|||
*在許多情況下意識混亂更加嚴重 |
|||
*睡眠問題 |
|||
*不知道自己在哪裡 |
|||
;阿茲海默症晚期 |
|||
*思考能力變差 |
|||
*說話問題 |
|||
*重複一樣的對話 |
|||
*更常辱罵、焦慮或被害妄想等 |
|||
}} |
|||
阿茲海默症的病程根據[[認知]]能力和身體機能的惡化程度分成四個時期,以下分段說明。 |
|||
== |
=== 失智症前期 === |
||
阿茲海默症最初的症狀常被誤認為是[[老化]]或是[[壓力 (醫學)|壓力]]<ref name="pmid17222085">{{vcite journal|vauthors=Waldemar G, Dubois B, Emre M|title=Recommendations for the Diagnosis and Management of Alzheimer's Disease and Other Disorders Associated with Dementia: EFNS Guideline|journal=European Journal of Neurology|volume=14|issue=1|pages=e1–26|year=2007|pmid=17222085|doi=10.1111/j.1468-1331.2006.01605.x|month=January}}</ref>,但若進行詳細的{{link-en|神經心理學檢查|Neuropsychological test}},甚至能在確診為阿茲海默症八年前就可發現輕微的認知困難<ref name="pmid15324363">{{vcite journal|vauthors=Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ|title=Multiple Cognitive Deficits During the Transition to Alzheimer's Disease|journal=Journal of Internal Medicine|volume=256|issue=3|pages=195–204|year=2004|pmid=15324363|doi=10.1111/j.1365-2796.2004.01386.x|month=Sep}}</ref>。這些早期症狀可以影響大部分複雜的[[日常生活活動]]<ref>{{vcite journal|vauthors=Nygård L|title=Instrumental Activities of Daily Living: A Stepping-stone Towards Alzheimer's Disease Diagnosis in Subjects with Mild Cognitive Impairment?|journal=Acta Neurologica Scandinavica|volume=Suppl|issue=179|pages=42–46|year=2003|pmid=12603250|doi=10.1034/j.1600-0404.107.s179.8.x}}</ref>,最明顯的缺陷是短期記憶障礙,主要是難以記住最近發生的事和無法吸收新資訊<ref name="pmid15324363" /><ref name="pmid12603249">{{vcite journal|vauthors=Arnáiz E, Almkvist O|title=Neuropsychological Features of Mild Cognitive Impairment and Preclinical Alzheimer's Disease|journal=Acta Neurologica Scandinavica|volume=179|pages=34–41|year=2003|pmid=12603249|doi=10.1034/j.1600-0404.107.s179.7.x}}</ref>。 |
|||
{{main|簡短智能測驗}} |
|||
其他症狀包括[[注意|注意力]][[管控功能|管控]]、計畫事情、彈性處理、[[抽象化|抽象思考]]和[[语义记忆|語義記憶]]等方面的問題<ref name="pmid15324363" />。[[冷漠]]也是此時期會出現的症狀之一,並會是在病程中持續出現的{{link-en|神經精神病學|Neuropsychiatry|精神}}症狀<ref>{{cite journal|title=Apathy in Alzheimer's disease|author=Landes AM, Sperry SD, Strauss ME, Geldmacher DS|date=Dec 2001|journal=J Am Geriatr Soc|accessdate=2012-12-09|issue=12|doi=10.1046/j.1532-5415.2001.49282.x|volume=49|pages=1700–7|pmid=11844006}}</ref>。阿茲海默症的臨床前期也被稱作{{link-en|輕微認知障礙|Mild cognitive impairment}}(MCI)<ref name="pmid126032492">{{cite journal|title=Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease|author=Arnáiz E, Almkvist O|journal=Acta Neurol. Scand., Suppl.|accessdate=2012-12-09|doi=10.1034/j.1600-0404.107.s179.7.x|year=2003|volume=179|pages=34–41|pmid=12603249}}</ref>,這是一個介於正常和[[失憶症]]之間的過渡狀態,但MCI可以是許多症候群的表現,而當它以記憶喪失為主要表現時,則稱作失憶性輕微認知障礙(amnestic MCI),此一名詞常被用來稱呼阿茲海默症的臨床前期<ref name="Grundman">{{cite journal|title=Mild cognitive impairment can be distinguished from Alzheimer disease and normal aging for clinical trials|date=January 2004|journal=Archives of Neurology|issue=1|doi=10.1001/archneur.61.1.59|volume=61|pages=59–66|pmid=14732621|vauthors=Grundman M, Petersen RC, Ferris SH, Thomas RG, Aisen PS, Bennett DA, Foster NL, Jack CR, Galasko DR, Doody R, Kaye J, Sano M, Mohs R, Gauthier S, Kim HT, Jin S, Schultz AN, Schafer K, Mulnard R, van Dyck CH, Mintzer J, Zamrini EY, Cahn-Weiner D, Thal LJ}}</ref>。 |
|||
[[File:PET Alzheimer.jpg|thumb|right|Upright|一個阿茲海默症患者的腦部[[正电子发射计算机断层扫描|正子電腦斷層掃瞄]],顯示顳葉失去功能。]] |
|||
=== 早期 === |
|||
阿茲海默症的初步診斷通常是由病患的臨床病史、親人的附帶病史和臨床醫師觀察到的神經學及神經心理學上的特徵,經{{link-en|除外診斷|Diagnosis of exclusion}}獲得<ref name="pmid17407994">{{vcite journal |accessdate=2014-01-27 |language=en |author=Mendez MF|title=The Accurate Diagnosis of Early-onset Dementia|journal=International Journal of Psychiatry Medicine|volume=36|issue=4|pages=401–412|year=2006|pmid=17407994|doi=10.2190/Q6J4-R143-P630-KW41}}</ref><ref name="pmid17018549">{{vcite journal |accessdate=2014-01-27 |language=en |author=Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J|title=Therapeutic Approaches to Alzheimer's Disease|journal=Brain|volume=129|issue=Pt 11|pages=2840–55|year=2006|pmid=17018549|doi=10.1093/brain/awl280}}</ref>,高階[[醫學影像|醫學影像技術]]如[[電腦斷層掃瞄]]、[[核磁共振成像]]、{{link-en|單光子電腦斷層攝影|Single-photon emission computed tomography}}和[[正電子發射計算機斷層掃描|正子電腦斷層攝影]]可以用來排除其他大腦病變或失智症亞型<ref>{{cite book |title=Dementia: Quick Reference Guide |publisher=(UK) National Institute for Health and Clinical Excellence |accessdate=2014-04-20 |year=2006 |location=London |language=en |isbn=1-84629-312-X |format=PDF |url=http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf |archiveurl=https://web.archive.org/web/20080227161412/http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf |archivedate=27 二月 2008 |deadurl=no }}</ref>。更重要的是,醫學影像也可以預測從輕微認知失調到阿茲海默症的轉變<ref name="pmid16327345">{{cite journal |author=Schroeter ML, Stein T, Maslowski N, Neumann J |title=Neural Correlates of Alzheimer's Disease and Mild Cognitive Impairment: A Systematic and Quantitative Meta-Analysis involving 1,351 Patients |journal=NeuroImage |volume=47 |issue=4 |pages=1196–1206 |year=2009 |pmid=19463961 |pmc=2730171 |doi=10.1016/j.neuroimage.2009.05.037}}</ref>。 |
|||
阿茲海默症病患的學習與記憶障礙會愈見明顯,最後使醫師能確認診斷。在少部分病患中,語言障礙、[[管控功能|執行]]障礙、認識障礙([[失认症|失認症]],agnosia)或技能執行障礙({{link-en|失用症|Apraxia}},apraxia)會比記憶障礙更明顯<ref name="pmid10653284">{{vcite journal|vauthors=Förstl H, Kurz A|title=Clinical Features of Alzheimer's Disease|journal=European Archives of Psychiatry and Clinical Neuroscience|volume=249|issue=6|pages=288–90|year=1999|pmid=10653284|doi=10.1007/s004060050101}}</ref>。阿茲海默症並不會對所有記憶能力都有同等的影響,相對於新近發生的事情或記憶,病患[[长期记忆|長期]]的[[情节记忆]]、[[语义记忆]]和[[内隐记忆]](身體記住如何做一件事,例如使用叉子吃東西)受到的影響比較少<ref name="pmid1300219">{{vcite journal|vauthor s=Carlesimo GA, Oscar-Berman M|title=Memory Deficits in Alzheimer's Patients: A Comprehensive Review|journal=Neuropsychology Review|volume=3|issue=2|pages=119–69|year=1992|pmid=1300219|doi=10.1007/BF01108841|month=June}}</ref><ref name="pmid8821346">{{vcite journal|vauthors=Jelicic M, Bonebakker AE, Bonke B|title=Implicit Memory Performance of Patients with Alzheimer's Disease: A Brief Review|journal=International Psychogeriatrics|volume=7|issue=3|pages=385–92|year=1995|pmid=8821346|doi=10.1017/S1041610295002134}}</ref>。 |
|||
阿茲海默症患者的語言障礙主要為{{link-en|原發性進行性失語症|Primary progressive aphasia}},特徵是病患可使用的[[詞彙]]變少,且{{link-en|流暢度|Fluency}}降低,導致病患的口語和[[书面语|書面表達]]變得困難<ref name="pmid10653284" /><ref name="pmid1856925">{{vcite journal|vauthors=Taler V, Phillips NA|title=Language Performance in Alzheimer's Disease and Mild Cognitive Impairment: a comparative review|journal=Journal of Clinical and Experimental Neuropsychology|volume=30|issue=5|pages=501–56|date=July 2008|pmid=18569251|doi=10.1080/13803390701550128}}</ref>。在這一時期,病患通常還能適當表達簡單的想法<ref name="pmid10653284" /><ref name="pmid1856925" /><ref name="pmid7967534">{{vcite journal|vauthors=Frank EM|title=Effect of Alzheimer's Disease on Communication Function|journal=Journal of the South Carolina Medical Association|volume=90|issue=9|pages=417–23|year=1994|pmid=7967534|month=September}}</ref>;當進行{{link-en|精細動作|Fine motor skill}}時(如寫作、畫圖、或是穿衣),可能會出現些微的動作不協調和計畫困難(失用症),但這些徵兆常會被忽略<ref name="pmid10653284" />。隨著疾病進展,阿茲海默症病患通常仍能獨立完成許多事情,但是大部分需要認知功能的活動可能就需要協助或是監督<ref name="pmid10653284" />。 |
|||
{{link-en|神經心理學評估|Neuropsychological assessment}}(包括記憶測試)可以進一步鑑別疾病狀態<ref name="pmid17222085"/>。醫學組織已經為臨床執業醫師建立診斷標準以簡化及標準化診斷程序,若是可以取得腦組織,則可以經由高準確度的[[組織學]]免疫染色法檢驗進一步確認診斷<ref name="pmid6610841">{{vcite journal|author=McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM|title=Clinical Diagnosis of Alzheimer's Disease: Report of the NINCDS-ADRDA Work Group under the Auspices of Department of Health and Human Services Task Force on Alzheimer's Disease|journal=Neurology|volume=34|issue=7|pages=939–44|year=1984|pmid=6610841}}</ref>。 |
|||
=== 中期 === |
|||
阿茲海默症的診斷先檢查病史、進行神經檢查及簡短的智能測驗。基本檢查有神經心理測試、血液常規、生化檢查(肝腎功能)、維他命B12濃度、甲狀腺功能、梅毒血清檢查及腦部電腦斷層或磁振造影等,特殊情況亦有其他檢查類型<ref name="檢察">[http://www.adc.org.cn/html/news/rsad_1242.shtml 阿茲海默氏症的檢查] {{Wayback|url=http://www.adc.org.cn/html/news/rsad_1242.shtml |date=20131013232710 }},2008年9月27日查閱</ref>。有失去記憶導致憂慮的症狀,就可能罹患了阿茲海默症,但必須經過醫師的智能測驗及腦部斷層掃描才能確定,以下是作為指標的智能量表。 |
|||
隨著病情惡化,病患將失去獨立生活的能力,而無法進行大部分的日常活動<ref name="pmid10653284" />。患者的語言障礙逐漸變得明顯,常會無法想起詞彙({{link-en|命名不能症|Anomic aphasia}}),會使用錯誤的字彙來替換({{link-en|言語錯亂症|paraphasia}}),同時也漸漸失去讀寫能力<ref name="pmid10653284" /><ref name="pmid7967534" />。患者在執行複雜的動作序列時會變得不協調,增加了跌倒的風險<ref name="pmid10653284" />。在這一時期,記憶問題也會惡化,病患可能無法認出親近的家屬<ref name="pmid10653284" />,之前仍完整的长期记忆也受到影響<ref name="pmid10653284" />。 |
|||
此時期行為和神經精神病學的變化也更為顯著,常見的表現包括{{le|遊蕩(醫學)|Wandering (dementia)|遊蕩}}、[[易怒]]和{{tsl|en|mood swing|情感不穩|情緒不穩}},這些變化會導致病患突然哭泣、突發的非故意攻擊行為、或是拒絕接受照顧<ref name="pmid10653284" />,此時也會出現[[日落症候群]]<ref>{{vcite journal|vauthors=Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A|title=Sundowning and Circadian Rhythms in Alzheimer's Disease|journal=The American Journal of Psychiatry|volume=158|issue=5|pages=704–11|year=2001|pmid=11329390|doi=10.1176/appi.ajp.158.5.704|month=May}}</ref>。大約30%的患者會產生出現{{tsl|en|Delusional misidentification syndrome|妄想錯認症候群|妄想錯認}}或其他[[妄想]]症狀<ref name="pmid10653284" />,另外也可能會尿失禁<ref name="pmid10653284" />。患者無法體認到疾病的進展({{tsl|en|anosognosia|病覺缺失症|病覺缺失症}},即缺乏病識感)<ref name="pmid10653284" />。這些症狀都會對家屬或照護者帶來壓力,由[[居家照護]]轉至{{tsl|en|Nursing home|長期照護機構|}}可減輕此類壓力<ref name="pmid10653284" /><ref name="pmid7806732">{{vcite journal|vauthors=Gold DP, Reis MF, Markiewicz D, Andres D|title=When Home Caregiving Ends: A Longitudinal Study of Outcomes for Caregivers of Relatives with Dementia|journal=Journal of the American Geriatrics Society|volume=43|issue=1|pages=10–16|year=1995|pmid=7806732|month=January|doi=10.1111/j.1532-5415.1995.tb06235.x}}</ref>。 |
|||
{| class="wikitable" |
|||
|- |
|||
!階段 |
|||
!智能測驗說明 |
|||
!症狀說明 |
|||
!平均期間 |
|||
!退化程度 |
|||
|- |
|||
| 一 |
|||
| (MMSE:29-30) |
|||
| 正常 |
|||
| - |
|||
| 成人 |
|||
|- |
|||
| 二 |
|||
| (MMSE:29) |
|||
| 正常年齡之健忘,與年齡有關之記憶障礙(忘記東西放置的地方及某些字,減少注意力) |
|||
| - |
|||
| 成人 |
|||
|- |
|||
| 三 |
|||
| 輕度神經認知功能障礙(MMSE:25) |
|||
| 降低從事複雜工作之能力及社會功能(例如:完成一件報告) |
|||
| - |
|||
| 年輕之成人 |
|||
|- |
|||
| 四 |
|||
| 輕度阿茲海默氏失智症(MMSE:20) |
|||
| 計算能力下降(100-7, 40-4),無法從事複雜活動(個人理財、料理三餐、上市場),注意力、計算及記憶障礙(近期為主) |
|||
| 2年 |
|||
| 8歲-青少年 |
|||
|- |
|||
| 五 |
|||
| 中度阿茲海默氏失智症(MMSE:14) |
|||
| 計算能力明顯下降(20-2),失去選擇適當衣服及日常活動之能力,走路緩慢、退縮、容易流淚、妄想、躁動不安 |
|||
| 1.5年 |
|||
| 5-7歲 |
|||
|- |
|||
| 六 |
|||
| 中重度阿茲海默氏失智症(MMSE:5) |
|||
| 無法唸10-9-8-7……,需他人協助穿衣、洗澡及上廁所,大小便失禁,躁動不安,降低語言能力 |
|||
| 2.5年 |
|||
| 5-7歲 |
|||
|- |
|||
| 七 |
|||
| 重度阿茲海默氏失智症(MMSE:0) |
|||
| 需依賴他人持續照顧,除叫喊外無語言能力、無法行走,行為問題減少,增加褥瘡、肺炎及四肢攣縮之可能性 |
|||
| MMSE從23(輕度)→0約6年,每年約降3-4分,MMSE到0後可平均再活2-3年 |
|||
| 4週-15個月 |
|||
|} |
|||
== |
=== 晚期 === |
||
在阿茲海默症的最終時期,病患已經完全依賴照護者<ref name="pmid10653284"/>,語言能力退化至簡單的詞語甚至僅有單字,最後完全失去談話能力<ref name="pmid10653284"/><ref name="pmid7967534"/>。除了失去口語能力之外,病患通常能理解並回應情感刺激<ref name="pmid10653284" />,雖然攻擊行為仍然存在,但大多時間表現得極度冷漠和[[疲倦]]<ref name="pmid10653284" />,病患最終無法獨立進行任何簡單的事情<ref name="pmid10653284" />,[[肌肉|肌肉質量]]和行動能力退化至長期臥床,也無法自行進食<ref name="pmid10653284" />。阿茲海默症是一種絕症,但死因通常是外在因素,例如[[褥疮]]感染或[[肺炎]],而不是疾病本身<ref name="pmid10653284" />。 |
|||
[[File:Auguste D aus Marktbreit.jpg|thumb|澳傑斯特·狄特,爱羅斯·阿茲海默第一個報告的阿兹海默症病人]] |
|||
[[德国]][[精神病学家]][[爱罗斯·阿兹海默]]於1907年<ref name="原始描述">{{cite journal |language=de | author=Alzheimer A | title = Über eine eigenartige Erkrankung der Hirnrinde.| journal = Allg. Z. Psychiat. Psych.-Gerichtl. Med.| volume = 64 | issue = 1–2 | pages = 146–148|date=Jan 1907}}</ref>最初報告了這一病症,并由此得名阿茲海默症。 |
|||
== |
==病因== |
||
阿茲海默症的病程根據[[認知]]能力和身體機能的惡化程度分成四個時期。 |
|||
大部分病患罹患阿茲海默症的原因仍然不明(除了1%到5%的病患可以找到基因差異)<ref>{{cite web|url=http://www.alz.org/research/science/alzheimers_disease_causes.asp|title=What We Know Today About Alzheimer's Disease|publisher=Alzheimer's Association|access-date=1 October 2011|quote=While scientists know Alzheimer's disease involves progressive brain cell failure, the reason cells fail isn't clear.|deadurl=no|archive-url=https://web.archive.org/web/20111007055341/http://alz.org/research/science/alzheimers_disease_causes.asp|archive-date=7 October 2011}} |
|||
===失智症前期=== |
|||
</ref><ref>{{cite journal | vauthors = Reitz C, Mayeux R | title = Alzheimer disease: epidemiology, diagnostic criteria, risk factors and biomarkers | journal = Biochemical Pharmacology | volume = 88 | issue = 4 | pages = 640–51 | date = April 2014 | pmid = 24398425 | pmc = 3992261 | doi = 10.1016/j.bcp.2013.12.024 }}</ref>。目前有幾個不同的[[假说]]嘗試解釋阿茲海默症的病因。 |
|||
最初的症狀常被誤認為是[[老化]]或是[[壓力 (醫學)|壓力]]<ref name="pmid17222085"/>,但是若進行詳細的{{link-en|神經心理學檢查|Neuropsychological test}}可能可以發現輕微的認知困難,甚至能在確診為阿茲海默症的八年前就可發現<ref name="pmid15324363">{{cite journal |language=en |author=Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ |title=Multiple cognitive deficits during the transition to Alzheimer's disease |journal=J Intern Med |volume=256 |issue=3 |pages=195–204 |pmid=15324363 |doi=10.1111/j.1365-2796.2004.01386.x|accessdate=2012-12-09|date=Sep 2004}}</ref>。這些早期症狀可以影響大部分複雜的[[日常生活活動]]<ref>{{cite journal |language=en |author=Nygård L 刀|title=Instrumental activities of daily living: a stepping-stone towards Alzheimer's disease diagnosis in subjects with mild cognitive impairment? |journal=Acta Neurol Scand |volume=Suppl |issue=179 |pages=42–6 |year=2003 |month= |pmid=12603250 |doi=10.1034/j.1600-0404.107.s179.8.x|accessdate=2012-12-09}}</ref>,最明顯的缺陷是失憶,主要是難以記住最近發生的事和無法吸收新資訊<ref name="pmid15324363"/><ref name="pmid12603249">{{cite journal |language=en |author=Arnáiz E, Almkvist O |title=Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease |journal=Acta Neurol. Scand., Suppl. |volume=179 |pages=34–41 |year=2003 |pmid=12603249 |doi=10.1034/j.1600-0404.107.s179.7.x|accessdate=2012-12-09}}</ref>,其他症狀包括出現在[[注意|注意力]]的[[管控功能|管控]]、計畫事情、彈性、和[[抽象化]]的微小問題,或是[[语义记忆]]障礙<ref name="pmid15324363"/>。[[冷漠]]也是此時期會出現的症狀之一,並且是整個病程中一直持續的{{link-en|神經精神病學|Neuropsychiatry}}症狀<ref>{{cite journal |language=en |author=Landes AM, Sperry SD, Strauss ME, Geldmacher DS |title=Apathy in Alzheimer's disease |journal=J Am Geriatr Soc |volume=49 |issue=12 |pages=1700–7 |pmid=11844006 |doi=10.1046/j.1532-5415.2001.49282.x|accessdate=2012-12-09|date=Dec 2001}}</ref>。阿茲海默症的臨床前期也被稱為{{link-en|輕微認知障礙|Mild cognitive impairment}}<ref name="pmid12603249"/>,然而這一名詞是否即是阿茲海默症的另一個診斷期或是可以作為鑑別阿茲海默症的第一步仍舊有爭議<ref name="pmid12603249"/><ref name="pmid17279076">{{cite journal |language=en |author=Petersen RC |title=The current status of mild cognitive impairment—what do we tell our patients? |journal=Nat Clin Pract Neurol |volume=3 |issue=2 |pages=60–1 |pmid=17279076 |doi=10.1038/ncpneuro0402|accessdate=2012-12-09|date=February 2007}}</ref>。 |
|||
=== |
===遺傳=== |
||
根據雙胞胎和家族研究,阿茲海默症的基因遺傳性約在49%到79%之間<ref name="pmid20930268">{{vcite journal | vauthors = Wilson RS, Barral S, Lee JH | title = Heritability of different forms of memory in the Late Onset Alzheimer's Disease Family Study. | journal = Journal of Alzheimer's Disease | volume = 23 | issue = 2 | pages = 249–55 | year = 2011 | pmid = 20930268 | doi = 10.3233/JAD-2010-101515 | pmc=3130303}}</ref><ref name="pmid16461860">{{vcite journal | vauthors = Gatz M, Reynolds CA, Fratiglioni L | title = Role of genes and environments for explaining Alzheimer disease | journal = Arch. Gen. Psychiatry | volume = 63 | issue = 2 | pages = 168–74 | year = 2006 | month = Feb | pmid = 16461860 | doi = 10.1001/archpsyc.63.2.168 }}</ref>。約0.1%家族性遺傳的患者為[[常染色体|體染色體]][[显性|顯性]]遺傳,他們常在65歲前發病,稱為{{tsl|en|Familial Alzheimer disease|家族性阿茲海默症|早發性家族性阿茲海默症}}<ref name="pmid16876668">{{vcite journal | vauthors = Blennow K, de Leon MJ, Zetterberg H | title = Alzheimer's Disease | journal = Lancet | volume = 368 | issue = 9533 | pages = 387–403 | year = 2006 | pmid = 16876668 | doi = 10.1016/S0140-6736(06)69113-7 | month = July }}</ref>。家族型阿茲海默症病患大多可以歸因於以下三個基因其中之一發生突變:[[前類澱粉蛋白質]]基因''APP'' 、''[[早老素|Presenilin]] 1''和<i>Presenilin 2</i><ref name="pmid18332245">{{vcite journal | vauthors = Waring SC, Rosenberg RN | title = Genome-wide association studies in Alzheimer disease | journal = Archives of Neurology | volume = 65 | issue = 3 | pages = 329–34 | year = 2008 | pmid = 18332245 | doi = 10.1001/archneur.65.3.329 | month = March }}</ref>, 這三個基因的突變大多會導致[[類澱粉蛋白|類澱粉蛋白質]]斑塊的主要成分{{tsl|en|Beta amyloid|β類澱粉胜肽|Aβ}}42在細胞中的產量升高<ref name=Selkoe>{{vcite journal | vauthors = Selkoe DJ | title = Translating cell biology into therapeutic advances in Alzheimer's disease | journal = Nature | volume = 399 | issue = 6738 Suppl | pages = A23–31 | year = 1999 | pmid = 10392577 | doi = 10.1038/19866 | month = June }}</ref>,一些突變雖然不增加Aβ42的產量,但會改變細胞內Aβ42和其他主要同型異構物(特別是Aβ40)的比例<ref name=Borchelt>{{vcite journal | vauthors = Borchelt DR, Thinakaran G, Eckman CB | title = Familial Alzheimer's disease-linked presenilin 1 variants elevate βA1-42/1-40 ratio in vitro and in vivo | journal = Neuron | volume = 17 | issue = 5 | pages = 1005–13 | year = 1996 | pmid = 8938131 | doi = 10.1016/S0896-6273(00)80230-5 |url=http://ac.els-cdn.com/S0896627300802305/1-s2.0-S0896627300802305-main.pdf?_tid=e1a5d3c4-f405-11e4-ac9c-00000aacb362&acdnat=1430926862_7e175593a77c62b8a2646077b6b07ba4 |format=PDF}}</ref><ref name="pmid17254019">{{vcite journal | vauthors = Shioi J, Georgakopoulos A, Mehta P | title = FAD mutants unable to increase neurotoxic Aβ 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta | journal = Journal of Neurochemistry | volume = 101 | issue = 3 | pages = 674–81 | year = 2007 | pmid = 17254019 | doi = 10.1111/j.1471-4159.2006.04391.x }}</ref>。 |
|||
在阿茲海默症病患身上的學習與記憶障礙會愈見明顯最後使醫師能確認診斷,在某些病患中,語言障礙、[[管控功能]]障礙、[[知觉]]障礙([[認識不能]],或稱失認症)或是行動障礙({{link-en|運用不能|Apraxia}},或稱失用症)會比記憶障礙更明顯<ref name="pmid10653284">{{cite journal |language=en |author=Förstl H, Kurz A |title=Clinical features of Alzheimer's disease |journal=European Archives of Psychiatry and Clinical Neuroscience |volume=249 |issue=6 |pages=288–290 |year=1999 |pmid=10653284 |doi=10.1007/s004060050101 |accessdate=2012-12-10}}</ref>。阿茲海默症並非對病患的所有記憶能力都有相同影響,相對於新近發生的事情或記憶,病患人生的[[长期记忆]]([[情节记忆]])、[[语义记忆]]和[[内隐记忆]](身體記住如何做一件事,例如使用叉子吃東西)受到的影響比較少<ref name="pmid1300219">{{cite journal |language=en |author=Carlesimo GA, Oscar-Berman M |title=Memory deficits in Alzheimer's patients: a comprehensive review |journal=Neuropsychol Rev |volume=3 |issue=2 |pages=119–69 |pmid=1300219 |doi=10.1007/BF01108841 |accessdate=2012-12-10|date=June 1992}}</ref><ref name="pmid8821346">{{cite journal |language=en |author=Jelicic M, Bonebakker AE, Bonke B |title=Implicit memory performance of patients with Alzheimer's disease: a brief review |journal=International Psychogeriatrics |volume=7 |issue=3 |pages=385–392 |year=1995 |pmid=8821346 |doi=10.1017/S1041610295002134 |accessdate=2012-12-10}}</ref>。 |
|||
阿茲海默症患者多數沒有上述的體染色體遺傳,稱為偶發型阿茲海默症。但有些基因或環境因素仍可能是罹患此病的危險因子。最著名的基因危險因子是[[载脂蛋白]]E(APOE)的ε4[[等位基因]]<ref name="pmid8446617">{{vcite journal|vauthors=Strittmatter WJ, Saunders AM, Schmechel D|title=Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease|journal=Proceedings of the National Academy of Sciences of the United States of America|volume=90|issue=5|pages=1977–81|year=1993|pmid=8446617|pmc=46003|doi=10.1073/pnas.90.5.1977}}</ref><ref name="pmid16567625">{{vcite journal|vauthors=Mahley RW, Weisgraber KH, Huang Y|title=Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer's disease|journal=Proceedings of the National Academy of Sciences of the United States of America|volume=103|issue=15|pages=5644–51|year=2006|pmid=16567625|pmc=1414631|doi=10.1073/pnas.0600549103|month=April}}</ref>,約有40%到80%的病患帶有至少一個APOEε4等位基因<ref name="pmid16567625" />,其中異型合子的個體罹患風險增加3倍,而同型合子則增加15倍<ref name="pmid16876668" />。然而,環境或基因造成的影響並不一定會完全[[外显度|表現出來]]。舉例來說,不同於其他族群,部分奈及利亞族群罹患阿茲海默症的機率和發病年齡與其是否帶有APOEε4沒有相關<ref name="pmid16434658">{{vcite journal|vauthors=Hall K, Murrell J, Ogunniyi A|display-authors=etal|title=Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba|journal=Neurology|volume=66|issue=2|pages=223–27|year=2006|pmid=16434658|pmc=2860622|doi=10.1212/01.wnl.0000194507.39504.17|month=January}}</ref><ref name="pmid16278853">{{vcite journal|vauthors=Gureje O, Ogunniyi A, Baiyewu O|title=APOE ε4 is not associated with Alzheimer's disease in elderly Nigerians|journal=Annals of Neurology|volume=59|issue=1|pages=182–85|year=2006|pmid=16278853|pmc=2855121|doi=10.1002/ana.20694|month=January}}</ref> 。遺傳學家已經檢驗超過400個候選基因與遲發性偶發性阿茲海默症(LOAD)的關聯,但大部分的基因都沒有發現明顯相關性<ref name="pmid16876668" /><ref name="pmid18332245" />。近期使用[[全基因组关联分析|全基因組關聯分析]](GWAS)的研究則找到了19個可能會影響罹病風險的基因區塊<ref name="GW2013">{{cite journal|title=Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease|date=December 2013|journal=Nature Genetics|issue=12|doi=10.1038/ng.2802|volume=45|pages=1452–8|pmc=3896259|pmid=24162737|vauthors=Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, DeStafano AL, Bis JC, Beecham GW, Grenier-Boley B, Russo G, Thorton-Wells TA, Jones N, Smith AV, Chouraki V, Thomas C, Ikram MA, Zelenika D, Vardarajan BN, Kamatani Y, Lin CF, Gerrish A, Schmidt H, Kunkle B, Dunstan ML, Ruiz A, Bihoreau MT, Choi SH, Reitz C, Pasquier F, Cruchaga C, Craig D, Amin N, Berr C, Lopez OL, De Jager PL, Deramecourt V, Johnston JA, Evans D, Lovestone S, Letenneur L, Morón FJ, Rubinsztein DC, Eiriksdottir G, Sleegers K, Goate AM, Fiévet N, Huentelman MW, Gill M, Brown K, Kamboh MI, Keller L, Barberger-Gateau P, McGuiness B, Larson EB, Green R, Myers AJ, Dufouil C, Todd S, Wallon D, Love S, Rogaeva E, Gallacher J, St George-Hyslop P, Clarimon J, Lleo A, Bayer A, Tsuang DW, Yu L, Tsolaki M, Bossù P, Spalletta G, Proitsi P, Collinge J, Sorbi S, Sanchez-Garcia F, Fox NC, Hardy J, Deniz Naranjo MC, Bosco P, Clarke R, Brayne C, Galimberti D, Mancuso M, Matthews F, Moebus S, Mecocci P, Del Zompo M, Maier W, Hampel H, Pilotto A, Bullido M, Panza F, Caffarra P, Nacmias B, Gilbert JR, Mayhaus M, Lannefelt L, Hakonarson H, Pichler S, Carrasquillo MM, Ingelsson M, Beekly D, Alvarez V, Zou F, Valladares O, Younkin SG, Coto E, Hamilton-Nelson KL, Gu W, Razquin C, Pastor P, Mateo I, Owen MJ, Faber KM, Jonsson PV, Combarros O, O'Donovan MC, Cantwell LB, Soininen H, Blacker D, Mead S, Mosley TH, Bennett DA, Harris TB, Fratiglioni L, Holmes C, de Bruijn RF, Passmore P, Montine TJ, Bettens K, Rotter JI, Brice A, Morgan K, Foroud TM, Kukull WA, Hannequin D, Powell JF, Nalls MA, Ritchie K, Lunetta KL, Kauwe JS, Boerwinkle E, Riemenschneider M, Boada M, Hiltuenen M, Martin ER, Schmidt R, Rujescu D, Wang LS, Dartigues JF, Mayeux R, Tzourio C, Hofman A, Nöthen MM, Graff C, Psaty BM, Jones L, Haines JL, Holmans PA, Lathrop M, Pericak-Vance MA, Launer LJ, Farrer LA, van Duijn CM, Van Broeckhoven C, Moskvina V, Seshadri S, Williams J, Schellenberg GD, Amouyel P}}</ref>,這些基因為{{tsl|en|CASS4||CASS4}}、[[CELF1]]、{{tsl|en|FERMT2||FERMT2}}、{{tsl|en|HLA-DRB5||HLA-DRB5}}、{{tsl|en|INPP5D||INPP5D}}、{{tsl|en|MEF2C||MEF2C}}、{{tsl|en|NME8||NME8}}、{{tsl|en|PTK2B||PTK2B}}、{{tsl|en|SORL1||SORL1}}、[[ZCWPW1]]、[[SlC24A4]]、{{tsl|en|CLU (gene)||CLU}}、{{tsl|en|PICALM||PICALM}}、{{tsl|en|Complement receptor 1||CR1}}、{{tsl|en|BIN1||BIN1}}、{{tsl|en|Membrane-spanning 4A||MS4A}}、{{tsl|en|ABCA7||ABCA7}}、{{tsl|en|EPHA1||EPHA1}}和[[CD2AP]]<ref name="GW2013" />。研究也發現''{{link-en|TREM2|TREM2}}''的某些等位基因變異會增加罹患阿茲海默症的風險達3到5倍,可能的原因是某些''TREM2''變異會使腦中的白血球將無法控制大腦中Aβ的產生量<ref>{{vcite journal|vauthors=Jonsson T, Stefansson H, Steinberg S|title=Variant of TREM2 associated with the risk of Alzheimer's disease|journal=The New England Journal of Medicine|volume=368|issue=2|pages=107–16|year=2012|pmid=23150908|pmc=3677583|doi=10.1056/NEJMoa1211103|type=Original article}}</ref><ref>{{vcite journal|vauthors=Guerreiro R, Wojtas A, Bras J|display-authors=etal|title=TREM2 variants in Alzheimer's disease|journal=The New England Journal of Medicine|volume=368|issue=2|pages=117–27|year=2012|pmid=23150934|pmc=3631573|doi=10.1056/NEJMoa1211851|author2=The Alzheimer Genetic Analysis Group|type=Original article}}</ref>。2018年的一項研究利用記憶、語言、視覺立體、執行,和功能等五個項目,配合新發表的30個與阿茲海默症相關的[[單核苷酸多態性]](SNPs),將阿茲海默症6大類<ref>{{Cite journal|title=Genetic data and cognitively defined late-onset Alzheimer’s disease subgroups|author=|url=https://www.nature.com/articles/s41380-018-0298-8|last=Crane|first=Paul K.|last2=Larson|first2=Eric B.|date=2018-12-04|journal=Molecular Psychiatry|issue=|doi=10.1038/s41380-018-0298-8|others=|year=|volume=|page=|pages=1|language=|issn=1476-5578|pmid=|last3=Keene|first3=C. Dirk|last4=Bennett|first4=David A.|last5=Jager|first5=Philip L. De|last6=Lopez|first6=Oscar L.|last7=Kamboh|first7=M. Ilyas|last8=Snitz|first8=Beth E.|last9=McCurry|first9=Susan M.}}</ref>。 |
|||
語言障礙({{link-en|原發性進行性失語症|Primary progressive aphasia}})的主要特徵是病患可使用的[[詞彙]]變少,並且{{link-en|流暢度|Fluency}}降低,因此導致病患的口語和[[书面语]]變得困難貧乏<ref name="pmid10653284"/><ref name="pmid1856925">{{cite journal |language=en |author=Taler V, Phillips NA |title=Language performance in Alzheimer's disease and mild cognitive impairment: a comparative review |journal=J Clin Exp Neuropsychol |volume=30 |issue=5 |pages=501–56 |pmid=18569251 |doi=10.1080/13803390701550128 |url= |accessdate=2012-12-10|date=July 2008}}</ref>,在這一時期,病患通常能適當地表達簡單的想法<ref name="pmid10653284"/><ref name="pmid1856925"/><ref name="pmid7967534">{{cite journal |language=en |author=Frank EM |title=Effect of Alzheimer's disease on communication function |journal=J S C Med Assoc |volume=90 |issue=9 |pages=417–23 |pmid=7967534 |accessdate=2012-12-10|date=September 1994}}</ref>;當進行{{link-en|精細動作|Fine motor skill}}例如寫作、畫圖、或是穿衣時,可能會出現一些動作不協調以及計畫困難(動作缺陷症),但這些徵兆通常會被忽略<ref name="pmid10653284"/>。隨著疾病進展,阿茲海默症病患仍然能獨立地完成許多事情,但是大部分需要認知功能的活動可能就需要協助或是監督<ref name="pmid10653284"/>。 |
|||
=== |
=== 膽鹼性假說 === |
||
{{link-en|膽鹼性|Cholinergic}}假說是最早被提出來的假說,也是現今大部分阿茲海默症藥物所依據的理論基礎<ref name="pmid10071091">{{vcite journal | vauthors = Francis PT, Palmer AM, Snape M, Wilcock GK | title = The Cholinergic Hypothesis of Alzheimer's Disease: a Review of Progress | journal = Journal of Neurology, Neurosurgery, and Psychiatry | volume = 66 | issue = 2 | pages = 137–47 | year = 1999 | pmid = 10071091 | pmc = 1736202 | doi = 10.1136/jnnp.66.2.137 | month = February }}</ref>,該假說認為阿茲海默症是由於神經系統減少產生[[神經傳導物質]][[乙酰胆碱]]而造成的,雖然膽鹼性假說的歷史悠久,但是沒有受到廣泛的支持,主要是由於使用藥物治療乙醯膽鹼缺乏後,對於阿茲海默症的療效有限<ref>{{cite journal | vauthors = Martorana A, Esposito Z, Koch G | title = Beyond the cholinergic hypothesis: do current drugs work in Alzheimer's disease? | journal = CNS Neuroscience & Therapeutics | volume = 16 | issue = 4 | pages = 235–45 | date = August 2010 | pmid = 20560995 | doi = 10.1111/j.1755-5949.2010.00175.x }}</ref>。 |
|||
隨著病情漸漸惡化將導致病患失去獨立性而無法進行大部分的日常生活活動<ref name="pmid10653284"/>。由於無法想起詞彙({{link-en|命名不能症|Anomic aphasia}})使語言障礙變得明顯,導致經常出現錯誤的字彙替換({{link-en|言語錯亂症|paraphasia}}),同時也漸漸失去讀寫能力<ref name="pmid10653284"/><ref name="pmid7967534"/>,複雜的動作變得不協調,因此增加跌倒的風險<ref name="pmid10653284"/>,在這一時期,記憶問題會惡化,病患可能變得無法認得親近的家屬<ref name="pmid10653284"/>,之前仍完整的长期记忆也受到影響<ref name="pmid10653284"/>。 |
|||
=== 類澱粉胜肽假說 === |
|||
此時期行為和神經精神病學的變化也更為顯著,常見的表現是{{le|遊蕩 (醫學)|Wandering (dementia)|遊蕩}}、[[易怒]]和[[假性延髓情绪]],這些變化導致病患突然哭泣、突發的非故意攻擊行為、或是拒絕接受照顧<ref name="pmid10653284"/>,此時也會出現[[日落症候群]]。 |
|||
1991年,學者提出類澱粉胜肽假說,認為{{link-en|β類澱粉胜肽|Beta amyloid}}(Aβ)在大腦堆積可能是導致阿茲海默症的根本原因<ref name="pmid1763432">{{vcite journal|vauthors=Hardy J, Allsop D|title=Amyloid Deposition as the Central Event in the Aetiology of Alzheimer's Disease|journal=Trends in Pharmacological Sciences|volume=12|issue=10|pages=383–88|year=1991|pmid=1763432|doi=10.1016/0165-6147(91)90609-V|month=October}}</ref><ref name="pmid11801334">{{vcite journal|vauthors=Mudher A, Lovestone S|title=Alzheimer's disease-do tauists and baptists finally shake hands?|journal=Trends in Neurosciences|volume=25|issue=1|pages=22–26|year=2002|pmid=11801334|doi=10.1016/S0166-2236(00)02031-2|month=January}}</ref>。有關[[唐氏综合症|唐氏症]]患者的研究支持了這項假說,表現Aβ的[[前類澱粉蛋白質|前類澱粉蛋白]]基因(<i>APP</i>)位在[[21號染色體]]上,而唐氏症病患多了一個21號染色體的副本,同時唐氏症病患幾乎全都在40歲左右時罹患阿茲海默症<ref name="pmid16904243">{{vcite journal|vauthors=Nistor M, Don M, Parekh M|title=Alpha- and Beta-secretase Activity as a Function of Age and Beta-amyloid in Down Syndrome and Normal Brain|journal=Neurobiology of Aging|volume=28|issue=10|pages=1493–506|year=2007|pmid=16904243|pmc=3375834|doi=10.1016/j.neurobiolaging.2006.06.023|month=October}}</ref><ref name="pmid15639317">{{vcite journal|vauthors=Lott IT, Head E|title=Alzheimer Disease and Down Syndrome: Factors in Pathogenesis|journal=Neurobiology of Aging|volume=26|issue=3|pages=383–89|year=2005|pmid=15639317|doi=10.1016/j.neurobiolaging.2004.08.005|month=March}}</ref>。此外,{{link-en|E型載脂蛋白4|APOE4}}(APOE4)是上阿茲海默症的主要遺傳危險因子,雖然載脂蛋白會增強Aβ的降解,但特定的載脂蛋白異構體對此反應的效果較差(如APOE4),導致多餘的Aβ在大腦中累積<ref name="pmid7566000">{{vcite journal|vauthors=Polvikoski T, Sulkava R, Haltia M|title=Apolipoprotein E, Dementia, and Cortical Deposition of Beta-amyloid Protein|journal=The New England Journal of Medicine|volume=333|issue=19|pages=1242–47|year=1995|pmid=7566000|doi=10.1056/NEJM199511093331902|month=November}}</ref>。進一步的證據則是來自於[[转基因生物|基因轉殖]]鼠實驗,研究人員在實驗鼠身上表現突變型人類''APP''基因,結果發現其大腦會產生纖維狀類澱粉蛋白斑塊(fibrillar amyloid plaques),並出現類似阿茲海默症的大腦病理變化及空間學習障礙<ref>基因轉殖鼠相關文獻: |
|||
* {{vcite journal|vauthors=Games D, Adams D, Alessandrini R|title=Alzheimer-type Neuropathology in Transgenic Mice Overexpressing V717F Beta-amyloid Precursor Protein|journal=Nature|volume=373|issue=6514|pages=523–27|year=1995|pmid=7845465|doi=10.1038/373523a0|month=February}} |
|||
* {{vcite journal|vauthors=Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D|title=Comparison of Neurodegenerative Pathology in Transgenic Mice Overexpressing V717F Beta-amyloid Precursor Protein and Alzheimer's Disease|journal=The Journal of Neuroscience|volume=16|issue=18|pages=5795–811|year=1996|pmid=8795633|month=September}} |
|||
* {{vcite journal|vauthors=Hsiao K, Chapman P, Nilsen S|title=Correlative Memory Deficits, Abeta Elevation, and Amyloid Plaques in Transgenic Mice|journal=Science|volume=274|issue=5284|pages=99–102|year=1996|pmid=8810256|doi=10.1126/science.274.5284.99}} |
|||
* {{vcite journal|vauthors=Lalonde R, Dumont M, Staufenbiel M, Sturchler-Pierrat C, Strazielle C|title=Spatial Learning, Exploration, Anxiety, and Motor Coordination in Female APP23 Transgenic Mice with the Swedish Mutation|journal=Brain Research|volume=956|issue=1|pages=36–44|year=2002|pmid=12426044|doi=10.1016/S0006-8993(02)03476-5}}</ref>。 |
|||
曾有一種實驗性疫苗在早期人體試驗中可以清除類澱粉蛋白斑塊,但此種治療對失智症卻沒有顯著的效果<ref name="pmid18640458">{{vcite journal | vauthors = Holmes C, Boche D, Wilkinson D | title = Long-term Effects of Abeta42 Immunisation in Alzheimer's Disease: Follow-up of a Randomised, Placebo-controlled Phase I Trial | journal = Lancet | volume = 372 | issue = 9634 | pages = 216–23 | year = 2008 | pmid = 18640458 | doi = 10.1016/S0140-6736(08)61075-2 | month = July }}</ref>。因此研究者轉而懷疑沒有形成大型類澱粉蛋白斑塊的Aβ[[低聚物|寡聚體]]才是主要的致病型態,這些寡聚體也被稱為類澱粉蛋白質衍生可溶性[[配體 (生物化學)|配體]](amyloid-derived diffusible ligands, ADDLs),它們會結合到神經細胞表面的[[受体 (生物化学)|受體]]並改變[[突觸]]的結構,因此會破壞神經元溝通<ref name="pmid17251419">{{vcite journal | vauthors = Lacor PN, Buniel MC, Furlow PW | title = Aß Oligomer-Induced Aberrations in Synapse Composition, Shape, and Density Provide a Molecular Basis for Loss of Connectivity in Alzheimer's Disease | journal = The Journal of Neuroscience | volume = 27 | issue = 4 | pages = 796–807 | year = 2007 | pmid = 17251419 | doi = 10.1523/JNEUROSCI.3501-06.2007 | month = January }}</ref>。其中一種可能的Aβ寡聚體受體可能是[[普利昂蛋白]],這種蛋白的錯誤構型會引起[[牛海綿狀腦病|狂牛症]]和人類[[庫賈氏症]],因此暗示著阿茲海默症與其他[[神經退化性疾病]]的機轉可能互有關聯<ref name="pmid192424752">{{cite journal|title=Cellular Prion Protein Mediates Impairment of Synaptic Plasticity by Amyloid-β Oligomers|author=Lauren J|date=February 2009|journal=Nature|accessdate=2012-12-23|issue=7233|doi=10.1038/nature07761|volume=457|pages=1128–32|pmc=2748841|pmid=19242475|last3=Nygaard|first3=Haakon B.|last4=Gilbert|first4=John W.|last5=Strittmatter|first5=Stephen M.|display-authors=2|author2=Gimbel D}}</ref>。 |
|||
=== 晚期症狀 === |
|||
在阿茲海默症的最終時期,病患已經完全依賴照護者<ref name="pmid10653284"/>,語言能力退化至簡單的詞語甚至僅有單字,最後完全失去談話能力<ref name="pmid10653284"/><ref name="pmid7967534"/>,除了失去口語能力之外,病患通常能理解及回應情感刺激<ref name="pmid10653284"/>,雖然攻擊行為仍然存在,但極度冷漠和[[疲倦]]成為更常見的症狀<ref name="pmid10653284"/>,最終病患會無法獨立進行任何事務<ref name="pmid10653284"/>,[[肌肉|肌肉質量]]和行動能力退化至長期臥床,也無法自行進食<ref name="pmid10653284"/>。阿茲海默症是一種絕症,但是死因通常是外在因素,例如[[褥疮]]感染或是[[肺炎]],而不是疾病本身<ref name="pmid10653284"/>。 |
|||
2009年,類澱粉胜肽假說有了新的發展,新的研究指出和Aβ關係密切的蛋白質可能才是阿茲海默症的罪魁禍首。此類與類澱粉斑塊相關的機制會在早年快速發育的時期,使腦部神經元間的連結減少,並在年紀較大後受到老化相關過程的刺激,導致阿茲海默症中的神經元退化<ref name="Nikolaev">{{vcite journal|vauthors=Nikolaev A|author2=McLaughlin T|author3=O'Leary DD|author4={{tsl|en|Marc Tessier-Lavigne||Tessier-Lavigne M}}|title=APP Binds DR6 to Cause Axon Pruning and Neuron Death via Distinct Caspases|journal=Nature|volume=457|issue=7232|pages=981–89|date=19 February 2009|pmid=19225519|pmc=2677572|doi=10.1038/nature07767|issn=0028-0836}}</ref>。該研究發現APP是DR6的一個[[配體 (生物化學)|配體]],{{tsl|en|beta-secretase|β-secretase|β-secretase}}會切下的APP的[[胺基端|N端]]片段產生N-APP(同樣的酵素也參與APP修飾為Aβ的過程),N-APP則會與死亡受體6(death receptor 6,DR6,或稱{{tsl|en|TNFRSF21||TNFRSF21}})結合,啟動[[细胞凋亡|細胞凋亡]]途徑。DR6在阿茲海默症患者受影響的腦區中有高量的表現,因此在{{tsl|en|ageing brain|大腦老化|老化的大腦}}中,可能就是N-APP/DR6途徑被活化而造成了神經元損傷<ref name="Nikolaev" />。N-APP/DR6途徑所啟動的細胞凋亡包含了神經細胞本體和軸突,不同於一般細胞凋亡的機制需要活化caspase-3,[[轴突|軸突]]的退化需要活化caspase-6。此外,經由caspase-6路徑所啟動的細胞凋亡,也可能和另一種[[亨丁頓舞蹈症|杭廷頓舞蹈症]]相關<ref>{{Cite journal|title=Cleavage at the caspase-6 site is required for neuronal dysfunction and degeneration due to mutant huntingtin|url=https://www.ncbi.nlm.nih.gov/pubmed/16777606|last=Graham|first=Rona K.|last2=Deng|first2=Yu|date=2006-06-16|journal=Cell|issue=6|doi=10.1016/j.cell.2006.04.026|volume=125|pages=1179–1191|issn=0092-8674|pmid=16777606|last3=Slow|first3=Elizabeth J.|last4=Haigh|first4=Brendan|last5=Bissada|first5=Nagat|last6=Lu|first6=Ge|last7=Pearson|first7=Jacqueline|last8=Shehadeh|first8=Jacqueline|last9=Bertram|first9=Lisa}}</ref>。2017年,β-secretase抑制劑{{tsl|en|verubecestat||verubecestat}}的臨床試驗因為被認為對臨床沒有助益而遭到中止<ref name="EPOCHStreet">{{Cite web |url=https://www.thestreet.com/story/14002423/1/merck-alzheimer-s-drug-study-halted-early-for-futility.html |title="Merck Alzheimer's Drug Study Halted Early for Futility" |last=Feuerstein |first=Adam |date=14 February 2017 |publisher=TheStreet, Inc. |location=New York City, NY, USA |deadurl=no |archive-url=https://web.archive.org/web/20170216062344/https://www.thestreet.com/story/14002423/1/merck-alzheimer-s-drug-study-halted-early-for-futility.html |archive-date=16 February 2017 }}Merck Alzheimer's Drug Study Halted Early for Futility Independent study monitors concluded that there was "virtually no chance of finding a positive clinical effect."</ref>。 |
|||
===Tau蛋白假說=== |
|||
[[File:TANGLES HIGH.jpg|upright=1.35|thumb|阿海海默症中,[[Tau蛋白]]異常會造成腦細胞內的微管瓦解。]] |
|||
[[Tau蛋白]]假說認為Tau蛋白異常是引起阿茲海默症病情發展的主因<ref name="pmid11801334" />。在這個模型中,{{tsl|en|hyperphosphorylated|過度磷酸化|過度磷酸化}}的Tau蛋白會開始與其他Tau蛋白質配對結合,結果在神經細胞中形成了{{tsl|en|neurofibrillary tangle|神經纖維糾結|神經纖維糾結}}<ref name="pmid1669718">{{vcite journal|vauthorv=Goedert M, Spillantini MG, Crowther RA|title=Tau Proteins and Neurofibrillary Degeneration|journal=Brain Pathology|volume=1|issue=4|pages=279–86|year=1991|pmid=1669718|doi=10.1111/j.1750-3639.1991.tb00671.x|month=July}}</ref>。在這種情形下,神經細胞內的[[微管]]開始瓦解並導致由[[细胞骨架|細胞骨架]]構成的運送系統崩壞<ref name="pmid15615638">{{vcite journal|vauthors=Iqbal K, Alonso Adel C, Chen S|title=Tau Pathology in Alzheimer Disease and Other Tauopathies|journal=Biochimica et Biophysica Acta|volume=1739|issue=2–3|pages=198–210|year=2005|pmid=15615638|doi=10.1016/j.bbadis.2004.09.008|month=January}}</ref>,這將造成神經細胞之間的化學訊息溝通失效,接著導致神經細胞死亡<ref name="pmid17127334">{{vcite journal|vauthors=Chun W, Johnson GV|title=The Role of Tau Phosphorylation and Cleavage in Neuronal Cell Death|journal=Frontiers in Bioscience|volume=12|pages=733–56|year=2007|pmid=17127334|doi=10.2741/2097}}</ref>。 |
|||
===其他假說=== |
|||
新生血管假說認為[[血腦屏障]]功能減低也可能和阿茲海默症有關<ref>{{cite journal | vauthors = Deane R, Zlokovic BV | title = Role of the blood-brain barrier in the pathogenesis of Alzheimer's disease | journal = Current Alzheimer Research | volume = 4 | issue = 2 | pages = 191–7 | date = April 2007 | pmid = 17430246 | doi = 10.2174/156720507780362245 }}</ref>。 |
|||
阿茲海默症患者細胞內外{{tsl|en|biometal (biology)|生物金屬|金屬離子}}(如銅、鐵、鋅離子)會不[[稳态|平衡]],雖然目前不清楚是蛋白質的改變造成離子不平衡,抑或離子的改變造成蛋白質的變化,這些離子會影響tau蛋白、APP和APOE<ref name="pmid24971061">{{vcite journal |journal=Frontiers in Aging Neuroscience |date=12 June 2014 |volume=6|page=121 |title=Interactions of metals and Apolipoprotein E in Alzheimer's disease |vauthors =Xu H, Finkelstein DI, Adlard PA |pmid=24971061 |pmc=4054654 |doi=10.3389/fnagi.2014.00121 |quote=Although we still do not know if the metal ion dyshomeostasis present in AD is a cause or consequence of the disease, there is a growing body of evidence showing a direct correlation between metal ions and key AD-related key proteins.}}</ref>,這些蛋白失調會造成細胞內部的[[氧化应激|氧化壓力]],並因此造成相關的病變<ref>{{vcite journal | vauthors = Su B, Wang X, Nunomura A | title = Oxidative Stress Signaling in Alzheimer's Disease | journal = Current Alzheimer Research | volume = 5 | issue = 6 | pages = 525–32 | date = December 2008 | pmid = 19075578 | pmc = 2780015 | doi = 10.2174/156720508786898451 }}</ref><ref>{{vcite journal | vauthors = Kastenholz B, Garfin DE, Horst J, Nagel KA | title = Plant Metal Chaperones: A Novel Perspective in Dementia Therapy | journal = Amyloid | volume = 16 | issue = 2 | pages = 81–83 | year = 2009 | pmid = 20536399 | doi = 10.1080/13506120902879392 }}</ref><ref> |
|||
{{cite web |title=Aluminium and Alzheimer's disease |publisher=Alzheimer's Society |work=Facts about dementia |url=http://www.alzheimers.org.uk/Facts_about_dementia/Risk_factors/info_aluminium.htm |access-date=14 October 2005 |deadurl=yes |archive-url=https://web.archive.org/web/20051027165732/http://www.alzheimers.org.uk/Facts_about_dementia/Risk_factors/info_aluminium.htm |archive-date=27 October 2005 }} |
|||
</ref><ref>{{cite journal | vauthors = Bondy SC | title = Low levels of aluminum can lead to behavioral and morphological changes associated with Alzheimer's disease and age-related neurodegeneration | journal = Neurotoxicology | volume = 52 | pages = 222–9 | date = January 2016 | pmid = 26687397 | doi = 10.1016/j.neuro.2015.12.002 }}</ref><ref>{{cite journal | vauthors = Kandimalla R, Vallamkondu J, Corgiat EB, Gill KD | title = Understanding Aspects of Aluminum Exposure in Alzheimer's Disease Development | journal = Brain Pathology | volume = 26 | issue = 2 | pages = 139–54 | date = March 2016 | pmid = 26494454 | doi = 10.1111/bpa.12333 }}</ref>。然而有些相關研究的品質受到批評<ref>{{vcite journal | vauthors = Santibáñez M, Bolumar F, García AM | title = Occupational Risk Factors in Alzheimer's Disease: A Review Assessing the Quality of Published Epidemiological Studies | journal = {{tsl|en|Occupational and Environmental Medicine||Occupational and Environmental Medicine}} | volume = 64 | issue = 11 | pages = 723–32 | year = 2007 | pmid = 17525096 | pmc = 2078415 | doi = 10.1136/oem.2006.028209 }}</ref><ref name="Is the Aluminum Hypothesis dead">{{cite journal | vauthors = Lidsky TI | title = Is the Aluminum Hypothesis dead? | journal = Journal of Occupational and Environmental Medicine | volume = 56 | issue = 5 Suppl | pages = S73-9 | date = May 2014 | pmid = 24806729 | pmc = 4131942 | doi = 10.1097/jom.0000000000000063 }}</ref>,因此這種推論仍有爭議<ref>{{cite journal | vauthors = Yegambaram M, Manivannan B, Beach TG, Halden RU | title = Role of environmental contaminants in the etiology of Alzheimer's disease: a review | journal = Current Alzheimer Research | volume = 12 | issue = 2 | pages = 116–46 | date = 2015 | pmid = 25654508 | pmc = 4428475 | doi = 10.2174/1567205012666150204121719 }}</ref>。多數的研究者並不支持鋁離子和阿茲海默症有因果關係<ref name="Is the Aluminum Hypothesis dead"/>。 |
|||
抽菸是阿茲海默症的顯著危險因子<ref>{{vcite journal | vauthors = Cataldo JK, Prochaska JJ, Glantz SA | title = Cigarette smoking is a risk factor for Alzheimer's disease: An analysis controlling for tobacco industry affiliation | journal = Journal of Alzheimer's Disease | volume = 19 | issue = 2 | pages = 465–80 | year = 2010 | pmid = 20110594 | pmc = 2906761 | doi = 10.3233/JAD-2010-1240 }}</ref>, [[先天免疫系統]]的[[炎症|發炎指標]]則是遲發型阿茲海默症的危險因子<ref>{{vcite journal | vauthors = Eikelenboom P, van Exel E, Hoozemans JJ, Veerhuis R, Rozemuller AJ, van Gool WA | title = Neuroinflammation – An Early Event in Both the History and Pathogenesis of Alzheimer's Disease | journal = Neuro-Degenerative Diseases | volume = 7 | issue = 1–3 | pages = 38–41 | year = 2010 | pmid = 20160456 | doi = 10.1159/000283480 }}</ref>。有限的證據指出[[空氣污染]]可能也是促進阿茲海默症發展的一項因素<ref>{{vcite journal | vauthors = Moulton PV, Yang W | title = Air Pollution, Oxidative Stress, and Alzheimer's Disease | journal = Journal of Environmental and Public Health | volume = 2012 | page = 472751 | year = 2012 | pmid = 22523504 | doi = 10.1155/2012/472751 | type = Review | pmc=3317180}}</ref>。 |
|||
[[牙周炎]]發生時的{{tsl|en|Spirochaete|螺旋體|}}感染也可能造成[[失智症|失智]],並參與阿茲海默症的{{tsl|en|pathogenesis|病理機制|}} <ref>{{cite journal | vauthors = Miklossy J | title = Alzheimer's disease – a neurospirochetosis. Analysis of the evidence following Koch's and Hill's criteria | journal = Journal of Neuroinflammation | volume = 8 | issue = 1 | pages = 90 | date = August 2011 | pmid = 21816039 | pmc = 3171359 | doi = 10.1186/1742-2094-8-90 }}</ref>。真菌感染也是一個可能的疾病機轉<ref>{{cite journal | vauthors = Pisa D, Alonso R, Rábano A, Rodal I, Carrasco L | title = Different Brain Regions are Infected with Fungi in Alzheimer's Disease | language = En | journal = Scientific Reports | volume = 5 | issue = 1 | pages = 15015 | date = October 2015 | pmid = 26468932 | pmc = 4606562 | doi = 10.1038/srep15015 | url = http://www.nature.com/articles/srep15015 }}</ref>。 |
|||
也有假說認為 [[寡突膠質細胞|寡突膠細胞]]功能異常以及其在老化過程中產生的髓鞘問題會造成軸突的傷害,最後導致了類澱粉生成和tau蛋白過磷酸化的副作用<ref>{{cite journal | vauthors = Bartzokis G | title = Alzheimer's disease as homeostatic responses to age-related myelin breakdown | journal = Neurobiology of Aging | volume = 32 | issue = 8 | pages = 1341–71 | date = August 2011 | pmid = 19775776 | pmc = 3128664 | doi = 10.1016/j.neurobiolaging.2009.08.007 }}</ref><ref>{{cite journal | vauthors = Cai Z, Xiao M | title = Oligodendrocytes and Alzheimer's disease | journal = The International Journal of Neuroscience | volume = 126 | issue = 2 | pages = 97–104 | date = 2016 | pmid = 26000818 | doi = 10.3109/00207454.2015.1025778 }}</ref>。 |
|||
逆生假說(Retrogenesis)是貝里·萊斯伯格(Barry Reisberg)在1980年代提出的另一項阿茲海默症假說<ref name=Kluger1999 />。胎兒發育時會歷經一連串的[[神经发生|神經發生]],這個過程始於{{tsl|en|neurulation|神經板形成|}},終於[[髓磷脂|髓鞘]]形成,該假說認為阿茲海默症患者的[[神經退化]]就如同此一過程的逆轉,先是{{tsl|en|demyelination|神經脫鞘|}}、白質的軸突死亡、最後灰質的神經元死亡<ref name=Laks2015>{{cite journal | vauthors = Alves GS, Oertel Knöchel V, Knöchel C, Carvalho AF, Pantel J, Engelhardt E, Laks J | title = Integrating retrogenesis theory to Alzheimer's disease pathology: insight from DTI-TBSS investigation of the white matter microstructural integrity | journal = BioMed Research International | volume = 2015 | pages = 291658 | date = 2015 | pmid = 25685779 | pmc = 4320890 | doi = 10.1155/2015/291658 }}</ref>。同樣地,嬰兒會經歷{{tsl|en|cognitive development|認知發展|}},該假說也認為阿茲海默症患者的[[認知障礙症|認知障礙]]就如同此一過程的倒轉<ref name=Kluger1999>{{cite journal | vauthors = Reisberg B, Franssen EH, Hasan SM, Monteiro I, Boksay I, Souren LE, Kenowsky S, Auer SR, Elahi S, Kluger A | title = Retrogenesis: clinical, physiologic, and pathologic mechanisms in brain aging, Alzheimer's and other dementing processes | journal = European Archives of Psychiatry and Clinical Neuroscience | volume = 249 Suppl 3 | issue = 3 | pages = 28–36 | date = 1999 | pmid = 10654097 | doi = 10.1007/pl00014170 | url = http://ncbi.nlm.nih.gov/pubmed/10654097 | archive-url = https://web.archive.org/web/20160919045628/http://www.ncbi.nlm.nih.gov/pubmed/10654097 | df = dmy-all | deadurl = no | archive-date = 19 September 2016 }}</ref>。萊斯伯格也發展出了一套稱為FAST(功能性評估分級工具,Functional Assessment Staging Tool)的照護評估工具,用以評估阿茲海默患者的病程發展到哪個階段,以此為依據為每個階段的患者提供適當的照護建議<ref name=Kluger1999 /><ref name=Carson2015>{{cite book|last1=Brenner Carson|first1=Verna|title=Caregiving for Alzheimer's Disease|date=2015|publisher=Springer New York Academy of Sciences|location=New York|isbn=978-1-4939-2406-6|pages=1–9}}</ref>。 |
|||
==病生理學== |
|||
[[File:Alzheimer dementia (3) presenile onset.jpg|thumb|早發性阿茲海默症患者的大腦皮質顯微影像,{{tsl|en|Histopathology|組織病理學|}}可見組織內有老年斑塊(senile plaques),銀染法。]] |
|||
[[File:Alzheimer's Disease.gif|thumb|阿茲海默症患者與正常人的腦皮質比較,患者顳葉、頂葉,及部分扣帶回中的溝回會消失。]] |
|||
==病理生理學== |
|||
:主条目:{{link-en|阿茲海默症病理生理學|Biochemistry of Alzheimer's disease}} |
|||
[[File:Alzheimers brain.jpg|thumb|210px|正常腦(左)與嚴重阿茲海默症的腦萎縮(右)相比較。]] |
|||
[[File:Alzheimer's Disease.gif|thumb|210px|阿茲海默症[[皮質]]萎縮,與[[顳葉]]、[[頂葉]]、[[額葉]]皮質和部分扣帶回,相關的[[腦回]]和[[腦溝]]損失。]] |
|||
[[File:Blausen 0017 AlzheimersDisease.png|thumb|阿茲海默症相關的神經元變性]] |
|||
[[File:Alzheimer dementia (3) presenile onset.jpg|thumb|這張組織病理學影像顯示一位早老性阿茲海默症病患大腦皮質中的老年瘢塊,銀染色法]] |
|||
===神經病理學=== |
===神經病理學=== |
||
阿茲海默症的特徵是損失[[大腦皮質]]和一些皮質下區域的[[神經元]]和[[突触]],損失神經元和突觸導致受影響區域過多的[[萎縮]],包括[[颞叶]]、[[顶叶]]、一部份的[[額葉]]和[[扣帶皮層]]<ref name="pmid12934968"/>,學者利用[[核磁共振成像|磁振造影]]和[[正电子发射计算机断层扫描|正子電腦斷層掃瞄]]紀錄阿茲海默症病患在疾病進展中的大腦影像,並與健康老年人的相同影像作比較,結果在大腦的特殊區域發現大腦質量退化<ref name="pmid19460794">{{cite journal |accessdate=2013-01-07 |language=en |author=Desikan RS |coauthors=Cabral HJ, Hess CP, Dillon WP, Glastonbury CM, Weiner MW, Schmansky NJ, Greve DN, Salat DH, Buckner RL, Fischl B; Alzheimer's Disease Neuroimaging Initiative |title=Automated MRI measures identify individuals with mild cognitive impairment and Alzheimer's disease |journal=Brain |volume=132 |issue=8 |pages=2048–57 |pmid=19460794 |pmc=2714061 |doi=10.1093/brain/awp123 |url=|date=August 2009}}</ref><ref name="Rebekah Moan">{{cite web |accessdate=2013-01-07 |language=en |url=http://www.diagnosticimaging.com/news/display/article/113619/1428344 |title=MRI software accurately IDs preclinical Alzheimer's disease |author=Moan R |publisher=Diagnostic Imaging |date=2009-07-20 |deadurl=yes |archiveurl=http://arquivo.pt/wayback/20160516192841/http://www.diagnosticimaging.com/news/display/article/113619/1428344 |archivedate=2016-05-16 }}</ref>。 |
|||
阿茲海默症的特徵是[[大腦皮質]]及特定皮質下區域的[[神經元]]和[[突触]]喪失。神經元喪失過多的區域甚至會導致巨觀解剖上的[[萎縮]],常見主要遭到的進犯部位包含[[颞叶]]、[[顶叶]]、一部份的[[額葉]],和[[扣带皮层|扣帶回]]<ref name="pmid12934968" />。某些腦幹的核區可能也會受到影響,如[[蓝斑核]]等<ref>{{vcite journal|vauthors=Braak H, Del Tredici K|title=Where, when, and in what form does sporadic Alzheimer's disease begin?|journal=Current Opinion in Neurology|volume=25|issue=Pt 6|pages=708–14|date=December 2012|pmid=23160422|doi=10.1097/WCO.0b013e32835a3432}}</ref>。[[核磁共振成像|磁振造影]](MRI)和[[正电子发射计算机断层扫描|正子電腦斷層掃瞄]](PET)研究已報導患者在疾病進程中部分腦區萎縮的狀況,且跟其他健康老年人比較也能發現有部分腦區萎縮<ref>{{vcite journal|vauthors=Desikan RS, Cabral HJ, Hess CP|title=Automated MRI Measures Identify Individuals with Mild Cognitive Impairment and Alzheimer's Disease|journal=Brain|volume=132|issue=Pt 8|pages=2048–57|date=August 2009|pmid=19460794|pmc=2714061|doi=10.1093/brain/awp123}}</ref><ref>{{vcite journal|author=Moan R|title=MRI Software Accurately IDs Preclinical Alzheimer's Disease|journal=Diagnostic Imaging|date=20 July 2009|url=http://www.diagnosticimaging.com/news/display/article/113619/1428344|archive-url=http://arquivo.pt/wayback/20160516192841/http://www.diagnosticimaging.com/news/display/article/113619/1428344|dead-url=yes|archive-date=16 May 2016|accessdate=7 January 2013|archiveurl=http://arquivo.pt/wayback/20160516192841/http://www.diagnosticimaging.com/news/display/article/113619/1428344|archivedate=16 May 2016|deadurl=yes}}</ref>。 |
|||
在顯微鏡下,阿茲海默症病患大腦中的β淀粉样斑块和神經纖維缠結都清楚可見<ref name="pmid15184601">{{cite journal |accessdate=2013-01-10 |language=en |author=Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J |title=The importance of neuritic plaques and tangles to the development and evolution of AD |journal=Neurology |volume=62 |issue=11 |pages=1984–9 |pmid=15184601|date=June 2004}}</ref>,蛋白質斑是高密度不溶於水的β類澱粉样蛋白質和細胞內容物在神經細胞周圍堆積形成,神經纖維缠結則是由微管相關蛋白質Tau蛋白質過度磷酸化並且堆積在細胞內聚集而成,雖然許多老年人都會因為老化而在大腦出現蛋白質斑和神經纖維缠結,相比之下,阿茲海默症病患在大腦中的特殊區域如顳葉有更多這些病變<ref name="pmid8038565">{{cite journal |accessdate=2013-01-10 |language=en |author=Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH |title=Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital |journal=Cereb. Cortex |volume=4 |issue=2 |pages=138–50 |year=1994 |pmid=8038565 |doi=10.1093/cercor/4.2.138}}</ref>,{{link-en|路易體|Lewy body}}在病患腦中也很常見<ref name="pmid11816795">{{cite journal |accessdate=2013-01-10 |language=en |author=Kotzbauer PT, Trojanowsk JQ, Lee VM |title=Lewy body pathology in Alzheimer's disease |journal=J Mol Neurosci |volume=17 |issue=2 |pages=225–32 |pmid=11816795 |doi=10.1385/JMN:17:2:225 |
|||
|date=Oct 2001}}</ref>。 |
|||
在顯微鏡下,阿茲海默症患者的腦皮質可以看到明顯的[[類澱粉蛋白|類澱粉斑塊]]以及{{tsl|en|neurofibrillary tangle|神經元纖維纏結|}}<ref name="pmid15184601">{{vcite journal|vauthors=Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J|title=The Importance of Neuritic Plaques and Tangles to the Development and Evolution of AD|journal=Neurology|volume=62|issue=11|pages=1984–89|year=2004|pmid=15184601|doi=10.1212/01.WNL.0000129697.01779.0A|month=June}}</ref>。斑塊大多由緻密且[[溶解性|不溶於水]]的{{tsl|en|beta-amyloid|β類澱粉|}}樣胜肽及細胞衍生物所構成,通常堆積於神經元周圍。神經纖維纏結則通常是由微管相關蛋白質Tau所構成,患者的[[Tau蛋白]]會過度磷酸化並聚集於細胞內。雖然許多老年人的大腦中都可發現這些因老化形成的斑塊和纏結,但阿茲海默症患者會在特定腦區出現更多斑塊及纏結,例如顳葉等<ref name="pmid8038565">{{vcite journal|vauthors=Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH|title=Regional Distribution of Neurofibrillary Tangles and Senile Plaques in the Cerebral Cortex of Elderly Patients: A Quantitative Evaluation of a One-year Autopsy Population from a Geriatric Hospital|journal=Cerebral Cortex|volume=4|issue=2|pages=138–50|year=1994|pmid=8038565|doi=10.1093/cercor/4.2.138}}</ref>。{{link-en|路易氏體|Lewy body}}在病患腦中也很常見<ref name="pmid11816795">{{vcite journal|vauthors=Kotzbauer PT, Trojanowsk JQ, Lee VM|title=Lewy Body Pathology in Alzheimer's Disease|journal=Journal of Molecular Neuroscience|volume=17|issue=2|pages=225–32|year=2001|pmid=11816795|doi=10.1385/JMN:17:2:225|month=Oct}}</ref>。 |
|||
===生物化學=== |
===生物化學=== |
||
{{Multiple image|footer = 酵素將前類澱粉蛋白(APP,圖中以藍色表示)降解之後,會形成蛋白片段,其中某一段即為β類澱粉蛋白質(A<sub>β</sub>圖中以黃色表示)。A<sub>β</sub>與阿茲海默症的形成有重要關聯。|image1 = Amyloid 01big1.jpg|image2 = Amyloid 02big1.jpg|image3 = Amyloid 03big1.jpg}} |
|||
[[File:Amyloid-plaque formation-big.jpg|300px|thumb|border|APP(amyloid precursor protein)被酵素切成碎片,其中β片段是阿茲海默症中產生老年瘢塊的重要成份。]] |
|||
阿茲海默症也被視為一種[[蛋白质折叠|蛋白質折疊錯誤]]的疾病([[蛋白质构象病]]),是由於大腦中折疊異常的β類澱粉蛋白質和Tau蛋白質堆積而造成<ref name="pmid14528050">{{cite journal |accessdate=2013-01-13 |language=en |
|||
|author=Hashimoto M, Rockenstein E, Crews L, Masliah E |title=Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer's and Parkinson's diseases |journal=Neuromolecular Med. |volume=4 |issue=1–2 |pages=21–36 |year=2003 |pmid=14528050 |doi=10.1385/NMM:4:1-2:21}}</ref>。老年瘢塊是由長度約39—43個[[氨基酸]]名為{{le|β類澱粉蛋白質|Amyloid beta}}的小[[肽]]形成,β類澱粉蛋白質則是一個叫做前類澱粉蛋白質(APP)的較大蛋白質的片段,APP是一個穿過神經細胞膜的[[跨膜蛋白|跨膜蛋白質]],對於神經元的生長、存活和受傷後的修復非常重要 |
|||
<ref name="pmid16822978">{{cite journal |accessdate=2013-01-13 |language=en |author=Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J |title=Synapse formation and function is modulated by the amyloid precursor protein |journal=J. Neurosci. |volume=26 |issue=27 |pages=7212–21 |pmid=16822978 |doi=10.1523/JNEUROSCI.1450-06.2006|date=July 2006}}</ref><ref name="pmid12927332">{{cite journal |accessdate=2013-01-13 |language=en |author=Turner PR, O'Connor K, Tate WP, Abraham WC |title=Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory |journal=Prog. Neurobiol. |volume=70 |issue=1 |pages=1–32 |pmid=12927332 |doi=10.1016/S0301-0082(03)00089-3|date=May 2003}}</ref>。在阿茲海默症中,有個尚未釐清的機制導致APP被酵素切成幾個較小的片段<ref name="pmid15787600">{{cite journal |accessdate=2013-01-21 |language=en |author=Hooper NM |title=Roles of proteolysis and lipid rafts in the processing of the amyloid precursor protein and prion protein |journal=Biochem. Soc. Trans. |volume=33 |issue=Pt 2 |pages=335–8 |pmid=15787600 |doi=10.1042/BST0330335|date=April 2005}}</ref>,其中一個片段使纖維和β類澱粉蛋白質增加,導致神經元外開始形成稱為老年瘢塊的團塊堆積<ref name="pmid15184601"/><ref name="pmid15004691">{{cite journal |accessdate=2013-01-21 |language=en |author=Ohnishi S, Takano K |title=Amyloid fibrils from the viewpoint of protein folding |journal=Cell. Mol. Life Sci. |volume=61 |issue=5 |pages=511–24 |pmid=15004691 |doi=10.1007/s00018-003-3264-8|date=March 2004}}</ref>。 |
|||
[[File:TANGLES HIGH.jpg|300px|thumb|在阿茲海默症病患大腦細胞中,Tau蛋白質的改變導致微小管解離。]] |
|||
阿茲海默症也被視為一種[[蛋白质折叠|蛋白質折疊錯誤]]的疾病([[蛋白质构象病]]),是由於大腦中折疊異常的{{tsl|en|amyloid beta|β類澱粉蛋白|}}和Tau蛋白質堆積而造成<ref name="pmid14528050">{{vcite journal|vauthors=Hashimoto M, Rockenstein E, Crews L, Masliah E|title=Role of Protein Aggregation in Mitochondrial Dysfunction and Neurodegeneration in Alzheimer's and Parkinson's Diseases|journal=Neuromolecular Medicine|volume=4|issue=1–2|pages=21–36|year=2003|pmid=14528050|doi=10.1385/NMM:4:1-2:21}}</ref>。構成斑塊的{{le|β類澱粉蛋白質|Amyloid beta}}(A<sub>β</sub>)是由約39至43個[[氨基酸]]構成的短鏈胜肽。A<sub>β</sub>為[[前類澱粉蛋白質|前類澱粉蛋白]](APP)的一小片段,該蛋白為神經元細胞膜上的一種[[跨膜蛋白]],對神經元的生長、存活和受傷後的修復非常重要<ref name="pmid16822978">{{vcite journal|vauthors=Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J|title=Synapse Formation and Function is Modulated by the Amyloid Precursor Protein|journal=The Journal of Neuroscience|volume=26|issue=27|pages=7212–21|year=2006|pmid=16822978|doi=10.1523/JNEUROSCI.1450-06.2006|month=July}}</ref><ref name="pmid12927332">{{vcite journal|vauthors=Turner PR, O'Connor K, Tate WP, Abraham WC|title=Roles of Amyloid Precursor Protein and its Fragments in Regulating Neural Activity, Plasticity and Memory|journal=Progress in Neurobiology|volume=70|issue=1|pages=1–32|year=2003|pmid=12927332|doi=10.1016/S0301-0082(03)00089-3|month=May}}</ref>。阿茲海默症患者的{{tsl|en|gamma secretase|γ分泌酶|}}及{{tsl|en|beta-secretase 1|β分泌酶|}}會共同進行[[蛋白酶解]]作用,將APP切成小片段<ref name="pmid15787600">{{vcite journal|vauthors=Hooper NM|title=Roles of Proteolysis and Lipid Rafts in the Processing of the Amyloid Precursor Protein and Prion Protein|journal=Biochemical Society Transactions|volume=33|issue=Pt 2|pages=335–38|year=2005|pmid=15787600|doi=10.1042/BST0330335|month=April}}</ref>。其中某些片段即為β類澱粉蛋白,他們會在神經元的胞外間質堆積,形成[[老年斑|老年斑塊]]<ref name="pmid15184601" /><ref name="pmid15004691">{{vcite journal|vauthors=Ohnishi S, Takano K|title=Amyloid Fibrils from the Viewpoint of Protein Folding|journal=Cellular and Molecular Life Sciences|volume=61|issue=5|pages=511–24|year=2004|pmid=15004691|doi=10.1007/s00018-003-3264-8|month=March}}</ref>。 |
|||
還有一種理論認為阿茲海默症是{{link-en|Tau蛋白質異常沉積|Tauopathy}}造成,每個神經元都有由[[微管]]組成的細胞內支撐系統,稱為[[細胞骨架]],這些微管的作用如同軌道,引導營養物質和其他分子在細胞本體和[[軸突]]之間來回移動。Tau蛋白質被[[磷酸化]]之後可以穩定微管,所以被歸類為{{link-en|微管關連蛋白質|microtubule-associated protein}}。在阿茲海默症病患中,Tau蛋白質發生了一些化學變化,變得{{link-en|過度磷酸化|Hyperphosphorylation}},接著就與其他蛋白質配對結合,產生神經纖維團塊並且瓦解神經元的運輸系統<ref name="pmid17604998">{{cite journal |accessdate=2013-01-25 |language=en |author=Hernández F, Avila J |title=Tauopathies |journal=Cell. Mol. Life Sci. |volume=64 |issue=17 |pages=2219–33 |pmid=17604998 |doi=10.1007/s00018-007-7220-x|date=September 2007}}</ref>。 |
|||
還有一種理論認為阿茲海默症是{{link-en|Tau蛋白質異常沉積|Tauopathy}}造成。每個神經元都有由[[微管]]組成的細胞內支撐系統,稱為[[細胞骨架]],這些微管的作用如同軌道,引導營養物質和其他分子在細胞本體和[[軸突]]之間來回移動。Tau蛋白質被[[磷酸化]]之後可以穩定微管,所以被歸類為{{link-en|微管關聯蛋白質|microtubule-associated protein}}<ref name="pmid17604998">{{vcite journal|vauthors=Hernández F, Avila J|title=Tauopathies|journal=Cellular and Molecular Life Sciences|volume=64|issue=17|pages=2219–33|year=2007|pmid=17604998|doi=10.1007/s00018-007-7220-x|month=September}}</ref>。在阿茲海默症病患中,Tau蛋白質發生突變而{{link-en|過度磷酸化|Hyperphosphorylation}},進而造成微管瓦解。釋出的Tau蛋白質會聚集起來,產生神經纖維團塊並且瓦解神經元的運輸系統<ref>{{Cite journal|title=Tau Protein Hyperphosphorylation and Aggregation in Alzheimer’s Disease and Other Tauopathies, and Possible Neuroprotective Strategies|author=|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4808800/|last=Šimić|first=Goran|last2=Babić Leko|first2=Mirjana|date=2016-01-06|journal=Biomolecules|issue=1|doi=10.3390/biom6010006|others=|year=|volume=6|page=|issn=2218-273X|pmc=4808800|pmid=26751493|last3=Wray|first3=Selina|last4=Harrington|first4=Charles|last5=Delalle|first5=Ivana|last6=Jovanov-Milošević|first6=Nataša|last7=Bažadona|first7=Danira|last8=Buée|first8=Luc|last9=de Silva|first9=Rohan}}</ref>。</ref> Pathogenic tau can also cause neuronal death through [[转座子|transposable element]] dysregulation.<ref>{{cite journal |last1=Sun |first1=Wenyan |last2=Samimi |first2=Hanie |last3=Gamez |first3=Maria |last4=Zare |first4=Habil |last5=Frost |first5=Bess |title=Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies |journal=Nature Neuroscience |date=23 July 2018 |volume=21 |issue=8 |pages=1038–48 |doi=10.1038/s41593-018-0194-1|pmid=30038280 |pmc=6095477 }}</ref> |
|||
===疾病機制=== |
|||
目前仍不清楚β類澱粉蛋白質的異常合成與異常聚集如何導致阿茲海默症的病理變化<ref name="pmid17622778">{{cite journal |accessdate=2013-02-04 |language=en |author=Van Broeck B, Van Broeckhoven C, Kumar-Singh S |title=Current insights into molecular mechanisms of Alzheimer disease and their implications for therapeutic approaches |journal=Neurodegener Dis |volume=4 |issue=5 |pages=349–65 |year=2007 |pmid=17622778 |doi=10.1159/000105156}}</ref>,類澱粉蛋白質假說指出β類澱粉蛋白質是刺激神經元退化的主要角色,類澱粉蛋白質聚集成的纖維是有毒的蛋白質構造且會摧毀細胞的鈣離子平衡,大量堆積類澱粉蛋白質纖維則會刺激細胞進行[[細胞凋亡]]<ref name="pmid2218531">{{cite journal |accessdate=2013-02-04 |language=en |author=Yankner BA, Duffy LK, Kirschner DA |title=Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides |journal=Science |volume=250 |issue=4978 |pages=279–82 |pmid=2218531 |doi=10.1126/science.2218531|date=October 1990}}</ref>,β類澱粉蛋白質也會選擇性地在阿茲海默症病灶處細胞的[[线粒体]]中堆積,並且抑制神經元使用[[葡萄糖]],也會抑制許多酵素的功能<ref name="pmid17424907">{{cite journal |accessdate=2013-02-04 |language=en |author=Chen X, Yan SD |title=Mitochondrial Abeta: a potential cause of metabolic dysfunction in Alzheimer's disease |journal=IUBMB Life |volume=58 |issue=12 |pages=686–94 |pmid=17424907 |doi=10.1080/15216540601047767|date=December 2006}}</ref>。 |
|||
===疾病機轉=== |
|||
不同的發炎過程和[[細胞激素]]也可能在阿茲海默症的病理變化中扮演一定的角色,[[發炎]]是組織受傷的一般標記,也可能是免疫反應的標記<ref name="pmid15681814">{{cite journal |accessdate=2013-02-04 |language=en |author=Greig NH |title=New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists |journal=Ann. N. Y. Acad. Sci. |volume=1035 |pages=290–315 |pmid=15681814 |doi=10.1196/annals.1332.018 |author2=Mattson MP |author3=Perry T |display-authors=3 |last4=Chan |first4=SL |last5=Giordano |first5=T |last6=Sambamurti |first6=K |last7=Rogers |first7=JT |last8=Ovadia |first8=H |last9=Lahiri |first9=DK|date=December 2004}}</ref>。 |
|||
目前仍不清楚A<sub>β</sub>蛋白的異常合成與異常聚集,如何導致阿茲海默症的病理變化<ref name="pmid17622778">{{vcite journal|vauthors=Van Broeck B, Van Broeckhoven C, Kumar-Singh S|title=Current Insights into Molecular Mechanisms of Alzheimer Disease and Their Implications for Therapeutic Approaches|journal=Neuro-Degenerative Diseases|volume=4|issue=5|pages=349–65|year=2007|pmid=17622778|doi=10.1159/000105156}}</ref><ref>{{vcite journal|vauthors=Huang Y, Mucke L|title=Alzheimer Mechanisms and Therapeutic strategies|journal=Cell|volume=148|issue=6|pages=1204–22|year=2012|pmid=22424230|doi=10.1016/j.cell.2012.02.040|pmc=3319071}}</ref>。類澱粉蛋白假說指出A<sub>β</sub>蛋白的堆積是造成神經元退化的主要原因,聚集的類澱粉蛋白纖維會瓦解細胞的鈣離子平衡,並造成[[細胞凋亡]]<ref name="pmid2218531">{{vcite journal|vauthors=Yankner BA, Duffy LK, Kirschner DA|title=Neurotrophic and Neurotoxic Effects of Amyloid Beta Protein: Reversal by Tachykinin Neuropeptides|journal=Science|volume=250|issue=4978|pages=279–82|year=1990|pmid=2218531|doi=10.1126/science.2218531|month=October}}</ref>。A<sub>β</sub>蛋白也會選擇性地堆積於病灶處細胞的[[线粒体]]中,抑制部分酵素的功能以及神經元使用[[葡萄糖]]的能力<ref name="pmid17424907">{{vcite journal|vauthors=Chen X, Yan SD|title=Mitochondrial Abeta: A Potential Cause of Metabolic Dysfunction in Alzheimer's Disease|journal=IUBMB Life|volume=58|issue=12|pages=686–94|year=2006|pmid=17424907|doi=10.1080/15216540601047767|month=December}}</ref>。 |
|||
多種發炎反應和[[細胞激素]]也可能在阿茲海默症的病理變化相關<ref name="pmid15681814">{{vcite journal|vauthors=Greig NH, Mattson MP, Perry T|title=New Therapeutic Strategies and Drug Candidates for Neurodegenerative Diseases: p53 and TNF-alpha Inhibitors, and GLP-1 Receptor Agonists|journal=Annals of the New York Academy of Sciences|volume=1035|pages=290–315|year=2004|pmid=15681814|doi=10.1196/annals.1332.018|month=December}}</ref>。越來越多證據顯示腦部神經元與免疫系統之間有很強的交互作用。肥胖與全身性發炎反應等干擾免疫反應的因子,可能都會引起疾病惡化<ref>{{cite journal|title=Neuroinflammation in Alzheimer's disease|date=April 2015|journal=The Lancet. Neurology|issue=4|doi=10.1016/S1474-4422(15)70016-5|volume=14|pages=388–405|pmid=25792098|vauthors=Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, Herrup K, Frautschy SA, Finsen B, Brown GC, Verkhratsky A, Yamanaka K, Koistinaho J, Latz E, Halle A, Petzold GC, Town T, Morgan D, Shinohara ML, Perry VH, Holmes C, Bazan NG, Brooks DJ, Hunot S, Joseph B, Deigendesch N, Garaschuk O, Boddeke E, Dinarello CA, Breitner JC, Cole GM, Golenbock DT, Kummer MP}}</ref>。 |
|||
不同[[神经营养因子]]以及其受體的分佈變化也在阿茲海默症中發現,例如[[脑源性神经营养因子]]<ref name="pmid18708092">{{cite journal |accessdate=2013-02-04 |language=en |author=Tapia-Arancibia L, Aliaga E, Silhol M, Arancibia S |title=New insights into brain BDNF function in normal aging and Alzheimer disease |journal=Brain Research Reviews |volume=59 |issue=1 |pages=201–20 |pmid=18708092 |doi=10.1016/j.brainresrev.2008.07.007|date=Nov 2008}}</ref><ref name="pmid18184369">{{cite journal |accessdate=2013-02-04 |language=en |doi=10.1111/j.1601-183X.2007.00378.x |author=Schindowski K, Belarbi K, Buée L |title=Neurotrophic factors in Alzheimer's disease: role of axonal transport |journal=Genes, Brain and Behavior |volume=7 |issue=Suppl 1 |pages=43–56 |pmid=18184369 |pmc=2228393|date=Feb 2008}}</ref>。 |
|||
不同{{tsl|en|neurotrophic factor|神經滋養因子|}}(如[[脑源性神经营养因子]])的分布變化,以及其受體的表現狀況,都曾有研究指出與阿茲海默症有關<ref>{{vcite journal|vauthors=Tapia-Arancibia L, Aliaga E, Silhol M, Arancibia S|title=New insights into brain BDNF function in normal aging and Alzheimer disease|journal=Brain Research Reviews|volume=59|issue=1|pages=201–20|year=2008|pmid=18708092|doi=10.1016/j.brainresrev.2008.07.007|month=Nov}}</ref><ref>{{vcite journal|vauthors=Schindowski K, Belarbi K, Buée L|title=Neurotrophic factors in Alzheimer's disease: role of axonal transport|journal=Genes, Brain, and Behavior|volume=7|issue=Suppl 1|pages=43–56|year=2008|pmid=18184369|pmc=2228393|doi=10.1111/j.1601-183X.2007.00378.x|month=Feb}}</ref>。 |
|||
===基因=== |
|||
雖然研究顯示有些基因可能是阿茲海默症的危險因子,但是絕大部分的阿茲海默症病患都不是因為遺傳因素而患病,這些病患稱為偶發型阿茲海默症;另一方面,約0.1%的病患具有體染色體顯性家族性遺傳變異,這些病患通常在65歲前發病,而被歸類為家族型阿兹海默症<ref name="pmid16876668">{{cite journal |accessdate=2013-02-16 |language=en |author=Blennow K, de Leon MJ, Zetterberg H |title=Alzheimer's disease |journal=Lancet |volume=368 |issue=9533 |pages=387–403 |pmid=16876668 |doi=10.1016/S0140-6736(06)69113-7|url=|date=July 2006}}</ref>。 |
|||
==診斷== |
|||
家族型阿茲海默症病患大多可以歸因於以下三個基因其中之一發生突變:[[前類澱粉蛋白質]]基因 ''APP'' 、''[[Presenilin]] 1''和''Presenilin 2'' <ref name="pmid18332245">{{cite journal|accessdate=2013-02-27 |language=en |author=Waring SC, Rosenberg RN |title=Genome-wide association studies in Alzheimer disease |journal=Arch Neurol |volume=65 |issue=3 |pages=329–34 |pmid=18332245 |doi=10.1001/archneur.65.3.329|date=March 2008}}</ref>。''APP''基因表現的APP蛋白在修飾後會產生{{link-en|β類澱粉胜肽|Beta amyloid}} (Aβ),而前述三個基因的突變會導致[[類澱粉蛋白|類澱粉蛋白質]]斑塊的主要成分Aβ42在細胞中的產量升高<ref name="pmid10392577">{{cite journal |accessdate=2013-04-06 |language=en |author=Selkoe DJ |title=Translating cell biology into therapeutic advances in Alzheimer's disease |journal=Nature |volume=399 |issue=6738 Suppl |pages=A23–31 |pmid=10392577 |doi=10.1038/19866|date=June 1999}}</ref>,有些突變則不會增加Aβ42在細胞中的產量,僅是改變細胞內Aβ42和其他主要同型異構物(如Aβ40)的比例<ref name="pmid8938131">{{cite journal |accessdate=2013-04-05 |language=en |author=Borchelt DR |title=Familial Alzheimer's disease-linked presenilin 1 variants elevate βA1-42/1-40 ratio in vitro and in vivo |journal=Neuron|volume=17|issue=5|pages=1005–13 |pmid=8938131 |doi=10.1016/S0896-6273(00)80230-5 |type=Original article |last12=Wang|first12=R |last13=Seeger|first13=M|first14=AI|first15=SE|first16=NG|first17=NA|first18=DL|first19=SG|last20=Sisodia|first20=SS |author2=Thinakaran G |author3=Eckman CB |display-authors=3 |last4=Levey |last5=Gandy |last6=Copeland |last7=Jenkins |last8=Price |last9=Younkin |first4=Michael K. |first5=Frances |first6=Tamara |first7=Cristian-Mihail |first8=Grace |first9=Sophia|date=Nov 1996}}</ref><ref name="pmid17254019">{{cite journal |accessdate=2013-04-05 |language=en |author=Shioi J |title=FAD mutants unable to increase neurotoxic Aβ 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta |journal=J Neurochem|volume=101|issue=3|pages=674–81 |pmid=17254019 |doi=10.1111/j.1471-4159.2006.04391.x |author2=Georgakopoulos A |author3=Mehta P |display-authors=3 |last4=Kouchi |first4=Zen |last5=Litterst |first5=Claudia M |last6=Baki |first6=Lia |last7=Robakis |first7=Nikolaos K|date=May 2007}}</ref>。這解釋了為何某些''Presenilin''基因突變即使降低Aβ產量仍可以導致疾病發生,也指出Presenilin蛋白質可能有其他功能,例如改變APP的功能或是Aβ以外的其他片段的功能。 |
|||
[[File:PET Alzheimer.jpg|thumb|left|Upright|腦部[[正电子发射计算机断层扫描|正子照影]](PET)顯示這名患者的顳葉功能喪失。]] |
|||
阿茲海默症的診斷一般透過[[病史]]收集和行為觀察獲得。臨床醫師可透過觀察患者[[神經內科|神經學]]及[[神经心理学|神經心理學]]上的特徵,並{{link-en|除外診斷|Diagnosis of exclusion|排除其他診斷}}來佐證診斷<ref name="pmid17407994">{{vcite journal|vauthors=Mendez MF|title=The Accurate Diagnosis of Early-onset Dementia|journal=International Journal of Psychiatry in Medicine|volume=36|issue=4|pages=401–12|year=2006|pmid=17407994|doi=10.2190/Q6J4-R143-P630-KW41}}</ref><ref name="pmid17018549">{{vcite journal|vauthors=Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J|title=Therapeutic Approaches to Alzheimer's Disease|journal=Brain|volume=129|issue=Pt 11|pages=2840–55|year=2006|pmid=17018549|doi=10.1093/brain/awl280|month=November}}</ref>。[[電腦斷層掃瞄]](CT)、[[核磁共振成像]](MRI)、{{link-en|單光子電腦斷層攝影|Single-photon emission computed tomography}}(SPECR),和[[正电子发射计算机断层扫描|正子電腦斷層攝影]](PET)等高階[[醫學影像|醫學影像技術]],可以協助排除其他大腦病變或失智症亞型<ref>{{cite book|url=http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf|title=Dementia: Quick Reference Guide|date=November 2006|publisher=(UK) {{tsl|en|National Institute for Health and Clinical Excellence||National Institute for Health and Clinical Excellence}}|isbn=1-84629-312-X|location=London|format=PDF|deadurl=yes|access-date=22 February 2008|archive-url=https://web.archive.org/web/20080227161412/http://www.nice.org.uk/nicemedia/pdf/CG042quickrefguide.pdf|archive-date=27 February 2008}}</ref>。此外,醫學影像也可以用於預測從輕微認知失調到阿茲海默症的轉變<ref name="Schroeter">{{vcite journal|vauthors=Schroeter ML, Stein T, Maslowski N, Neumann J|title=Neural Correlates of Alzheimer's Disease and Mild Cognitive Impairment: A Systematic and Quantitative Meta-Analysis involving 1,351 Patients|journal=NeuroImage|volume=47|issue=4|pages=1196–206|year=2009|pmid=19463961|pmc=2730171|doi=10.1016/j.neuroimage.2009.05.037}}</ref>。 |
|||
{{link-en|神經心理學評估|Neuropsychological assessment}}(包括記憶測試)可以進一步鑑別疾病狀態<ref name="pmid17222085" />,醫學組織已經為臨床醫師建立診斷標準以簡化及標準化診斷程序。阿茲海默症最準確的診斷方法為屍體[[驗屍|病理解剖]],直接取得腦組織,經由[[組織學]]免疫染色法進行確認診斷<ref name="pmid6610841">{{vcite journal|vauthors=McKhann G, Drachman D, Folstein M|title=Clinical Diagnosis of Alzheimer's Disease: Report of the NINCDS-ADRDA Work Group under the Auspices of Department of Health and Human Services Task Force on Alzheimer's Disease|journal=Neurology|volume=34|issue=7|pages=939–44|year=1984|pmid=6610841|month=July|doi=10.1212/wnl.34.7.939}}</ref>。 |
|||
大部分阿茲海默症病患並沒有體染色體遺傳疾病,這些病患稱為偶發型阿茲海默症。然而還是有些基因的異常可能是罹患阿茲海默症的危險因子。最著名的基因危險因子是[[载脂蛋白]]E的ε4 [[對偶基因]](''APOEε4'')<ref name="pmid8446617">{{cite journal |accessdate=2013-04-06 |language=en |author=Strittmatter WJ |title=Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease |journal=Proc Natl Acad Sci USA|volume=90|issue=5|pages=1977–81 |pmid=8446617 |pmc=46003 |doi=10.1073/pnas.90.5.1977 |author2=Saunders AM |author3=Schmechel D |display-authors=3 |last4=Pericak-Vance |first4=M |last5=Enghild |first5=J |last6=Salvesen |first6=GS |last7=Roses |first7=AD|date=March 1993}}</ref><ref name="pmid16567625">{{cite journal |accessdate=2013-04-06 |language=en |author=Mahley RW, Weisgraber KH, Huang Y |title=Apolipoprotein E4: A causative factor and therapeutic target in neuropathology, including Alzheimer's disease |journal=Proc. Natl. Acad. Sci. U.S.A.|volume=103|issue=15|pages=5644–51|pmid=16567625 |pmc=1414631 |doi=10.1073/pnas.0600549103|date=April 2006}}</ref>,約有40% - 80%阿茲海默症病患帶有至少一個''APOEε4''對偶基因<ref name="pmid16567625"/>,其中異型合子個體罹患阿茲海默症的風險增加3倍,而同型合子個體中則增加15倍<ref name="pmid16876668"/>。然而,這些基因造成的影響並非絕對是基因相關的。舉例來說,有些奈及利亞人罹患阿茲海默症的風險與是否帶有APOEε4對偶基因沒有相關<ref name="pmid16434658">{{cite journal |accessdate=2013-06-09 |author=Hall K, Murrell J, Ogunniyi A, Deeg M, Baiyewu O, Gao S, Gureje O, Dickens J, Evans R, Smith-Gamble V, Unverzagt FW, Shen J, Hendrie H |title=Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba |journal=Neurology|volume=66|issue=2|pages=223–227 |pmid=16434658 |pmc=2860622 |doi=10.1212/01.wnl.0000194507.39504.17|date=January 2006}}</ref><ref name="pmid16278853">{{cite journal |accessdate=2013-06-09 |author=Gureje O, Ogunniyi A, Baiyewu O, Price B, Unverzagt FW, Evans RM, Smith-Gamble V, Lane KA, Gao S, Hall KS, Hendrie HC, Murrell JR |title=APOE ε4 is not associated with Alzheimer's disease in elderly Nigerians |journal=Ann Neurol|volume=59|issue=1|pages=182–185 |pmid=16278853 |pmc=2855121 |doi=10.1002/ana.20694|date=January 2006}}</ref>。雖然基因學家同意其他許多基因也是阿茲海默症的危險因子,或是具有影響遲發型阿茲海默症病情發展的保護效果<ref name="pmid18332245"/>,然而根據奈及利亞研究和尚未完成的阿茲海默症相關基因危險因子[[外显度]]的研究結果,均顯示環境因素扮演更重要的角色。超過400個基因已被研究其與遲發偶發型阿茲海默症的關聯,然而大部分的基因都沒有發現明顯相關性<ref name="pmid16876668"/>。 |
|||
===診斷標準=== |
|||
有些研究發現''{{link-en|TREM2|TREM2}}''基因突變會增加罹患阿茲海默症的風險達3到5倍<ref>{{cite journal |accessdate=2013-06-09 |language=en |doi=10.1056/NEJMoa1211103 |title=Variant of TREM2 associated with the risk of Alzheimer's disease |year=2012 |last1=Jonsson |first1=Thorlakur |last2=Stefansson |first2=Hreinn |last3=Steinberg |first3=Stacy |last4=Jonsdottir |first4=Ingileif |last5=Jonsson |first5=Palmi V |last6=Snaedal |first6=Jon |last7=Bjornsson |first7=Sigurbjorn |last8=Huttenlocher |first8=Johanna |last9=Levey |first9=Allan I |journal=New England Journal of Medicine |pages= |type=Original article}}</ref><ref>{{cite journal |accessdate=2013-06-09 |language=en |doi=10.1056/NEJMoa1211851 |title=TREM2 variants in Alzheimer's disease |year=2012 |last1=Guerreiro |first1=Rita |last2=Wojtas |first2=Aleksandra |last3=Bras |first3=Jose |last4=Carrasquillo |first4=Minerva |last5=Rogaeva |first5=Ekaterina |last6=Majounie |first6=Elisa |last7=Cruchaga |first7=Carlos |last8=Sassi |first8=Celeste |last9=Kauwe |first9=John S.K. |journal=New England Journal of Medicine |pages= |type=Original article}}</ref>,可能的原因是當''TREM2''基因突變時,腦中的白血球就無法控制大腦中Aβ的產生量。 |
|||
{{tsl|en|National Institute of Neurological and Communicative Disorders and Stroke|美國神經與溝通疾患及中風研究院|}}(NINCDS)及{{tsl|en|Alzheimer's Disease and Related Disorders Association|阿茲海默症及相關疾病協會|}}(ADRDA)於1984年制定了{{tsl|en|NINCDS-ADRDA Alzheimer's Criteria|NINCDS-ADRDA阿茲海默症診斷標準|}},為目前最常用的診斷標準之一<ref name="pmid6610841"/>,最新一版於2007年更新<ref name="pmid176164822">{{vcite journal|vauthors=Dubois B, Feldman HH, Jacova C|title=Research Criteria for the Diagnosis of Alzheimer's Disease: Revising the NINCDS-ADRDA Criteria|journal=Lancet Neurology|volume=6|issue=8|pages=734–46|year=2007|pmid=17616482|doi=10.1016/S1474-4422(07)70178-3|month=August}}</ref>。臨床診斷標準包含{{tsl|en|Developmental disability|發展性障礙|認知功能損害}}、疑似失智症狀,並經由{{tsl|en|Neuropsychological assessment|神經心理學評估|}}確認。 |
|||
腦組織的[[微觀|顯微鏡檢]]可以提供阿茲海默症的{{tsl|en|histopathologic|組織病理學|}}確認診斷。上述的診斷標準在藉由組織病理學進行評估後,顯示該標準的[[信度]]及[[效度]]都不錯<ref name="pmid7986174">{{vcite journal|vauthors=Blacker D, Albert MS, Bassett SS|title=Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative|journal=Archives of Neurology|volume=51|issue=12|pages=1198–204|year=1994|pmid=7986174|month=December|doi=10.1001/archneur.1994.00540240042014}}</ref>。阿茲海默症最常損害的八個智能區塊為[[記憶]]、[[語言]]、[[知觉]]、[[注意|注意力]]、[[动作技能]]、{{tsl|en|orientation (mental)|定向力|}}、[[解决问题|問題解決能力]]、[[管控功能|執行能力]]等。這些問題在NINCDS-ADRDA診斷標準及[[美國精神醫學學會]]發行的《[[精神疾病診斷與統計手冊]]》(DSM-IV-TR)皆有提到<ref>{{cite book|title=Diagnostic and statistical manual of mental disorders: DSM-IV-TR|last=American Psychiatric Association|publisher=American Psychiatric Association|year=2000|isbn=0-89042-025-4|edition=4th Edition Text Revision|location=Washington, DC}}</ref><ref name="pmid8752526">{{vcite journal|vauthors=Ito N|title=[Clinical aspects of dementia]|language=Japanese|journal=Hokkaido Igaku Zasshi|volume=71|issue=3|pages=315–20|year=1996|pmid=8752526|month=May}}</ref>。 |
|||
== 病理 == |
|||
阿茲海默病主要是[[神經細胞]]的損失(或退化),以及腦中出現[[類澱粉斑|類澱粉斑塊]]以及[[神經纖維糾結]]。已知遺傳因素很重要。並且發現有三種不同[[體染色體顯性]]基因與少數家族性、早發性AD有關。這三種分別是:Presenilin 1, Presenilin 2, Amyloid Precursor Protein。晚發性AD(LOAD)只找到一個易感性基因:the epsilon 4 allele of the APOE gene。發病的年紀有50%的[[遺傳性]]。 |
|||
===檢測技術=== |
|||
在[[病理學]]上顯示出腦組織萎縮、[[大腦皮質]]出現[[老年斑]]等現象。研究發現老年斑是[[β澱粉樣蛋白]]的沉積所造成。從[[髓液]]將腦內{{link-en|β類澱粉胜肽|Beta amyloid}} (Aβ) 進行定量控制的工具現在正在實用化研發階段。 |
|||
[[File:InterlockingPentagons.svg|right|thumb|神經心理學{{tsl|en|screening test|篩檢|}}可以協助阿茲海默症的診斷。在此試驗中,受試者會被要求在另一張紙畫出圖中的圖形。另外也可能會請受試者記住單詞、閱讀,或是遞減數字。]] |
|||
[[簡短智能測驗]](MMSE)等{{tsl|en|Neuropsychological test|神經心理學檢查|}}常被用於評估認知功能障礙,以利於後續診斷。若要取得更可信的結果,可以進行更全面的測試,特別是在疾病初期的患者<ref name="pmid1512391">{{vcite journal|vauthors=Tombaugh TN, McIntyre NJ|title=The mini-mental state examination: a comprehensive review|journal=Journal of the American Geriatrics Society|volume=40|issue=9|pages=922–35|year=1992|pmid=1512391|month=September|doi=10.1111/j.1532-5415.1992.tb01992.x}}</ref><ref name="pmid9987708">{{vcite journal|vauthors=Pasquier F|title=Early diagnosis of dementia: neuropsychology|journal=Journal of Neurology|volume=246|issue=1|pages=6–15|year=1999|pmid=9987708|doi=10.1007/s004150050299|month=January}}</ref>。除非有明顯的認知功能障礙,{{tsl|en|Neurological examination|神經學檢察|}}結果在疾病初期一般會呈現正常,可能無法與其他疾病做出鑑別,包含其他原因造成的失智症。 |
|||
但是Aβ是否為本症的直接原因,或者是患病後呈現出的結果,現在還沒有定論<ref name="活力藥師網"/>。 |
|||
進一步的神經學檢查對於阿茲海默症的鑑別診斷相當重要<ref name="pmid17222085"/>,與家人會談也有助於評估病情。主要照護人能夠提供患者日常活動功能的重要資訊,以及病人 |
|||
==病因== |
|||
{{tsl|en|mental function|心智功能|}}下降的情形<ref name="pmid16327345">{{vcite journal|vauthors=Harvey PD, Moriarty PJ, Kleinman L|title=The Validation of a Caregiver Assessment of Dementia: the Dementia Severity Scale|journal=Alzheimer Disease and Associated Disorders|volume=19|issue=4|pages=186–94|year=2005|pmid=16327345|doi=10.1097/01.wad.0000189034.43203.60}}</ref>。由於患者通常自己{{tsl|en|anosognosia|病覺缺失症|無法查覺自身的異狀}},因此旁觀者的觀點對於疾病的評估相當重要<ref name="pmid15738860">{{vcite journal|vauthors=Antoine C, Antoine P, Guermonprez P, Frigard B|title=Awareness of Deficits and Anosognosia in Alzheimer's Disease|language=French|journal=L'Encéphale|volume=30|issue=6|pages=570–77|year=2004|pmid=15738860|doi=10.1016/S0013-7006(04)95472-3}}</ref>。但在失智症初期時,家人通常也無法察覺病人的症狀,而無法提供醫師準確的資訊<ref name="pmid16197855">{{vcite journal|vauthors=Cruz VT, Pais J, Teixeira A, Nunes B|title=The Initial Symptoms of Alzheimer Disease: Caregiver Perception|language=Portuguese|journal=Acta Médica Portuguesa|volume=17|issue=6|pages=435–44|year=2004|pmid=16197855}}</ref>。 |
|||
大部分病患罹患阿茲海默症的原因仍然不明<ref> |
|||
{{cite web |url=http://www.alz.org/research/science/alzheimers_disease_causes.asp |title=What We Know Today About Alzheimer's Disease |publisher=Alzheimer's Association |quote=While scientists know Alzheimer's disease involves progressive brain cell failure, the reason cells fail isn't clear. |accessdate=2012-12-20}}</ref><ref>{{cite web |url=http://www.med.nyu.edu/adc/forpatients/ad.html#causes |title=Alzheimer's Disease: Causes |publisher=NYU Medical Center/NYU School of Medicine |quote=The cause of Alzheimer's disease is not yet known, but scientists are hoping to find the answers by studying the characteristic brain changes that occur in a patient with Alzheimer's disease. In rare cases when the disease emerges before the age of sixty-five, these brain changes are caused by a genetic abnormality. Scientists are also looking to genetics as well as environmental factors for possible clues to the cause and cure of Alzheimer's disease. |accessdate=2012-12-20 }}{{dead link|date=2018年5月 |bot=InternetArchiveBot |fix-attempted=yes }}</ref>(除了1%到5%的病患可以找到基因差異),目前有幾個不同的[[假说]]試著解釋阿茲海默症的病因: |
|||
輔助性檢查可以提供一些額外資訊,以利排除其他診斷。[[血液检查]]也可以協助排除阿茲海默症以外的診斷<ref name="pmid17222085" />,偶見有些病因是可以治癒的<ref>{{vcite journal | vauthors = Clarfield AM | title = The Decreasing Prevalence of Reversible Dementias: An Updated Meta-analysis | journal = Archives of Internal Medicine | volume = 163 | issue = 18 | pages = 2219–29 | year = 2003 | pmid = 14557220 | doi = 10.1001/archinte.163.18.2219 | month = October }}</ref>。常見的血檢項目包含{{tsl|en|thyroid function tests|甲狀腺功能測試|}}、[[维生素B12全合成|维生素B<sub>12</sub>]]、[[梅毒]]檢測、代謝性疾病檢查(如腎功能檢查、電解質水平,以及糖尿病檢查)、重金屬水平,以及貧血等等。另外也必須[[譫妄]]的可能性。 |
|||
===膽鹼性假說=== |
|||
{{link-en|膽鹼性|Cholinergic}}假說是最早被提出來的假說,也是現今大部分阿茲海默症藥物所依據的理論基礎<ref name="pmid10071091">{{cite journal|language=en |author=Francis PT, Palmer AM, Snape M, Wilcock GK |title=The cholinergic hypothesis of Alzheimer's disease: a review of progress |journal=J. Neurol. Neurosurg. Psychiatr.|volume=66 |issue=2 |pages=137–47 |pmid=10071091 |pmc=1736202 |doi=10.1136/jnnp.66.2.137 |url= |accessdate=2012-12-22|date=February 1999}}</ref>,該假說認為阿茲海默症是由於神經系統減少產生[[神經傳導物質]][[乙酰胆碱]]而造成的,雖然膽鹼性假說的歷史悠久,但是沒有受到廣泛的支持,主要是由於使用藥物治療乙醯膽鹼缺乏後,對於阿茲海默症的療效有限。其他膽鹼性效應也曾被提出,例如:大量的[[類澱粉蛋白]]沉澱導致廣泛的神經發炎反應<ref name="pmid12934968">{{cite journal |language=en |author=Wenk GL |title=Neuropathologic changes in Alzheimer's disease |journal=J Clin Psychiatry |volume=64 Suppl 9 |pages=7–10 |year=2003 |pmid=12934968 |accessdate=2012-12-22}}</ref><ref name="pmid15236795">{{cite journal |language=en |author=Shen ZX |title=Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease |journal=Med Hypotheses |volume=63 |issue=2 |pages=308–21 |year=2004 |pmid=15236795 |doi=10.1016/j.mehy.2004.02.031|accessdate=2012-12-22}}</ref>。 |
|||
針對[[重性抑郁障碍|抑鬱症]]的[[心理測驗]]也建議進行,因為阿茲海默症常{{tsl|en|Depression of Alzheimer disease|阿茲海默症的抑鬱症狀|同時伴隨抑鬱症狀}},也是認知功能損傷的早期症狀之一<ref>{{vcite journal | vauthors = Sun X, Steffens DC, Au R | display-authors = etal | title = Amyloid-Associated Depression: A Prodromal Depression of Alzheimer Disease? | journal = Archives of General Psychiatry | volume = 65 | issue = 5 | pages = 542–50 | year = 2008 | pmid = 18458206 | pmc = 3042807 | doi = 10.1001/archpsyc.65.5.542 | url = http://archpsyc.ama-assn.org/cgi/content/short/65/5/542 | deadurl = no | archive-url = https://web.archive.org/web/20080706023907/http://archpsyc.ama-assn.org/cgi/content/short/65/5/542 | archive-date = 6 July 2008 | df = dmy-all }}</ref>,甚至是原因<ref name="pmid9153154">{{vcite journal | vauthors = Geldmacher DS, Whitehouse PJ | title = Differential Diagnosis of Alzheimer's Disease | journal = Neurology | volume = 48 | issue = 5 Suppl 6 | pages = S2–9 | year = 1997 | pmid = 9153154 | month = May | doi = 10.1212/WNL.48.5_Suppl_6.2S}}</ref><ref name="pmid17495754">{{vcite journal | vauthors = Potter GG, Steffens DC | title = Contribution of Depression to Cognitive Impairment and Dementia in Older adults | journal = The Neurologist | volume = 13 | issue = 3 | pages = 105–17 | year = 2007 | pmid = 17495754 | doi = 10.1097/01.nrl.0000252947.15389.a9 | month = May }}</ref>。 |
|||
=== 類澱粉胜肽假說 === |
|||
1991年,學者提出類澱粉胜肽假說,認為{{link-en|β類澱粉胜肽|Beta amyloid}}(Aβ)在大腦堆積可能是導致阿茲海默症的根本原因<ref name="pmid1763432">{{cite journal |language=en |author=Hardy J, Allsop D |title=Amyloid deposition as the central event in the aetiology of Alzheimer's disease |journal=Trends Pharmacol. Sci. |volume=12 |issue=10 |pages=383–88 |pmid=1763432 |doi=10.1016/0165-6147(91)90609-V |accessdate=2012-12-23 |date=October 1991}}</ref><ref name="pmid11801334">{{cite journal |language=en |author=Mudher A, Lovestone S |title=Alzheimer's disease-do tauists and baptists finally shake hands? |journal=Trends Neurosci. |volume=25 |issue=1 |pages=22–26 |pmid=11801334 |doi=10.1016/S0166-2236(00)02031-2 |accessdate=2012-12-23|date=January 2002}}</ref>。根據研究發現表現Aβ的[[前類澱粉蛋白質]]基因(''APP'')位在第21對染色體上,而[[唐氏综合症]]病患都多了一套第21對染色體基因,同時唐氏症病患幾乎全都在40歲左右時罹患阿茲海默症<ref name="pmid16904243">{{cite journal |language=en |
|||
|author=Nistor M |title=Alpha- and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain |journal=Neurobiol Aging |volume=28 |issue=10 |pages=1493–1506 |pmid=16904243 |doi=10.1016/j.neurobiolaging.2006.06.023 |last12=Head |first12=E |author2=Don M |author3=Parekh M |display-authors=3 |last4=Sarsoza |first4=F.|last5=Goodus |first5=M.|last6=Lopez |first6=G.E.|last7=Kawas |first7=C.|last8=Leverenz |first8=J.|last9=Doran |first9=E.|accessdate=2012-12-23|date=October 2007}}</ref><ref name="pmid15639317">{{cite journal |accessdate=2012-12-23 |language=en |author=Lott IT, Head E |title=Alzheimer disease and Down syndrome: factors in pathogenesis |journal=Neurobiol Aging |volume=26 |issue=3 |pages=383–89 |pmid=15639317 |doi=10.1016/j.neurobiolaging.2004.08.005|date=March 2005}}</ref>,加上阿茲海默症的主要遺傳危險因子{{link-en|E型載脂蛋白質|Apolipoprotein E}}會導致[[類澱粉蛋白|類澱粉蛋白質]]斑塊在大腦中累積<ref name="pmid7566000">{{cite journal |accessdate=2012-12-23 |language=en |author=Polvikoski T |title=Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein |journal=N Engl J Med |volume=333 |issue=19 |pages=1242–47 |pmid=7566000 |doi=10.1056/NEJM199511093331902 |author2=Sulkava R |author3=Haltia M |display-authors=3 |last4=Kainulainen |first4=Katariina |last5=Vuorio |first5=Alpo |last6=Verkkoniemi |first6=Auli |last7=Niinistö |first7=Leena |last8=Halonen |first8=Pirjo |last9=Kontula |first9=Kimmo|date=November 1995}}</ref>,因此推測Aβ是導致阿茲海默症的原因,進一步的證據則是來自於轉殖基因老鼠實驗,研究人員在實驗老鼠身上表現突變型人類''APP''基因,結果發現實驗老鼠的大腦會產生纖維狀的[[類澱粉蛋白|類澱粉蛋白質]]斑塊(fibrillar amyloid plaques)和類似阿茲海默症的大腦病理變化及空間學習障礙(spatial learning deficits)<ref name="轉基因實驗">{{cite journal | language=en |author =Howlett DR| title = APP transgenic mice and their application to drug discovery | journal = Histol Histopathol| volume = 26 | issue = 12 | pages = 1611-1632|date=December 2011}}</ref><ref name="pmid7845465">{{cite journal |accessdate=2012-12-23 |language=en |author=Games D |title=Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein |journal=Nature |volume=373 |issue=6514 |pages=523–27 |pmid=7845465 |doi=10.1038/373523a0 |author2=Adams D |author3=Alessandrini R |display-authors=3 |last4=Barbour |first4=Robin |last5=Borthelette |first5=Patricia |last6=Blackwell |first6=Catherine |last7=Carr |first7=Tony |last8=Clemens |first8=James |last9=Donaldson |first9=Thomas|date=February 1995}}</ref><ref name="pmid8795633">{{cite journal |accessdate=2012-12-23 |language=en |author=Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D |title=Comparison of neurodegenerative pathology in transgenic mice overexpressing V717F beta-amyloid precursor protein and Alzheimer's disease |journal=J Neurosci |volume=16 |issue=18 |pages=5795–811 |pmid=8795633|date=September 1996}}</ref><ref name="pmid8810256">{{cite journal |accessdate=2012-12-23 |language=en |author=Hsiao K |title=Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice |journal=Science |volume=274 |issue=5284 |pages=99–102 |pmid=8810256 |doi=10.1126/science.274.5284.99 |author2=Chapman P |author3=Nilsen S |display-authors=3 |last4=Eckman |first4=C. |last5=Harigaya |first5=Y. |last6=Younkin |first6=S. |last7=Yang |first7=F. |last8=Cole |first8=G.|date=October 1996}}</ref><ref name="pmid12426044">{{cite journal |accessdate=2012-12-23 |language=en |author=Lalonde R, Dumont M, Staufenbiel M, Sturchler-Pierrat C, Strazielle C. |title=Spatial learning, exploration, anxiety, and motor coordination in female APP23 transgenic mice with the Swedish mutation |journal=Brain Research (journal) |volume=956 |pages=36–44 |pmid=12426044 |doi=10.1016/S0006-8993(02)03476-5 |year=2002 |issue=1}}</ref>。 |
|||
C-PIB正子照影(C-PIB PET)在疾病初期的準確率不高,因此不建議用於早期診斷,或預測輕度知能障礙患者進展到阿茲海默症的機會<ref>{{cite journal|title=(11)C-PIB-PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI)|date=July 2014|journal=The Cochrane Database of Systematic Reviews|issue=7|doi=10.1002/14651858.CD010386.pub2|pages=CD010386|pmid=25052054|vauthors=Zhang S, Smailagic N, Hyde C, Noel-Storr AH, Takwoingi Y, McShane R, Feng J}}</ref>。¹⁸F-FDG正子照影(¹⁸F-FDG PET)在預測阿茲海默症的發生機會上也沒有實證支持<ref>{{cite journal|title=¹⁸F-FDG PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI)|date=January 2015|journal=The Cochrane Database of Systematic Reviews|doi=10.1002/14651858.CD010632.pub2|volume=1|pages=CD010632|pmid=25629415|vauthors=Smailagic N, Vacante M, Hyde C, Martin S, Ukoumunne O, Sachpekidis C}}</ref>。 |
|||
然而在早期人體試驗中曾發現一個實驗性的疫苗可以清除類澱粉蛋白質斑塊,利用這個疫苗治療失智症病患卻沒有顯著的效果<ref name="pmid18640458">{{cite journal |accessdate=2012-12-23 |language=en |author=Holmes C |title=Long-term effects of Abeta42 immunisation in Alzheimer's disease: follow-up of a randomised, placebo-controlled phase I trial |journal=Lancet |volume=372 |issue=9634 |pages=216–23 |pmid=18640458 |doi=10.1016/S0140-6736(08)61075-2 |last12=Nicoll |first12=JA |author2=Boche D |author3=Wilkinson D |display-authors=3 |last4=Yadegarfar |first4=Ghasem |last5=Hopkins |first5=Vivienne |last6=Bayer |first6=Anthony |last7=Jones |first7=Roy W |last8=Bullock |first8=Roger |last9=Love |first9=Seth|date=July 2008}}</ref>。因此研究者改而懷疑不是Aβ形成的大型[[類澱粉蛋白|類澱粉蛋白質]]斑塊,而是其小型的[[低聚物|寡聚合物]] (oligomers) 是其主要的致病型態,也具有更高的神經毒性。這些的寡聚合物也被稱為類澱粉蛋白質衍生可溶性[[配體 (生物化學)|配體]](amyloid-derived diffusible ligands, ADDLs),這些配體會結合到神經細胞表面的[[受体 (生物化学)|受體]]並且改變神經突觸的結構,因此破壞神經元溝通<ref name="pmid17251419">{{cite journal |accessdate=2012-12-23 |language=en |author=Lacor PN |title=Aß Oligomer-Induced Aberrations in Synapse Composition, Shape, and Density Provide a Molecular Basis for Loss of Connectivity in Alzheimer's Disease |journal=Journal of Neuroscience |volume=27 |issue=4 |pages=796–807 |pmid=17251419 |doi=10.1523/JNEUROSCI.3501-06.2007 |last2=Buniel |first2=MC |last3=Furlow |first3=PW |last4=Clemente |first4=AS |last5=Velasco |first5=PT |last6=Wood |first6=M |last7=Viola |first7=KL |last8=Klein |first8=WL |display-authors=1|date=January 2007}}</ref>。先前研究中顯示Aβ寡聚合物會結合在細胞膜外正常構型的[[普利昂蛋白|普利昂蛋白質]] (其錯誤構型造成的[[蛋白質聚集]]現象會引起[[牛海綿狀腦病|狂牛症]]和人類[[庫賈氏症]]),因此可能與阿茲海默症的發病有關,這項研究也顯示這些不同的[[神经退行性疾病|神經退化性疾病]]的機轉可能有互相關聯<ref name="pmid19242475">{{cite journal |accessdate=2012-12-23 |language=en |author=Lauren J |title=Cellular Prion Protein Mediates Impairment of Synaptic Plasticity by Amyloid-β Oligomers |journal=Nature |volume=457 |issue=7233 |pages=1128–32 |pmid=19242475 |doi=10.1038/nature07761 |pmc=2748841 |author2=Gimbel D |display-authors=2 |last3=Nygaard |first3=Haakon B. |last4=Gilbert |first4=John W. |last5=Strittmatter |first5=Stephen M.|date=February 2009}}</ref>。 |
|||
==預防== |
|||
2009年,類澱粉胜肽假說有了新的發展,新的研究認為 Death Receptor 6 (DR6) 蛋白和 APP (Aβ未修飾的原本形態) 蛋白的結合產生的下游[[訊息傳遞 (生物)|訊息傳導]]可能才是阿茲海默症的主要罪魁禍首。發育中神經細胞會大量表現的 DR6 和神經的[[细胞凋亡|細胞凋亡]]有關,在缺乏神經營養因子 (例如Nerve Growth Factor, NGF) 的狀況下會啟動神經細胞本體和軸突的凋亡。這個研究發現APP是DR6的一個[[配體 (生物化學)|配體]],在APP被β-secretase 酵素 (由APP產生Aβ時同樣需要它的修飾) 從APP上切下來後所產生的[[胺基端|N端]]的片段 (N-APP) ,會被一個未知的機制進一步切割並與DR6結合,最終啟動了[[细胞凋亡|細胞凋亡]]的路徑<ref name="pmid19225519">{{cite journal|title=APP binds DR6 to cause axon pruning and neuron death via distinct caspases|author=Nikolaev A, McLaughlin T, O'Leary D, Tessier-Lavigne M|date=19 February 2009|journal=Nature|accessdate=2012-12-23|issue=7232|doi=10.1038/nature07767|volume=457|pages=981–989|language=en|issn=0028-0836|pmc=2677572|pmid=19225519}}</ref>。N-APP/DR6信號傳導所啟動的神經細胞凋亡包含細胞本體和軸突,不同於一般細胞凋亡的機制需要激發caspase-3蛋白,神經[[轴突|軸突]]的退化需要激發caspase-6蛋白,而且是在神經軸突上呈現點狀散佈的激發,進而造成軸突的凋亡。此外,經由caspase-6路徑所啟動的細胞凋亡,也可能和另一種[[神经退行性疾病|神經退化疾病]]-[[亨丁頓舞蹈症|杭廷頓舞蹈症]]相關<ref>{{Cite journal|title=Cleavage at the caspase-6 site is required for neuronal dysfunction and degeneration due to mutant huntingtin|url=https://www.ncbi.nlm.nih.gov/pubmed/16777606|last=Graham|first=Rona K.|last2=Deng|first2=Yu|date=2006-06-16|journal=Cell|issue=6|doi=10.1016/j.cell.2006.04.026|volume=125|pages=1179–1191|issn=0092-8674|pmid=16777606|last3=Slow|first3=Elizabeth J.|last4=Haigh|first4=Brendan|last5=Bissada|first5=Nagat|last6=Lu|first6=Ge|last7=Pearson|first7=Jacqueline|last8=Shehadeh|first8=Jacqueline|last9=Bertram|first9=Lisa}}</ref>。 |
|||
[[File:Honoré Daumier 032.jpg|right|thumb|[[下棋]]及日常社交等益智活動,於流行病學上顯示與較低的阿茲海默症發生風險相關,但目前其因果性尚未證實。]] |
|||
目前實證上沒有任何能有效預防阿茲海默症的方式<ref name="nonprevention" />,有關預防及推遲阿茲海默症進程的跨國研究結果經常不一致。流行病學研究推測阿茲海默症可能與某些飲食、心血管風險、藥物等因子相關。某些智力活動及族群發生阿茲海默症的機會可能也不同。但這些相關性是否真的可以用來預防阿茲海默症,仍需進一步的研究闡明<ref name=nonprevention/>。 |
|||
2018年11月22日,Nature發表了關於腦細胞基因重組的重磅研究成果。美國科學家為了尋找大腦中體細胞重組的確切證據,對阿爾茨海默病患者的大腦進行了分析。研究發現,患者神經元中含有數千種APP基因突變,是普通健康人的6倍!在這些APP基因突變中,有11個單核苷酸突變與家族性阿爾茨海默病中的已知突變相同,健康人大腦中並沒有這些突變。<ref>{{Cite news|url=http://www.zhongworld.com/2018/11/25/nature%E7%99%BC%E8%A1%A8%E8%A3%A1%E7%A8%8B%E7%A2%91%E5%BC%8F%E7%A0%94%E7%A9%B6%E6%88%90%E6%9E%9C%EF%BC%8Capp%E5%9F%BA%E5%9B%A0%E6%95%B8%E5%8D%83%E7%A8%AE%E7%AA%81%E8%AE%8A%E6%88%96%E6%98%AF%E9%98%BF/|title=Nature發表裡程碑式研究成果,APP基因數千種突變或是阿爾茨海默病真兇! - 中文世界|date=2018-11-25|newspaper=中文世界|accessdate=2018-12-02|language=zh-TW}}</ref> |
|||
===藥物=== |
|||
===微管相關蛋白質假說=== |
|||
雖然[[高膽固醇血症|高膽固醇]]、[[高血壓]]、[[糖尿病]],及[[吸煙|吸菸]]等心血管風險增強因子,可能與較高的阿茲海默症發生率相關<ref name="pmid18299540">{{vcite journal|vauthors=Patterson C, Feightner JW, Garcia A|title=Diagnosis and Treatment of Dementia: 1. Risk Assessment and Primary Prevention of Alzheimer Disease|journal=Canadian Medical Association Journal|volume=178|issue=5|pages=548–56|year=2008|pmid=18299540|pmc=2244657|doi=10.1503/cmaj.070796|month=February}}</ref><ref name="pmid17483665">{{vcite journal|vauthors=Rosendorff C, Beeri MS, Silverman JM|title=Cardiovascular Risk Factors for Alzheimer's Disease|journal=The American Journal of Geriatric Cardiology|volume=16|issue=3|pages=143–49|year=2007|pmid=17483665|doi=10.1111/j.1076-7460.2007.06696.x}}</ref>。但服用降膽固醇用的[[羟甲基戊二酸单酰辅酶A还原酶抑制剂|他汀類藥物]](Statins)無法有效預防阿茲海默症的發生或推遲其進程<ref name="pmid17877925">{{vcite journal | vauthors = Kuller LH | title = Statins and Dementia | journal = Current Atherosclerosis Reports | volume = 9 | issue = 2 | pages = 154–61 | year = 2007 | pmid = 17877925 | doi = 10.1007/s11883-007-0012-9 | month = August }}</ref><ref>{{cite journal | vauthors = McGuinness B, Craig D, Bullock R, Malouf R, Passmore P | title = Statins for the treatment of dementia | journal = The Cochrane Database of Systematic Reviews | volume = 7 | issue = 7 | pages = CD007514 | date = July 2014 | pmid = 25004278 | doi = 10.1002/14651858.CD007514.pub3 }}</ref>。 |
|||
微管相關蛋白質假說認為[[微管相關蛋白質]]異常是引起阿茲海默症病情發展的主因<ref name="pmid11801334"/>,在這個模型中,過度磷酸化的Tau蛋白質開始與其他Tau蛋白質配對結合,結果在神經細胞中形成了神經纖維糾結<ref name="pmid1669718">{{cite journal |accessdate=2012-12-29 |language=en |author=Goedert M, Spillantini MG, Crowther RA |title=Tau proteins and neurofibrillary degeneration |journal=Brain Pathol |volume=1 |issue=4 |pages=279–86 |pmid=1669718 |doi=10.1111/j.1750-3639.1991.tb00671.x|date=July 1991}}</ref>,在這種情形下,神經細胞內的微小管開始瓦解並導致神經細胞內的運送系統崩壞<ref name="pmid15615638">{{cite journal |accessdate=2012-12-29 |language=en |author=Iqbal K |title=Tau pathology in Alzheimer disease and other tauopathies |journal=Biochim Biophys Acta |volume=1739 |issue=2–3 |pages=198–210 |pmid=15615638 |doi=10.1016/j.bbadis.2004.09.008 |url= |last12=Grundke-Iqbal |first12=I |author2=Alonso Adel C |author3=Chen S |display-authors=3 |last4=Chohan |first4=M. Omar |last5=El-Akkad |first5=Ezzat |last6=Gong |first6=Cheng-Xin |last7=Khatoon |first7=Sabiha |last8=Li |first8=Bin |last9=Liu |first9=Fei|date=January 2005}}</ref>,這將造成神經細胞之間的生化溝通失效,接著並導致神經細胞死亡<ref name="pmid17127334">{{cite journal |accessdate=2012-12-29 |language=en |author=Chun W, Johnson GV |title=The role of tau phosphorylation and cleavage in neuronal cell death |journal=Front Biosci |volume=12 |pages=733–56 |year=2007 |pmid=17127334 |doi=10.2741/2097}}</ref>。 |
|||
長期使用[[非甾体抗炎药]](NSAIDs)在2007年時被認為可能與較低的阿茲海默症發生率相關<ref name="pmid17612054">{{vcite journal|vauthors=Szekely CA, Town T, Zandi PP|title=NSAIDs for the Chemoprevention of Alzheimer's Disease|journal=Sub-Cellular Biochemistry|volume=42|pages=229–48|year=2007|pmid=17612054|doi=10.1007/1-4020-5688-5_11|isbn=978-1-4020-5687-1|series=Subcellular Biochemistry}}</ref>。亦有證據顯示NSAID可以減少與[[類澱粉蛋白|類澱粉斑塊]]相關的{{tsl|en|chronic inflammation|慢性發炎|發炎}}反應。但由於副作用過高,相關的臨床實驗提早中止<ref name="nonprevention" />。截至目前為止,尚無預防研究完成試驗<ref name="nonprevention" />。NSAID對於治療阿茲海默症沒有任何功效,但為預防的候選藥物之一<ref>{{cite journal|title=Soothing the inflamed brain: effect of non-steroidal anti-inflammatory drugs on Alzheimer's disease pathology|date=February 2011|journal=CNS & Neurological Disorders Drug Targets|issue=1|doi=10.2174/187152711794488665|volume=10|pages=57–67|pmid=21143138|vauthors=Hoozemans JJ, Veerhuis R, Rozemuller JM, Eikelenboom P}}</ref>。[[更年期]]的[[激素替代療法]]可能會增加失智的風險,即使已經停藥也一樣<ref>{{vcite journal|vauthors=Marjoribanks J, Farquhar C, Roberts H, Lethaby A, Lee J|title=Long term hormone therapy for perimenopausal and postmenopausal women|journal=The Cochrane Database of Systematic Reviews|volume=1|issue=|page=CD004143|year=2017|pmid=28093732|doi=10.1002/14651858.CD004143.pub5}}</ref>。 |
|||
===其他假說=== |
|||
[[单纯疱疹病毒]]第一型也被報導過在帶有易感性''apoE''基因的人身上扮演引發阿茲海默症的角色<ref name="pmid18487848"> |
|||
{{cite journal |accessdate=2012-12-29 |language=en |author=Itzhaki RF, Wozniak MA |title=Herpes simplex virus type 1 in Alzheimer's disease: the enemy within |journal=J Alzheimers Dis |volume=13 |issue=4 |pages=393–405 |pmid=18487848 |doi= |issn=1387-2877 |url=http://iospress.metapress.com/openurl.asp?genre=article&issn=1387-2877&volume=13&issue=4&spage=393|date=May 2008}}</ref><ref>{{Cite news|url=https://www.bbc.com/ukchina/trad/vert-fut-46106733|title=皰疹導致老年癡呆——證據越來越充足|last=Itzhaki)|first=露絲·伊扎克 (Ruth|date=2018-11-06|newspaper=BBC 英伦网|accessdate=2018-11-09|language=en-GB}}</ref>。 |
|||
===生活型態=== |
|||
另一個假說認為阿茲海默症可能由大腦中與老化相關的[[髓磷脂]]斷裂引起,這個假說並認為在髓磷脂斷裂時釋放出來的鐵離子還可能會擴大傷害,維持體內平衡的髓磷脂修復過程則助長β類澱粉蛋白質和Tau蛋白質在大腦中囤積<ref name="pmid19775776">{{cite journal |accessdate=2012-12-29 |language=en |author=Bartzokis G |title=Alzheimer's disease as homeostatic responses to age-related myelin breakdown |journal=Neurobiol. Aging |volume=32 |issue=8 |pages=1341–71 |pmid=19775776 |pmc=3128664 |doi=10.1016/j.neurobiolaging.2009.08.007 |url=|date=August 2011}}</ref><ref name="pmid=15665415">{{cite journal |accessdate=2012-12-29 |language=en |author=Bartzokis G, Lu PH, Mintz J |title=Quantifying age-related myelin breakdown with MRI: novel therapeutic targets for preventing cognitive decline and Alzheimer's disease |journal=J. Alzheimers Dis. |volume=6 |issue=6 Suppl |pages=S53–9 |pmid=15665415 |doi= |url=|date=December 2004}}</ref><ref name="pmid18596894">{{cite journal |accessdate=2012-12-29 |language=en |author=Bartzokis G, Lu PH, Mintz J |title=Human brain myelination and beta-amyloid deposition in Alzheimer's disease |journal=Alzheimers Dement |volume=3 |issue=2 |pages=122–5 |pmid=18596894 |pmc=2442864 |doi=10.1016/j.jalz.2007.01.019 |url=|date=April 2007}}</ref>。 |
|||
從事某些益智活動的人們,罹患阿茲海默症的風險似乎較低,如[[閱讀]]、[[圖版遊戲]]、[[填字游戏]]、演奏[[樂器]],及從事日常[[社交|社交活動]]等<ref name="pmid16917199">{{vcite journal|vauthors=Stern Y|title=Cognitive reserve and Alzheimer disease|journal=Alzheimer Disease and Associated Disorders|volume=20|issue=2|pages=112–17|date=July 2006|pmid=16917199|doi=10.1097/01.wad.0000213815.20177.19|issn=0893-0341|month=}}</ref>。這點符合{{tsl|en|cognitive reserve|認知存量|}}假說,該假說認為有些生活經歷會增進神經功能的效能,並擴充個人的認知存量,進而延遲失智症的發生<ref name="pmid16917199" />。接受[[教育]]也會延遲阿茲海默症的發生,但並不會改變病程的長短<ref name="pmid19026089">{{vcite journal|vauthors=Paradise M, Cooper C, Livingston G|title=Systematic Review of the Effect of Education on Survival in Alzheimer's Disease|journal=International Psychogeriatrics|volume=21|issue=1|pages=25–32|year=2009|pmid=19026089|doi=10.1017/S1041610208008053|month=February}}</ref>。學習[[第二語言]]也有可能可以延遲疾病發生<ref>{{cite news|url=http://www.denverpost.com/ci_17427474|title=Speaking 2 Languages May Delay Getting Alzheimer's|last=Neergaard|first=Lauran|date=19 February 2011|publisher=The Denver Post|deadurl=no|agency=Associated Press|archive-url=https://web.archive.org/web/20140502013633/http://www.denverpost.com/ci_17427474|archive-date=2 May 2014}}</ref>。[[體能鍛鍊]]亦顯示可以降低阿茲海默症的風險<ref name="pmid19026089" />,且發生失智症的比率較低<ref>{{cite journal|title=Cognitive Reserve and the Prevention of Dementia: the Role of Physical and Cognitive Activities|date=September 2016|journal=Current Psychiatry Reports|issue=9|doi=10.1007/s11920-016-0721-2|volume=18|pages=85|pmc=4969323|pmid=27481112|vauthors=Cheng ST}}</ref>,另外也能減輕患者症狀嚴重程度<ref>{{cite journal|title=The effect of exercise interventions on cognitive outcome in Alzheimer's disease: a systematic review|url=https://www.cambridge.org/core/product/identifier/S1041610213001385/type/JOURNAL_ARTICLE|date=January 2014|journal=International Psychogeriatrics|issue=1|doi=10.1017/S1041610213001385|volume=26|pages=9–18|pmid=23962667|vauthors=Farina N, Rusted J, Tabet N}}</ref>。 |
|||
===飲食=== |
|||
[[氧化应激|氧化壓力]]和生物金屬失去[[稳态|體內平衡]]也可能是阿茲海默症病患產生病理變化的重要因子<ref name="pmid19075578">{{cite journal |accessdate=2012-12-29 |language=en |author=Su B, Wang X, Nunomura A, ''et al.'' |title=Oxidative stress signaling in Alzheimer's disease |journal=Curr Alzheimer Res |volume=5 |issue=6 |pages=525–32 |pmid=19075578 |pmc=2780015 |doi=10.2174/156720508786898451 |url=|date=December 2008}}</ref><ref name="pmid=19075578">{{cite journal |accessdate=2012-12-29 |language=en |author=Kastenholz B, Garfin DE, Horst J, Nagel KA |title=Plant metal chaperones: a novel perspective in dementia therapy |journal=Amyloid |volume=16 |issue=2 |pages=81–3 |year=2009 |pmid=20536399 |doi=10.1080/13506120902879392 |url=}}</ref>。 |
|||
<!--Diets --> |
|||
平時身體健康者、[[日本人]]、[[地中海飲食]]者顯示罹患阿茲海默症的機會較小<ref name="Hu2013">{{vcite journal|vauthors=Hu N, Yu JT, Tan L|title=Nutrition and the Risk of Alzheimer's Disease|journal=BioMed Research International|volume=2013|pmid=23865055|year=2013|doi=10.1155/2013/524820|type=Review|pmc=3705810}}</ref>。地中海飲食同時也能改善患病者的預後<ref>{{vcite journal|vauthors=Solfrizzi V, Panza F, Frisardi V|title=Diet and Alzheimer's disease risk factors or prevention: the current evidence|journal=Expert Review of Neurotherapeutics|volume=11|issue=5|pages=677–708|date=May 2011|pmid=21539488|doi=10.1586/ern.11.56}}</ref>。飲食含有高脂肪酸及簡單碳水化合物(simple carbohydrates,[[單醣]]或[[雙醣]]等)患病機率也較高<ref>{{vcite journal|vauthors=Kanoski SE, Davidson TL|title=Western diet consumption and cognitive impairment: links to hippocampal dysfunction and obesity|journal=Physiology & Behavior|volume=103|issue=1|pages=59–68|date=18 April 2011|pmid=21167850|pmc=3056912|doi=10.1016/j.physbeh.2010.12.003|type=Review}}</ref>。地中海飲食對心血管正面影響的機制也已有文獻發表<ref name="pmid18088206">{{vcite journal|vauthors=Solfrizzi V, Capurso C, D'Introno A|title=Lifestyle-related Factors in Predementia and Dementia Syndromes|journal=Expert Review of Neurotherapeutics|volume=8|issue=1|pages=133–58|year=2008|pmid=18088206|doi=10.1586/14737175.8.1.133|month=January}}</ref>。 |
|||
<!--Dietary components --> |
|||
阿茲海默症病患損失了70%負責產生[[去甲肾上腺素|正腎上腺素]]的[[藍斑核]]細胞, |
|||
飲食的配方與阿茲海默症間的關係目前仍不明朗,因為相關的研究結果沒有定論<ref name=Hu2013/>。有限證據顯示適量飲酒,與較低的阿茲海默症發生率相關,特別是紅酒<ref name=Hu2013 />。另有證據表明[[咖啡因]]可能為阿茲海默症的保護因子<ref name="pmid20182026">{{vcite journal|vauthors=Santos C, Costa J, Santos J, Vaz-Carneiro A, Lunet N|title=Caffeine intake and dementia: systematic review and meta-analysis|journal=Journal of Alzheimer's Disease|volume=20 Suppl 1|issue=|pages=S187–204|year=2010|pmid=20182026|doi=10.3233/JAD-2010-091387|url=}}</ref>。含有高量[[黄酮类化合物|黄酮类]]的食物,如[[可可]]、紅酒、茶,等,也可能與較低的阿茲海默症風險相關<ref>{{vcite journal | vauthors = Nehlig A | title = The neuroprotective effects of cocoa flavanol and its influence on cognitive performance | journal = British Journal of Clinical Pharmacology | volume = 75 | issue = 3 | pages = n/a–n/a | date = July 2012 | pmid = 22775434 | doi = 10.1111/j.1365-2125.2012.04378.x | type = Review | pmc=3575938}}</ref><ref>{{vcite journal | vauthors = Stoclet JC, Schini-Kerth V | title = [Dietary flavonoids and human health] | journal = Annales Pharmaceutiques Françaises | volume = 69 | issue = 2 | pages = 78–90 | date = March 2011 | pmid = 21440100 | doi = 10.1016/j.pharma.2010.11.004 }}</ref>。 |
|||
在[[新皮質]]和[[海馬迴]],正腎上腺素除了是神經傳導物質以外,在靜脈曲張處擴散也可以作為神經細胞、[[神經膠質細胞]]和血管周圍微環境的內源性抗發炎物<ref name="pmid20231476">{{cite journal |accessdate=2012-12-29 |language=en |first=MT |last=Heneka |authorlink= |coauthors=Nadrigny F, Regen T, Martinez-Hernandez A, Dumitrescu-Ozimek L, Terwel D, Jardanhazi-Kurutz D, Walter J, Kirchhoff F, Hanisch UK, Kummer MP. |year=2010 |month= |title=Locus ceruleus controls Alzheimer's disease pathology by modulating microglial functions through norepinephrine. |journal=Proc Natl Acad Sci U S A. |volume=107 |issue= |pages=6058–6063 |url=http://www.pnas.org.libproxy.ucl.ac.uk/content/107/13/6058.full.pdf |pmid=20231476 |doi=10.1073/pnas.0909586107}}</ref>,已有研究顯示正腎上腺素會刺激老鼠小神經膠質細胞,進而抑制小神經膠質細胞產生[[細胞激素]]和及吞噬β類澱粉蛋白質,由這些發現推測藍斑核退化可能是阿茲海默症病患大腦中β類澱粉蛋白質產生囤積的原因<ref name="pmid20231476"/>。 |
|||
<!--Vitamins and minerals --> |
|||
== 患病因素 == |
|||
目前沒有有力證據支持攝取[[維生素]]或[[礦物質]]對疾病有幫助,此部分已研究的物質包含維生素A<ref>{{vcite journal|vauthors=Ono K, Yamada M|title=Vitamin A and Alzheimer's disease|journal=Geriatrics & Gerontology International|volume=12|issue=2|pages=180–88|date=April 2012|pmid=22221326|doi=10.1111/j.1447-0594.2011.00786.x|type=Review}}</ref><ref>{{vcite journal|vauthors=Lerner AJ, Gustaw-Rothenberg K, Smyth S, Casadesus G|title=Retinoids for treatment of Alzheimer's disease|journal=BioFactors|volume=38|issue=2|pages=84–89|date=Mar–April 2012|pmid=22419567|doi=10.1002/biof.196}}</ref>、C<ref>{{vcite journal|vauthors=Heo JH, Lee KM|title=The possible role of antioxidant vitamin C in Alzheimer's disease treatment and prevention|journal=American Journal of Alzheimer's Disease & Other Dementias|volume=28|issue=2|pages=120–25|date=March 2013|pmid=23307795|doi=10.1177/1533317512473193|type=Review}}</ref><ref name="pmid16227450">{{vcite journal|vauthors=Boothby LA, Doering PL|title=Vitamin C and Vitamin E for Alzheimer's Disease|journal=The Annals of Pharmacotherapy|volume=39|issue=12|pages=2073–80|year=2005|pmid=16227450|doi=10.1345/aph.1E495|month=December}}</ref>、α-生育酚態的[[維生素E]]<ref name=":0">{{Cite journal|title=Vitamin E for Alzheimer's dementia and mild cognitive impairment|url=https://www.ncbi.nlm.nih.gov/pubmed/28418065|last=Farina|first=Nicolas|last2=Llewellyn|first2=David|date=2017|journal=The Cochrane Database of Systematic Reviews|doi=10.1002/14651858.CD002854.pub5|volume=4|pages=CD002854|issn=1469-493X|pmid=28418065|last3=Isaac|first3=Mokhtar Gad El Kareem Nasr|last4=Tabet|first4=Naji|via=}}</ref>、[[硒]]<ref>{{vcite journal|vauthors=Loef M, Schrauzer GN, Walach H|title=Selenium and Alzheimer's disease: a systematic review|journal=Journal of Alzheimer's Disease|volume=26|issue=1|pages=81–104|year=2011|pmid=21593562|doi=10.3233/JAD-2011-110414|type=Review}}</ref>、[[鋅]]<ref>{{vcite journal|vauthors=Loef M, von Stillfried N, Walach H|title=Zinc diet and Alzheimer's disease: a systematic review|journal=Nutritional Neuroscience|volume=15|issue=5|pages=2–12|date=1 September 2012|pmid=22583839|doi=10.1179/1476830512Y.0000000010|type=Review}}</ref><ref>{{cite journal|title=Zinc and Copper in Alzheimer's Disease|journal=Journal of Alzheimer's Disease|issue=1|doi=10.3233/JAD-150186|year=2015|volume=46|pages=89–92|type=Review|pmid=25835420|vauthors=Avan A, Hoogenraad TU}}</ref>、[[叶酸|葉酸]],以及B<sub>12</sub>等<ref>{{vcite journal|vauthors=Malouf R, Grimley Evans J|title=Folic Acid with or without Vitamin B<sub>12</sub> for the Prevention and Treatment of Healthy Elderly and Demented people|journal=The Cochrane Database of Systematic Reviews|issue=4|page=CD004514|year=2008|pmid=18843658|doi=10.1002/14651858.CD004514.pub2}}</ref>。一項證據品質中等的隨機分派研究指出,α-生育酚態的維生素E可以減緩認知功能下降的速度<ref name=":0" />;而葉酸及其他維生素B的臨床試驗則無法證明有同樣功能<ref>{{vcite journal|vauthors=Wald DS, Kasturiratne A, Simmonds M|title=Effect of Folic Acid, with or without other B vitamins, on Cognitive Decline: Meta-analysis of Randomized trials|journal=The American Journal of Medicine|volume=123|issue=6|pages=522–27.e2|date=June 2010|pmid=20569758|doi=10.1016/j.amjmed.2010.01.017}}</ref>。植物油及魚油中常見的Omega-3脂肪酸,以及[[二十二碳六烯酸]](DHA)對於改善阿茲海默症沒有已知助益<ref>{{vcite journal|vauthors=Cunnane SC, Chouinard-Watkins R, Castellano CA, Barberger-Gateau P|title=Docosahexaenoic acid homeostasis, brain aging and Alzheimer's disease: Can we reconcile the evidence?|journal=Prostaglandins, Leukotrienes, and Essential Fatty Acids|volume=88|issue=1|pages=61–70|date=January 2013|pmid=22575581|doi=10.1016/j.plefa.2012.04.006}}</ref><ref>{{cite journal|title=Omega-3 fatty acids for the treatment of dementia|date=April 2016|journal=The Cochrane Database of Systematic Reviews|doi=10.1002/14651858.CD009002.pub3|volume=4|pages=CD009002|pmid=27063583|vauthors=Burckhardt M, Herke M, Wustmann T, Watzke S, Langer G, Fink A}}</ref>。 |
|||
阿茲海默症受遗传因素的一定影響。根據調査显示,80歳以后15%的人有罹患痴呆性疾患的危险。親族中有阿茲海默症患者的場合患病的機率也相对要高。其中,更有13歲的年輕小女孩罹患阿茲海默症的紀錄。 |
|||
<ref>[http://dailynews.sina.com/bg/tw/twpolitics/bcc/20090912/1834663152.html 英國13歲女童患老人癡呆症]</ref> |
|||
<!--Alternative medicine --> |
|||
大規模調査显示多摄取[[蔬菜]]、魚虾類食物将减少患阿茲海默症的機率、肉類的过多摄取则会使得機率提高。 |
|||
[[姜黄素|薑黃]]在動物實驗中顯示對阿茲海默症有幫助,但截至2010年為止,尚無人體實驗證實有效<ref>{{vcite journal | vauthors = Hamaguchi T, Ono K, Yamada M | title = Curcumin and Alzheimer's disease |type=review | journal = CNS Neuroscience & Therapeutics | volume = 16 | issue = 5 | pages = 285–97 | date = October 2010 | pmid = 20406252 | doi = 10.1111/j.1755-5949.2010.00147.x | url = }}</ref>。[[银杏]]及大麻素目前也尚無有力證據支持其在失智症的效果<ref>{{vcite journal | vauthors = Birks J, Grimley Evans J | title = Ginkgo Biloba for Cognitive Impairment and Dementia | journal = The Cochrane Database of Systematic Reviews | issue = 1 | page = CD003120 | year = 2009 | pmid = 19160216 | doi = 10.1002/14651858.CD003120.pub3 }}</ref><ref name="pmid19370677">{{vcite journal | vauthors = Krishnan S, Cairns R, Howard R | title = Cannabinoids for the treatment of dementia | journal = The Cochrane Database of Systematic Reviews | volume = | issue = 2 | page = CD007204 | year = 2009 | pmid = 19370677 | doi = 10.1002/14651858.CD007204.pub2 | url = | editor1-last = Krishnan | editor1-first = Sarada }}</ref>,但內源性大麻素(endocannabinoids)似乎有一些證據顯示有所助益<ref name="pmid23108550">{{cite journal | vauthors = Bilkei-Gorzo A | title = The endocannabinoid system in normal and pathological brain ageing | journal = Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences | volume = 367 | issue = 1607 | pages = 3326–41 | date = December 2012 | pmid = 23108550 | pmc = 3481530 | doi = 10.1098/rstb.2011.0388 }}</ref>。 |
|||
==治療== |
|||
[[藍藻]]生物皆含有神經毒素[[β-甲氨基-L-丙氨酸]],β-甲氨基-L-丙氨酸已經被證實會對動物產生強烈的毒性,加速動物[[腦]][[神經]]退化、四肢肌肉萎縮等等,小量BMAA積累已能選擇性殺死從老鼠的神經元。藍藻門的生物包括[[髮菜]]、[[螺旋藻]]等等。香港中文大學呼籲大眾停止食用[[髮菜]],減輕患上阿茲海默症的風險。<ref>Greg Miller. Guam's Deadly Stalker: On the Loose Worldwide? ''Science'' '''July 2006''', ''28'' (313), 428-431. [http://dx.doi.org/10.1126/science.313.5786.428]</ref> |
|||
目前阿茲海默症尚無根本性治療,僅有一些症狀性治療,此類療法大多屬於[[和缓医疗|和緩醫療]]。現行治療可分為藥物治療、心理治療,以及照護品質。 |
|||
===藥物治療=== |
|||
另外曾有抽烟摄取[[尼古丁]]能减少阿茲海默症的发病機率之说,但在大規模的研究后現在这一说法被否定<ref name="活力藥師網"/>。 |
|||
[[File:Donepezil 1EVE.png|right|thumb|{{tsl|en|donepezil|愛憶欣|}}(donepezil)的3D{{tsl|en|molecular model|分子結構模型|}},本品屬於{{tsl|en|acetylcholinesterase inhibitor|乙醯膽鹼酯酶抑制劑|}},可用於改善阿茲海默症的症狀。]] |
|||
[[File:Memantine.svg|right|thumb|Upright|{{tsl|en|memantine|美金剛胺|}}的分子結構。]] |
|||
目前用於改善阿茲海默症認知障礙的藥物有五種,其中四種為{{tsl|en|acetylcholinesterase inhibitor|乙醯膽鹼酯酶抑制劑|}}({{tsl|en|tacrine|達可寧|}}、{{tsl|en|rivastigmine|憶思能|}}、{{tsl|en|galantamine|加蘭他敏|}}、{{tsl|en|donepezil|愛憶欣|}}),另外一種為{{tsl|en|NMDA receptor antagonist|NMDA受體拮抗劑|}}({{tsl|en|memantine|美金剛胺|}})。但這些藥物的效益都不大<ref name="Pres2012">{{vcite journal||author=Commission de la transparence|title=Médicaments de la maladie d'Alzheimer|journal=Prescrire International|volume=21|issue=128|page=150|date=June 2012|pmid=22822592|trans_title=Drugs for Alzheimer's disease: best avoided. No therapeutic advantage}}</ref><ref name="pmid16437430">{{vcite journal|vauthors=Birks J, Harvey RJ|title=Donepezil for dementia due to Alzheimer's disease|journal=The Cochrane Database of Systematic Reviews|issue=1|page=CD001190|date=25 January 2006|pmid=16437430|doi=10.1002/14651858.CD001190.pub2|editor1-last=Birks|editor1-first=Jacqueline}}</ref><ref name="Birks2015">{{cite journal|title=Rivastigmine for Alzheimer's disease|authorlink2=John Grimley Evans|date=April 2015|journal=The Cochrane Database of Systematic Reviews|issue=4|doi=10.1002/14651858.CD001191.pub3|pages=CD001191|pmid=25858345|vauthors=Birks JS, Grimley Evans J}}</ref>,且截至目前為止,仍沒有證據這些藥物能延緩或停止疾病的進程。 |
|||
阿茲海默症會降低膽鹼性神經元的活性<ref name="pmid8534419">{{vcite journal | vauthors = Geula C, Mesulam MM | title = Cholinesterases and the pathology of Alzheimer disease | journal = Alzheimer Disease and Associated Disorders | volume = 9 Suppl 2 | pages = 23–28 | year = 1995 | pmid = 8534419 | doi = 10.1097/00002093-199501002-00005 }}</ref>,而乙醯膽鹼酯酶抑制劑可以減緩[[乙酰胆碱|乙醯膽鹼]](ACh)的降解速率,藉此提升突觸間的乙酰胆碱濃度,已補足因膽鹼性神經元死亡而造成乙醯膽鹼濃度下降的現象<ref name="pmid11105732">{{vcite journal|vauthors=Stahl SM|title=The new cholinesterase inhibitors for Alzheimer's disease, part 2: illustrating their mechanisms of action|journal=The Journal of Clinical Psychiatry|volume=61|issue=11|pages=813–14|year=2000|pmid=11105732|doi=10.4088/JCP.v61n1101}}</ref>。目前此類藥品在輕度至中度的阿茲海默症的症狀控制上,已經證實有效<ref name="pmid16437532">{{vcite journal|vauthors=Birks J|title=Cholinesterase inhibitors for Alzheimer's disease|journal=The Cochrane Database of Systematic Reviews|issue=1|pages=CD005593|year=2006|pmid=16437532|doi=10.1002/14651858.CD005593|editor1-last=Birks|editor1-first=Jacqueline}}</ref><ref name="Birks2015" /><ref name=":1">{{Cite journal|title=Donepezil for dementia due to Alzheimer's disease|url=https://www.ncbi.nlm.nih.gov/pubmed/29923184|last=Birks|first=Jacqueline S.|last2=Harvey|first2=Richard J.|date=2018|journal=The Cochrane Database of Systematic Reviews|doi=10.1002/14651858.CD001190.pub3|volume=6|pages=CD001190|issn=1469-493X|pmid=29923184|via=}}</ref> ,有一些證據甚至表示重度患者使用也有效果<ref name=":1" />。{{tsl|en|mild cognitive impairment|輕度知能障礙|}}患者用藥並不能延遲阿茲海默症的發生<ref name="pmid18044984">{{vcite journal|vauthors=Raschetti R, Albanese E, Vanacore N, Maggini M|title=Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials|journal=PLoS Medicine|volume=4|issue=11|page=e338|year=2007|pmid=18044984|pmc=2082649|doi=10.1371/journal.pmed.0040338}}</ref>。此類藥物最常見的[[药物不良反应|副作用]]為[[恶心|噁心]]和[[呕吐|嘔吐]],兩者皆為膽鹼過量的副作用。約10–20%的患者用藥後會產生副作用,嚴重程度從輕度到中度皆有。如有此類問題,可以緩慢調降藥量來改善<ref>{{cite book|title=Applied therapeutics : the clinical use of drugs|first1=edited by Brian K. Alldredge ... [et|date=2013|publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins|isbn=978-1609137137|edition=10th|location=Baltimore|page=2385|last1=al.]}}</ref>。比較少見的副作用包含肌肉[[抽搐]]、[[心跳过缓|心搏過緩]]、[[食慾]]及體重下降,以及[[胃酸]]製造增加等等<ref name="pmid16437532"/>。 |
|||
=== 铝致病説 === |
|||
曾有学说认为摄取过量[[铝]][[离子]]是阿茲海默症原因之一,但是这一说法目前已不被採信<ref>{{cite web |url=http://alzheimers.org.uk/site/scripts/documents_info.php?documentID=99 |title=存档副本 |accessdate=2012年6月15日 |deadurl=yes |archiveurl=https://web.archive.org/web/20120311205419/http://alzheimers.org.uk/site/scripts/documents_info.php?documentID=99 |archivedate=2012年3月11日 |df= }}</ref>。 |
|||
[[谷氨酸|麩胺酸]]為興奮性[[神经递质|神經傳遞物質]],若在腦中含量過多可能會引起{{tsl|en|excitotoxicity|神經興奮性毒性反應|興奮性毒性反應}},使細胞因受體過度刺激而死亡。興奮性毒性反應存在於阿茲海默症、[[帕金森氏症]],以及[[多发性硬化症|多發性硬化症]]等神經性疾病中<ref name="pmid16424917">{{vcite journal | vauthors = Lipton SA | title = Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond | journal = Nature Reviews. Drug Discovery | volume = 5 | issue = 2 | pages = 160–70 | year = 2006 | pmid = 16424917 | doi = 10.1038/nrd1958 }}</ref>。{{tsl|en|Memantine|美金剛胺|}}為一種非競爭性{{tsl|en|NMDA receptor antagonist|NMDA受體拮抗劑|}},一開始被用於治療[[流行性感冒]],但後來發現它可以藉由抑制[[N-甲基-D-天門冬胺酸受體|NMDA受體]]來達到抑制麩胺酸系統的效果<ref name="pmid16424917" /><ref>{{cite web|url=https://www.nlm.nih.gov/medlineplus/druginfo/meds/a604006.html|title=Memantine|access-date=3 February 2010|date=4 January 2004|publisher=US National Library of Medicine (Medline)|archive-url=https://web.archive.org/web/20100222203921/https://www.nlm.nih.gov/medlineplus/druginfo/meds/a604006.html|archive-date=22 February 2010 |deadurl=no}}</ref>。後來的研究顯示美金剛胺對於阿茲海默症有些許效益<ref>{{cite journal | vauthors = McShane R, Areosa Sastre A, Minakaran N | title = Memantine for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 2 | pages = CD003154 | date = April 2006 | pmid = 16625572 | doi = 10.1002/14651858.CD003154.pub5 }}</ref>。本品已知的[[不良反應 (醫學)|不良反應]]包含偶爾產生輕微[[幻觉|幻覺]]、{{tsl|en|confusion|意識混亂|}}、[[頭暈|暈眩]]、[[頭痛]],以及[[疲勞]]<ref>{{cite web|url=http://www.frx.com/pi/namenda_pi.pdf |title=Namenda prescribing information |access-date=19 February 2008 |format=PDF |publisher={{tsl|en|Forest Pharmaceuticals||Forest Pharmaceuticals}} |archive-url=https://web.archive.org/web/20080227161413/http://www.frx.com/pi/namenda_pi.pdf |archive-date=27 February 2008 |deadurl=yes }} (primary source)<!-- also available at https://web.archive.org/web/*/http://www.frx.com/pi/namenda_pi.pdf --></ref>。美金剛胺與愛憶欣併用的效果統計上呈現顯著,但臨床效益不大<ref name="pmid18316756">{{vcite journal|vauthors=Raina P, Santaguida P, Ismaila A|title=Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline|journal=Annals of Internal Medicine|volume=148|issue=5|pages=379–97|year=2008|pmid=18316756|doi=10.7326/0003-4819-148-5-200803040-00009}}</ref>。 |
|||
阿茲海默症患者脑内检测出的铝离子浓度比正常人通常高出数十倍,这是阿茲海默症的成因还是导致的結果目前还不明。 |
|||
{{tsl|en|Atypical antipsychotic|非典型抗精神病藥|}}對於緩解患者的[[侵略 (社會科學)|攻擊性]]及[[思覺失調]]症狀具有一些效果,但同時此類藥物也會造成一些嚴重副作用,例如[[中風]]、[[錐體外症候群|動作障礙]],已及認知功能損傷等等<ref>{{vcite journal|vauthors=Ballard C, Waite J|title=The Effectiveness of Atypical Antipsychotics for the Treatment of Aggression and Psychosis in Alzheimer's Disease|journal=The Cochrane Database of Systematic Reviews|issue=1|page=CD003476|year=2006|pmid=16437455|doi=10.1002/14651858.CD003476.pub2|editor1-last=Ballard|editor1-first=Clive G}}</ref>。長期使用此類藥物可能會增加死亡風險<ref name="pmid19138567">{{vcite journal|vauthors=Ballard C, Hanney ML, Theodoulou M|title=The Dementia Antipsychotic Withdrawal Trial (DART-AD): Long-term Follow-up of a Randomised Placebo-controlled Trial|journal=Lancet Neurology|volume=8|issue=2|pages=151–17|date=9 January 2009|pmid=19138567|doi=10.1016/S1474-4422(08)70295-3|laysummary=http://www.physorg.com/news150695213.html}}</ref>,而對於精神症狀輕度至中度的長期服藥者,停藥似乎為安全的選擇<ref>{{cite journal | vauthors = Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, Christiaens T | title = Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia | journal = The Cochrane Database of Systematic Reviews | volume = 3 | issue = 3 | pages = CD007726 | date = March 2013 | pmid = 23543555 | doi = 10.1002/14651858.CD007726.pub2 }}</ref>。 |
|||
此説源于第二次世界大战後[[关岛]]驻扎的美軍患有老年痴呆的機率異常之高,经过调查后发现关岛[[地下水]]中铝离子的含量非常高,通过改为饮用雨水以及从其它岛屿提供的水后患病率马上急剧下降,由此得出铝致病说。另外日本[[紀伊半島]]地区阿茲海默症患病比率极高,其地下水中铝离子含量也极高,通过完善用水设备后患病率下降也是这一学说的根据。 |
|||
{{tsl|en|Huperzine A|石杉鹼甲|}}對改善認知功能似乎有正面影響,但目前仍需進一步研究證實其效果<ref>{{vcite journal | vauthors = Li J, Wu HM, Zhou RL, Liu GJ, Dong BR | title = Huperzine A for Alzheimer's disease | journal = The Cochrane Database of Systematic Reviews | issue = 2 | page = CD005592 | year = 2008 | pmid = 18425924 | doi = 10.1002/14651858.CD005592.pub2 | url = http://www2.cochrane.org/reviews/en/ab005592.html | editor1-last = Wu | editor1-first = Hong Mei | deadurl = no | archive-url = https://web.archive.org/web/20110317114141/http://www2.cochrane.org/reviews/en/ab005592.html | archive-date = 17 March 2011 | df = dmy-all }}</ref>。 |
|||
根據牛津大學神經病理學院三名教授的聯合研究報告,已更正鋁有害腦部之說法。這項研究對八十名老人癡呆症患者腦組織中作切片檢查,證實鋁並未存於病患腦中。以往認定鋁元素與老人癡呆症有關,是因傳統製作腦切片及染色過程中,鋁元素常是必須用品,所以檢查結果有鋁元素,而牛津大學教授所使用的核子電鏡,卻是不須經過染色步驟即可進行分析切片。原来认为血液到脑部时通过[[血脑屏障]]时铝离子无法到达大脑,如今发现这种看法是错误的。<ref>{{cite web | url = http://alzheimers.org.uk/site/scripts/documents_info.php?documentID=99 | title = Aluminium and Alzheimer's disease | accessdate = 2012-06-15 | deadurl = yes | archiveurl = https://web.archive.org/web/20120311205419/http://alzheimers.org.uk/site/scripts/documents_info.php?documentID=99 | archivedate = 2012年3月11日 | df = }}</ref> |
|||
== |
===心理治療=== |
||
[[社会心理学|社會心理]]治療可用於輔助藥物治療,分為行為性、情緒性、認知性、刺激性等介入方式。但此類治療的效度無法測量,且此類研究的研究對象大多收錄了所有失智症,鮮少明確針對阿茲海默症<ref name="pracGuideAPA">{{vcite journal | vauthors = Rabins PV, Blacker D, Rovner BW | title = American Psychiatric Association practice guideline for the treatment of patients with Alzheimer's disease and other dementias | journal = The American Journal of Psychiatry | volume = 164 | issue = 12 Suppl | pages = 5–56 | date = December 2007 | pmid = 18340692 | author9 = Steering Committee on Practice Guidelines }}</ref>。 |
|||
目前沒有治愈阿茲海默症的方法,現有的治療本質上仍然是治標不治本,它提供了相對比較小的症狀改善的好處。目前的治療可分為藥物、心理和護理。 |
|||
=== 药物疗法 === |
|||
五種藥物是目前用於治療阿茲海默症的認知問題:其中四種是[[乙酰膽鹼酯酶]]抑制劑(他克林,tacrine、利凡斯的明,rivastigmine、加蘭他敏,galantamine和多奈哌齊,donepezil)以及其他(美金剛,memantine)則是[[N-甲基-D-天門冬胺酸受體]](NMDA受體)拮抗劑。 |
|||
{{tsl|en|Behavior modification|行為調整|行為治療}}乃是藉由識別問題行為的前因及結果,進而試圖減少之。此類治療雖然無法改善整體功能<ref name="pmid16323385">{{vcite journal|vauthors=Bottino CM, Carvalho IA, Alvarez AM, et al|title=Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study|journal=Clinical Rehabilitation|volume=19|issue=8|pages=861–69|year=2005|pmid=16323385|doi=10.1191/0269215505cr911oa}}</ref>,但可以減少一些特定的問題行為,例如[[尿失禁]]<ref name="pmid11342679">{{vcite journal | vauthors = Doody RS, Stevens JC, Beck C | title = Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology | journal = Neurology | volume = 56 | issue = 9 | pages = 1154–66 | year = 2001 | pmid = 11342679 | doi = 10.1212/WNL.56.9.1154 }}</ref>。但目前對於遊走(wandering)等其他問題,並沒有足夠實證顯示其效果<ref name="pmid17253573">{{vcite journal | vauthors = Hermans DG, Htay UH, McShane R | title = Non-pharmacological interventions for wandering of people with dementia in the domestic setting | journal = The Cochrane Database of Systematic Reviews | issue = 1 | page = CD005994 | year = 2007 | pmid = 17253573 | doi = 10.1002/14651858.CD005994.pub2 }}</ref><ref name="pmid17096455">{{vcite journal | vauthors = Robinson L, Hutchings D, Dickinson HO | title = Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review | journal = International Journal of Geriatric Psychiatry | volume = 22 | issue = 1 | pages = 9–22 | year = 2007 | pmid = 17096455 | doi = 10.1002/gps.1643 }}</ref>。音樂治療可能對於減少行為性或心理性症狀有些效果<ref>{{cite journal |authors=Abraha I, Rimland JM, Trotta FM, Dell'Aquila G, Cruz-Jentoft A, Petrovic M, Gudmundsson A, Soiza R, O'Mahony D, Guaita A, Cherubini A |title=Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series |journal=BMJ Open |date=16 March 2017 |volume=7 |issue=3 |page=e012759 |doi=10.1136/bmjopen-2016-012759 |pmid=28302633 |pmc=5372076 }}</ref>。 |
|||
目前使用這些藥物的效果大多還不理想。 |
|||
==== 乙醯膽鹼酶抑制劑 ==== |
|||
{{le|乙醯膽鹼酶抑制劑|Acetylcholinesterase}},2006年[[美國食品和藥物管理局]]批准多奈哌齊({{tsl|en|Donepezil|Donepezil}},愛憶欣)用於治療輕度、中度和重度的阿茲海默症。 |
|||
情緒導向治療包括{{tsl|en|reminiscence therapy|懷舊療法|}}、{{tsl|en|validation therapy|確認療法|}}、支持性[[心理治療]]、 {{tsl|en|sensory integration therapy|感官統合治療|感官統合}}(或稱為{{tsl|en|snoezelen|多感官治療|}})和{{tsl|en|simulated presence therapy|情境模擬治療|}}。一份[[考科藍]]的回顧性文章認為此類療法並無足夠實證支持效果<ref>{{cite journal | vauthors = Chung JC, Lai CK, Chung PM, French HP | title = Snoezelen for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 4 | pages = CD003152 | date = 2002 | pmid = 12519587 | doi = 10.1002/14651858.CD003152 }}</ref>。 支持性心理治療的正式學術研究相當少,但有些治療者認為對於改善病人的病感有些許效果<ref name="pracGuideAPA"/>。懷舊療法的做法是與病患引導病人回憶過去的經驗,治療者會反覆藉由照片、日常用品、音樂、錄音檔,或是病患熟悉的事物,引導病人回憶並組織過去的經驗。懷舊療法可以個別進行或以小組模式進行。一份2018年的回顧性文章認為懷舊療法的一致性不足,且對象規模過小、各團體差異過大,以致不足以彰顯其臨床意義<ref>{{cite journal |last1=Woods |first1=B |last2=O'Philbin |first2=L |last3=Farrell |first3=EM |last4=Spector |first4=AE |last5=Orrell |first5=M |title=Reminiscence therapy for dementia. |journal=The Cochrane Database of Systematic Reviews |date=1 March 2018 |volume=3 |pages=CD001120 |doi=10.1002/14651858.CD001120.pub3 |pmid=29493789}}</ref>。情境模擬治療的理論是建基於[[依附理論]]上,治療者會播放病患熟悉的聲音。此療法在改善病患的{{tsl|en|challenging behaviour|挑釁行為|}}有部分證據<ref name="pmid19023729">{{vcite journal | vauthors = Zetteler J | title = Effectiveness of simulated presence therapy for individuals with dementia: a systematic review and meta-analysis | journal = Aging & Mental Health | volume = 12 | issue = 6 | pages = 779–85 | date = November 2008 | pmid = 19023729 | doi = 10.1080/13607860802380631 }}</ref>。最後,確認療法是基於接受患者所感受到的真實和個人信念,而感官統合療法則以刺激訓練患者的感知為目標。目前沒有證據支持這些療法是否有效<ref name="pmid12917907">{{vcite journal | vauthors = Neal M, Briggs M | title = Validation therapy for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 3 | page = CD001394 | year = 2003 | pmid = 12917907 | doi = 10.1002/14651858.CD001394 | editor1-last = Neal | editor1-first = Martin }}</ref><ref name="pmid12519587">{{vcite journal | vauthors = Chung JC, Lai CK, Chung PM, French HP | title = Snoezelen for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 4 | page = CD003152 | year = 2002 | pmid = 12519587 | doi = 10.1002/14651858.CD003152 | editor1-last = Chung | editor1-first = Jenny CC }} (up to date as of 2009)</ref>。 |
|||
研究表明胆碱酯酶阻断剂可减轻阿茲海默症患者的精神症状。日本Eisai株式会社研发的[[乙酰胆碱]]分解酵素阻断剂,作为認知改善药物被用于治疗阿茲海默症。 |
|||
認知導向治療的目標包含協助病人恢復現實定向(reality orientation)以及{{tsl|en|Rehabilitation (neuropsychology)|復健 (神經心理學)|認知功能再訓練}}(cognitive retraining)。現實定向的做法是提供病人當下的人、事、時、地、物等現實資訊,以協助病人了解其環境。認知功能再訓練則旨在協助病人改善其心智功能。上述兩者對於改善認知能力都有一些效果<ref name="pmid17636652">{{vcite journal | vauthors = Spector A, Orrell M, Davies S, Woods B | title = Withdrawn: reality orientation for dementia | journal = The Cochrane Database of Systematic Reviews | issue = 3 | page = CD001119 | year = 2000 | pmid = 17636652 | doi = 10.1002/14651858.CD001119.pub2 | editor1-last = Spector | editor1-first = Aimee E }}</ref><ref name="pmid12948999">{{vcite journal | vauthors = Spector A, Thorgrimsen L, Woods B | title = Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial | journal = The British Journal of Psychiatry | volume = 183 | issue = 3 | pages = 248–54 | year = 2003 | pmid = 12948999 | doi = 10.1192/bjp.183.3.248 }}</ref>,雖然在部分研究中,這些效果短暫的,負面效果如使患者感到沮喪也曾被提出<ref name="pracGuideAPA"/>。 |
|||
此外针对阿茲海默症伴有的失眠、易怒、幻覺、妄想等「周边症状」,通常投与適宜対症的药剂如[[安眠药]]、抗精神病药物、抗[[癫痫]]药物、抗[[抑郁症]]药物等。 |
|||
刺激導向治療(Stimulation-oriented treatments)包括以[[藝術治療|藝術]]、[[音樂治療|音樂]]、{{tsl|en|Animal-assisted therapy|寵物治療|寵物}}、[[物理治療|運動]]或其他任何娛樂活動來進行治療。刺激可以適當地協助患者改善行為、心情和少部分的功能。雖然如此,這些治療提供的支持除了其本身的效果外,患者習慣的改變也是同等重要的<ref name="pracGuideAPA"/>。非侵入性腦刺激和侵入性腦刺激在阿茲海默症的效用目前還不明瞭<ref name=ChangLane2018>{{cite journal|last1=Chang|first1=Chun-Hung|last2=Lane|first2=Hsien-Yuan|last3=Lin|first3=Chieh-Hsin|title=Brain Stimulation in Alzheimer's Disease|journal=Frontiers in Psychiatry|volume=9|year=2018|issn=1664-0640|doi=10.3389/fpsyt.2018.00201|pmc=5992378|pmid=29910746}}{{CC-notice|cc=by4|url=https://www.frontiersin.org/articles/10.3389/fpsyt.2018.00201/full|author(s)=Chun-Hung Chang, Hsien-Yuan Lane, and Chieh-Hsin Lin}}</ref>。 |
|||
==== NMDA受體拮抗劑 ==== |
|||
這類藥物目前僅有memantine一種,許可適應症為中重度及重度阿茲海默症。 |
|||
=== |
===醫療照護=== |
||
由於阿茲海默症無法治癒,且會逐漸使患者無法自理,因此照護實質上是治療的核心,在整個疾病進程中必須小心處理。在疾病早期,改善居住環境和生活模式可以增進[[病人安全]],並減少照護者的負擔<ref name="pmid11220813">{{vcite journal|vauthors=Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW |title=A Randomized, Controlled Trial of a Home Environmental Intervention: Effect on Efficacy and Upset in Caregivers and on Daily Function of Persons with Dementia |journal=The Gerontologist |volume=41 |issue=1 |pages=4–14 |date=1 February 2001 |pmid=11220813 |doi=10.1093/geront/41.1.4}}</ref><ref name="pmid15860476">{{vcite journal | vauthors = Gitlin LN, Hauck WW, Dennis MP, Winter L | title = Maintenance of Effects of the Home Environmental Skill-building Program for Family Caregivers and Individuals with Alzheimer's Disease and Related Disorders | journal = The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences | volume = 60 | issue = 3 | pages = 368–74 | year = 2005 | pmid = 15860476 | doi = 10.1093/gerona/60.3.368 | month = March }}</ref>,實務上包括讓患者的生活作息符合固定簡單的模式、使用安全防護裝置、在居家物品上做標示(用以提示患者)或使用特殊設計的生活用具<ref name="pracGuideAPA" /><ref>{{cite web|url=http://www.alz.org/Health/Treating/agitation.asp|title=Treating Behavioral and Psychiatric Symptoms|year=2006|access-date=25 September 2006|publisher=Alzheimer's Association|archive-url=https://web.archive.org/web/20060925112503/http://www.alz.org/Health/Treating/agitation.asp|archive-date=25 September 2006}}</ref><ref name="pmid15297089">{{vcite journal | vauthors = Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A | title = Visual Contrast Enhances Food and Liquid Intake in Advanced Alzheimer's Disease | journal = Clinical Nutrition (Edinburgh, Scotland) | volume = 23 | issue = 4 | pages = 533–38 | year = 2004 | pmid = 15297089 | doi = 10.1016/j.clnu.2003.09.015 }}</ref>。若有進食問題,則須將食物切成小塊或甚至做成泥狀<ref>{{cite book|author=Dudek, Susan G.|title=Nutrition Essentials for Nursing Practice|publisher=Lippincott Williams & Wilkins|location=Hagerstown, Maryland|year=2007|page=360|isbn=0-7817-6651-6|url=https://books.google.com/?id=01zo6yf0IUEC&pg=PA360&dq=alzheimer%27s+chew|access-date=19 August 2008}}</ref>;當出現[[吞嚥障礙]]時,則可能需使用{{tsl|en|feeding tube|餵食管|}},對於這樣的患者,照護者和家人必須仔細考量藥物療效和餵食與否等倫理議題<ref name="pmid16415742">{{vcite journal | vauthors = Dennehy C | title = Analysis of Patients' Rights: Dementia and PEG Insertion | journal = British Journal of Nursing | volume = 15 | issue = 1 | pages = 18–20 | year = 2006 | pmid = 16415742 | doi=10.12968/bjon.2006.15.1.20303}}</ref><ref name="pmid16556924">{{vcite journal | vauthors = Chernoff R | title = Tube Feeding Patients with Dementia | journal = Nutrition in Clinical Practice | volume = 21 | issue = 2 | pages = 142–46 | year = 2006 | pmid = 16556924 | doi = 10.1177/0115426506021002142 | month = April }}</ref>。無論是哪個階段的阿茲海默症的患者,通常都不需要身體拘束,雖然在少數狀況下,為了保護患者或照護者仍必須執行拘束<ref name="pracGuideAPA" />。 |
|||
[[神经元]]保护剂可以阻斷[[穀氨酸]]的兴奋毒性(excitotoxicity),藉此減緩生活技能的日漸喪失,也是目前唯一治療中、重度失智症的藥物。 |
|||
當疾病逐漸惡化,各式病症也會逐漸出現如{{tsl|en|dental disease|牙科疾病|口腔或牙科疾病}}、[[褥疮|褥瘡]]、[[營養不良]]、[[衛生]]問題、呼吸道感染」皮膚感染、眼感染等。小心的照護管理能避免上述問題產生,但若真的發生了,則需要專業的治療<ref name="pmid10369823">{{vcite journal | vauthors = Gambassi G, Landi F, Lapane KL, Sgadari A, Mor V, Bernabei R | title = Predictors of Mortality in Patients with Alzheimer's Disease Living in Nursing Homes | journal = Journal of Neurology, Neurosurgery, and Psychiatry | volume = 67 | issue = 1 | pages = 59–65 | year = 1999 | pmid = 10369823 | pmc = 1736445 | doi = 10.1136/jnnp.67.1.59 | month = July }}</ref><ref>Medical issues: |
|||
==== 成纤维细胞修复因子(bFGF) ==== |
|||
有报道称bFGF对人诱导的痴呆老鼠模型有一定的治疗作用,但没有临床报告。 |
|||
*{{vcite journal | vauthors = Head B | title = Palliative Care for Persons with Dementia | journal = Home Healthcare Nurse | volume = 21 | issue = 1 | pages = 53–60; quiz 61 | year = 2003 | pmid = 12544465 | doi = 10.1097/00004045-200301000-00012 | month = January }} |
|||
=== 其他的治療法 === |
|||
*{{vcite journal | vauthors = Friedlander AH, Norman DC, Mahler ME, Norman KM, Yagiela JA | title = Alzheimer's Disease: Psychopathology, Medical Management and Dental Implications | journal = Journal of the American Dental Association | volume = 137 | issue = 9 | pages = 1240–51 | year = 2006 | pmid = 16946428 | month = September }} |
|||
通过散步等改善昼夜生活节奏,将有纪念意义的照片纪念品等放置在病人旁边给予安心感等药物以外的手段也被认为对患者的失眠、不安等症状有效。 |
|||
*{{vcite journal | vauthors = Belmin J | title = Practical Guidelines for the Diagnosis and Management of Weight Loss in Alzheimer's Disease: A Consensus from Appropriateness Ratings of a Large Expert Panel | journal = The Journal of Nutrition, Health & Aging | volume = 11 | issue = 1 | pages = 33–37 | year = 2007 | pmid = 17315078 }} |
|||
*{{vcite journal | vauthors = McCurry SM, Gibbons LE, Logsdon RG, Vitiello M, Teri L | title = Training Caregivers to Change the Sleep Hygiene Practices of Patients with Dementia: The NITE-AD Project | journal = Journal of the American Geriatrics Society | volume = 51 | issue = 10 | pages = 1455–60 | year = 2003 | pmid = 14511168 | doi = 10.1046/j.1532-5415.2003.51466.x | month = October }} |
|||
*{{vcite journal | vauthors = Perls TT, Herget M | title = Higher Respiratory Infection Rates on an Alzheimer's Special Care Unit and successful intervention | journal = Journal of the American Geriatrics Society | volume = 43 | issue = 12 | pages = 1341–44 | year = 1995 | pmid = 7490383 | month = December | doi=10.1111/j.1532-5415.1995.tb06611.x}}</ref>。在疾病的最末期,治療著重於在患者死亡前緩解其痛楚,通常會需要[[和缓医疗|緩和醫療]]的協助<ref name="pmid12854952">{{vcite journal | vauthors = Shega JW, Levin A, Hougham GW | title = Palliative Excellence in Alzheimer Care Efforts (PEACE): A Program Description | journal = Journal of Palliative Medicine | volume = 6 | issue = 2 | pages = 315–20 | year = 2003 | pmid = 12854952 | doi = 10.1089/109662103764978641 }}</ref>。 |
|||
==預後== |
|||
2018年五月的文獻顯示,[[地中海飲食]]有可能減緩阿茲海默症的病程,甚至降低引發阿茲海默症的可能。<ref name="National Institutes of Health (NIH) 2018">{{cite web | title=Mediterranean diet may slow development of Alzheimer’s disease | website=National Institutes of Health (NIH) | date=2018-05-14 | url=https://www.nih.gov/news-events/nih-research-matters/mediterranean-diet-may-slow-development-alzheimers-disease | access-date=2018-05-17}}</ref> |
|||
[[File:Alzheimer and other dementias world map - DALY - WHO2004.svg|thumb|upright=1.2|2004年阿茲海默症與其他失智患者每100,000人的[[失能調整生命年]]。 |
|||
{{colbegin}} |
|||
{{legend|#b3b3b3|無資料}} |
|||
{{legend|#ffff65|≤ 50}} |
|||
{{legend|#fff200|50–70}} |
|||
{{legend|#ffdc00|70–90}} |
|||
{{legend|#ffc600|90–110}} |
|||
{{legend|#ffb000|110–130}} |
|||
{{legend|#ff9a00|130–150}} |
|||
{{legend|#ff8400|150–170}} |
|||
{{legend|#ff6e00|170–190}} |
|||
{{legend|#ff5800|190–210}} |
|||
{{legend|#ff4200|210–230}} |
|||
{{legend|#ff2c00|230–250}} |
|||
{{legend|#cb0000|≥ 250}} |
|||
{{colend}}]] |
|||
阿茲海默症早期十分難診斷,通常要到認知障礙影響到日常生活後才會確診,雖然此時患者可能仍能獨立生活。患者的症狀會由輕度的認知功能問題(例如記憶力衰退)開始逐漸惡化,到疾病後期完全不可能獨自生活<ref name="pmid10653284"/>。 |
|||
阿茲海默症患者的[[预期寿命|預期壽命]]較短<ref name=Za2009>{{cite journal | vauthors = Zanetti O, Solerte SB, Cantoni F | title = Life expectancy in Alzheimer's disease (AD) | journal = Archives of Gerontology and Geriatrics | volume = 49 Suppl 1 | pages = 237–43 | date = 2009 | pmid = 19836639 | doi = 10.1016/j.archger.2009.09.035 }}</ref>,診斷後的預期餘命約三到十年<ref name=Za2009/>,少於3%的人能活超過14年<ref name="pmid7793228">{{vcite journal | vauthors = Mölsä PK, Marttila RJ, Rinne UK | title = Long-Term Survival and Predictors of Mortality in Alzheimer's Disease and Multi-Infarct Dementia | journal = Acta Neurologica Scandinavica | volume = 91 | issue = 3 | pages = 159–64 | year = 1995 | pmid = 7793228 | month = March | doi=10.1111/j.1600-0404.1995.tb00426.x}}</ref>。會造成存活年數顯著減少的特徵包括認知障礙嚴重度增加、生活功能減退、曾經跌倒和神經學檢查出現問題。其他共病如[[心血管疾病]]、[[糖尿病]]、曾經[[酗酒]]都和存活年數減少有關<ref name="pmid8757016">{{vcite journal | vauthors = Bowen JD, Malter AD, Sheppard L | title = Predictors of Mortality in Patients Diagnosed with Probable Alzheimer's Disease | journal = Neurology | volume = 47 | issue = 2 | pages = 433–39 | year = 1996 | pmid = 8757016 | doi = 10.1212/wnl.47.2.433 }}</ref><ref name="pmid15068977">{{vcite journal | vauthors = Larson EB, Shadlen MF, Wang L | title = Survival after Initial Diagnosis of Alzheimer Disease | journal = Annals of Internal Medicine | volume = 140 | issue = 7 | pages = 501–09 | year = 2004 | pmid = 15068977 | doi=10.7326/0003-4819-140-7-200404060-00008}}</ref><ref name="pmid7792352">{{vcite journal | vauthors = Jagger C, Clarke M, Stone A | title = Predictors of Survival with Alzheimer's Disease: A Community-based Study | journal = Psychological Medicine | volume = 25 | issue = 1 | pages = 171–77 | year = 1995 | pmid = 7792352 | doi = 10.1017/S0033291700028191 | month = January }}</ref>。雖然越年輕時就診斷的患者有越長的存活年數,但事實上年輕的患者相對於健康族群來說壽命較短<ref name="pmid12580712">{{vcite journal | vauthors = Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M | title = Functional Transitions and Active Life Expectancy Associated with Alzheimer Disease | journal = Archives of Neurology | volume = 60 | issue = 2 | pages = 253–59 | year = 2003 | pmid = 12580712 | doi = 10.1001/archneur.60.2.253 | month = February }}</ref> 。男性的預後也較女性差<ref name="pmid7793228" /><ref name="pmid15883266">{{vcite journal | vauthors = Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST | title = Alzheimer Disease and Mortality: A 15-year Epidemiological Study | journal = Archives of Neurology | volume = 62 | issue = 5 | pages = 779–84 | year = 2005 | pmid = 15883266 | doi = 10.1001/archneur.62.5.779 | month = May }}</ref>。 |
|||
== 相關疾病 == |
|||
*[[朊毒體|普利昂疾病]] |
|||
*[[帕金森氏症]] |
|||
*[[腦硫脂]] |
|||
*[[異染性腦白質退化症]](較高水平腦硫脂) |
|||
[[肺炎]]和[[脱水|脫水]]是最常造成阿茲海默症患者立即死亡的原因;相較於一般人,阿茲海默症患者因癌症死亡的比率較少<ref name="pmid15883266" />。 |
|||
== 注釋 == |
|||
{{ |
{{clear}} |
||
== |
==流行病學== |
||
{| class="wikitable" style="float:right; text-align:center;" |
|||
{{Reflist|2}} |
|||
|+65歲以上年長者的發生率<ref name="pmid17727890"/> |
|||
|- |
|||
! 年齡 !! 年發生率(每千人) |
|||
|- |
|||
!65–69 |
|||
| 3 |
|||
|- |
|||
!70–74 |
|||
| 6 |
|||
|- |
|||
!75–79 |
|||
| 9 |
|||
|- |
|||
!80–84 |
|||
|23 |
|||
|- |
|||
!85–89 |
|||
|40 |
|||
|- |
|||
!90– <!-- The nonbreaking spaces to the left of this comment make the numbers line up properly. --> |
|||
|69 |
|||
|} |
|||
阿茲海默症的[[流行病学|流行病學]]研究主要著重在[[患病率|盛行率]]和[[发病率|發生率]]上:盛行率指的是某種疾病在任一時間點占群體總人數的比例;發生率則是指特定時期內某人群新發生某一疾病的比率。 |
|||
==參考文獻== |
|||
{{reflisth}} |
|||
*Huntley, J., Bor, D., Hampshire, A., Owen, A., & Howard, R. (2011). Working memory task performance and chunking in early alzheimer's disease. British Journal of Psychiatry, 198(5), 398-403 |
|||
{{reflistf}} |
|||
在發生率方面,[[纵向研究|縱貫性]][[队列研究|世代研究]](追蹤一群無疾病人口的發病比率)指出,每年失智症發生風險約為1-1.5%,而其中阿茲海默症的風險則為0.5-0.8%<ref name="pmid17727890">{{vcite journal | vauthors = Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC | title = Incidence and subtypes of dementia in three elderly populations of central Spain | journal = Journal of the Neurological Sciences | volume = 264 | issue = 1–2 | pages = 63–72 | year = 2008 | pmid = 17727890 | doi = 10.1016/j.jns.2007.07.021 | month = January }}</ref><ref name="pmid12028245">{{vcite journal | vauthors = Di Carlo A, Baldereschi M, Amaducci L | title = Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study | journal = Journal of the American Geriatrics Society | volume = 50 | issue = 1 | pages = 41–48 | year = 2002 | pmid = 12028245 | doi = 10.1046/j.1532-5415.2002.50006.x | month = January }}</ref> 。這代表在每年新發生的失智症中,有幾乎一半是阿茲海默症。高齡是阿茲海默症的主要風險因子,本病在每個年齡層的發生率不同,年齡越大者發生風險越高。65歲以上的長者,每五年的罹病風險就會增加一倍<ref name="pmid17727890"/><ref name="pmid12028245"/>。除年齡外,阿茲海默症的發生率還存在性別差異,女性的發生率較男性為高,特別是85歲以上的年長女性<ref name="pmid12028245"/><ref>{{vcite journal | vauthors = Andersen K, Launer LJ, Dewey ME | title = Gender Differences in the Incidence of AD and Vascular Dementia: The EURODEM Studies. EURODEM Incidence Research Group | journal = Neurology | volume = 53 | issue = 9 | pages = 1992–97 | year = 1999 | pmid = 10599770 | month = December | doi = 10.1212/wnl.53.9.1992 }}</ref>。在[[美国|美國]],非拉丁裔白人死於阿茲海默症的風險,比起非裔高出了26%,更比拉丁裔高出了30%<ref>Tejada-Vera B. (2013). [https://purl.fdlp.gov/GPO/gpo41882 Mortality from Alzheimer's Disease in the United States: Data for 2000 and 2010.] Hyattsville, MD: [[美国卫生及公共服务部|U.S. Department of Health and Human Services]], [[美国疾病控制与预防中心|Centers for Disease Control and Prevention]], {{tsl|en|National Center for Health Statistics||National Center for Health Statistics}}.</ref>。 |
|||
==延伸閱讀== |
|||
[[File:Alzheimer's disease and other dementias world map-Deaths per million persons-WHO2012.svg|thumb|left|upright=1.3|2012年每百萬人口因失智症而死亡的人數 {{refbegin|3}}{{legend|#ffff20|0–4}}{{legend|#ffe820|5–8}}{{legend|#ffd820|9–10}}{{legend|#ffc020|11–13}}{{legend|#ffa020|14–17}}{{legend|#ff9a20|18–24}}{{legend|#f08015|25–45}}{{legend|#e06815|46–114}}{{legend|#d85010|115–375}}{{legend|#d02010|376–1266}}{{refend}}]] |
|||
阿茲海默症的盛行率取決於許多因素,包括當地患者的存活率。由於阿茲海默症的發生率隨年齡增加,考量當地人口的平均年齡是相當重要的。美國的阿茲海默症的總人口盛行率和65–74歲的族群盛行率皆為1.6%,但在75–84歲的族群盛行率則為19%,85歲以上的族群更達到42%<ref>2000 U.S. estimates: |
|||
* {{vcite journal | vauthors = Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA | title = Alzheimer Disease in the US population: Prevalence Estimates Using the 2000 census | journal = Archives of Neurology | volume = 60 | issue = 8 | pages = 1119–22 | year = 2003 | pmid = 12925369 | doi = 10.1001/archneur.60.8.1119 | month = August }} |
|||
* {{cite web|title=Profiles of General Demographic Characteristics, 2000 Census of Population and Housing, United States|year=2001|publisher=U.S. Census Bureau|url=https://www.census.gov/prod/cen2000/dp1/2kh00.pdf|format=PDF|access-date=27 August 2008|archive-url=https://web.archive.org/web/20080819203118/http://www.census.gov/prod/cen2000/dp1/2kh00.pdf|archive-date=19 August 2008 |deadurl=no}}</ref>。低度開發地區的盛行率也因此較低<ref name="pmid16360788"/>。[[世界卫生组织|世界衛生組織]]估計2005年全球的失智症盛行率為0.379%,2015年會增加到0.441%,並在2030年達到0.556%<ref name="isbn9789241563369">{{cite book|last=World Health Organization|title=Neurological Disorders: Public Health Challenges|publisher=World Health Organization|year=2006|location=Switzerland|pages=204–07|url=http://www.who.int/mental_health/neurology/neurodiso/en/index.html|isbn=978-92-4-156336-9|deadurl=no|archive-url=https://web.archive.org/web/20100210144936/http://www.who.int/mental_health/neurology/neurodiso/en/index.html|archive-date=10 February 2010}}</ref>;其他研究也有類似的結論<ref name="pmid16360788">{{vcite journal | vauthors = Ferri CP, Prince M, Brayne C, Brodaty H | title = Global Prevalence of Dementia: A Delphi Consensus Study | journal = Lancet | volume = 366 | issue = 9503 | pages = 2112–17 | year = 2005 | pmid = 16360788 | pmc = 2850264 | doi = 10.1016/S0140-6736(05)67889-0 | month = December }}</ref>。另一項研究估計2006年全球約有0.40%(範圍從0.17到0.89%;實際人數約2660萬人,範圍從1140萬到5940萬人)的人口受阿茲海默症的影響,在2050年以前,盛行率會是現在的三倍,實際人數則會高達四倍<ref name="Brookmeyer2007">2006 prevalence estimate: |
|||
* {{vcite journal | vauthors = Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM | title = Forecasting the global burden of Alzheimer's disease | journal = Alzheimer's & Dementia | volume = 3 | issue = 3 | pages = 186–91 | year = 2007 | pmid = 19595937 | doi = 10.1016/j.jalz.2007.04.381 | url = http://works.bepress.com/cgi/viewcontent.cgi?article=1022&context=rbrookmeyer | month = July | access-date = 18 June 2008 | deadurl = no | archive-url = https://web.archive.org/web/20081207025403/http://works.bepress.com/cgi/viewcontent.cgi?article=1022&context=rbrookmeyer | archive-date = 7 December 2008 | df = dmy-all }} |
|||
* {{vcite journal|url=http://un.org/esa/population/publications/wpp2006/WPP2006_Highlights_rev.pdf|format=PDF|access-date=27 August 2008|year=2007|title=World population prospects: the 2006 revision, highlights|publisher=Population Division, Department of Economic and Social Affairs, United Nations|version=Working Paper No. ESA/P/WP.202|author1=<!-- Please add first missing authors to populate metadata. -->|deadurl=no|archive-url=https://web.archive.org/web/20080819191533/http://www.un.org/esa/population/publications/wpp2006/WPP2006_Highlights_rev.pdf|archive-date=19 August 2008}}</ref>。 |
|||
{{clear}} |
|||
==歷史== |
|||
[[File:Auguste D aus Marktbreit.jpg|thumb|left|1902年的{{tsl|en|Auguste D|奧古斯特·迪特|}},第一位阿茲海默症病例。]] |
|||
早在[[古典时代|古希臘羅馬時代]],當時的[[哲學家]]和[[医生|醫師]]就已經發現年老與[[失智症|失智]]的關聯性<ref name="pmid9661992"/>。1901年,德國[[精神病学|精神科醫師]][[愛羅斯·阿茲海默]]描述了第一個阿茲海默症病例。這名病患是一名名叫{{tsl|en|Auguste D|奧古斯特·迪特|}}的50歲女性,阿茲海默持續追蹤迪特的病程進展至病人於1906年死亡為止,並在之後發表該病例<ref>Auguste D.: |
|||
* {{vcite journal|author=Alzheimer Alois|title=Über eine eigenartige Erkrankung der Hirnrinde|trans_title=About a peculiar disease of the cerebral cortex|journal=Allgemeine Zeitschrift für Psychiatrie und Psychisch-Gerichtlich Medizin|volume=64|issue=1–2|pages=146–48|year=1907|language={{de icon}}}} |
|||
* {{vcite journal | vauthors = Alzheimer Alois | title = About a Peculiar Disease of the Cerebral Cortex | journal = Alzheimer Disease and Associated Disorders | volume = 1 | issue = 1 | pages = 3–8 | year = 1987 | pmid = 3331112 | author2 = L. Jarvik |translator= H. Greenson }} |
|||
* {{cite book |author1=Maurer Ulrike |author2=Maurer Konrad |title=Alzheimer: The Life of a Physician and the Career of a Disease|publisher=Columbia University Press|location=New York|year=2003|page=270|isbn=0-231-11896-1}}</ref>。其後五年,陸續又出現了11例類似的病例報告,其中有些論文已經用「阿茲海默症」來稱呼此疾病<ref name="pmid9661992" />。1910年7月15日,{{tsl|en|Emil Kraepelin|艾米爾·克雷珀林|}}於《精神科學課本》(''Textbook of Psychiatry'')第八版中首次將這些症狀描述為一個單一疾病,並將奧古斯特的部分症狀(如幻覺和妄想)及病理特徵(血管硬化)劃出該病的描述範圍<ref>{{vcite journal|author=Berrios G E|title=Alzheimer's Disease: A Conceptual History|journal=Int. J. Ger. Psychiatry|volume=5|issue=6|pages=355–65|year=1990|doi=10.1002/gps.930050603}}</ref>。艾米爾採用了「阿茲海默症」這個名字,並同時將其稱為「早發性老年失智症」(presenile dementia)將其視為是老年失智症的一個亞型<ref name="isbn1-4325-0833-4">{{cite book|title=Clinical Psychiatry: A Textbook For Students And Physicians (Reprint)|author=Kraepelin Emil|date=17 January 2007|publisher=Kessinger Publishing|isbn=1-4325-0833-4|page=568|translator=Diefendorf A. Ross}}</ref>。 |
|||
截至1970年代為止,阿茲海默症的診斷仍然僅限於描述45至65歲之間,提早出現特定失智症狀的患者。直到1977年,一場阿茲海默症研討會共識認定,阿茲海默症和老年失智症的臨床和病理表徵大致相同。雖然同時也強調兩者的病因學可能不同<ref name="isbn0-89004-225-X">{{cite book|title=Alzheimer's Disease: Senile Dementia and Related Disorders|publisher=Raven Press|year=1978|isbn=0-89004-225-X|editor=Katzman Robert|location=New York|page=595|editor2=Terry Robert D|editor3=Bick Katherine L}}</ref>,但這樣的共識已促使阿茲海默症的診斷,不再應該限定於特定年紀的的患者<ref>{{Cite journal|title=History of dementia and dementia in history: An overview|url=https://linkinghub.elsevier.com/retrieve/pii/S0022510X98001282|last=Boller|first=François|last2=Forbes|first2=Margaret M|date=1998-06|journal=Journal of the Neurological Sciences|issue=2|doi=10.1016/s0022-510x(98)00128-2|volume=158|pages=125–133|issn=0022-510X}}</ref>。此後一段時期,超過65歲且擁有阿茲海默症症狀的患者,另被描述為「阿茲海默型老年失智症」(senile dementia of the Alzheimer type,SDAT)。如今,阿茲海默症已經被接受為醫學的正式名詞,描述各年齡患者某種共同特定症狀的病徵<ref>{{Cite journal|title=Origin of the distinction between Alzheimer's disease and senile dementia: How history can clarify nosology|url=http://n.neurology.org/content/36/11/1497|last=Schoenberg|first=Bruce S.|last2=Rocca|first2=Walter A.|date=1986-11-01|journal=Neurology|issue=11|doi=10.1212/WNL.36.11.1497|volume=36|pages=1497–1497|issn=1526-632X|pmid=3531918|last3=Amaducci|first3=Luigi A.}}</ref>。 |
|||
==社會及文化== |
|||
===社會成本=== |
|||
失智症(特別是阿茲海默症)已成為歐美社會花費最多的疾病之一<ref name="pmid15685097"/><ref name="pmid9543467"/>,其他如[[阿根廷]]<ref name="pmid16870037">{{vcite journal|vauthors=Allegri RF, Butman J, Arizaga RL|title=Economic Impact of Dementia in Developing Countries: An Evaluation of Costs of Alzheimer-type Dementia in Argentina|journal=International Psychogeriatrics|volume=19|issue=4|pages=705–18|year=2007|pmid=16870037|doi=10.1017/S1041610206003784}}</ref>和[[大韩民国|南韓]]<ref name="pmid16858741">{{vcite journal|vauthors=Suh GH, Knapp M, Kang CJ|title=The Economic Costs of Dementia in Korea, 2002|journal=International Journal of Geriatric Psychiatry|volume=21|issue=8|pages=722–28|year=2006|pmid=16858741|doi=10.1002/gps.1552|month=August}}</ref>等國家的花費也節節攀升。這些花費可能會使社會結構老化,進而成為[[社会问题|社會問題]]。與阿茲海默症有關的社會成本包括直接的醫療費用(如護理之家照護、在宅日間照護)和間接的成本(如病人和照護者[[生产率|生產力]]降低)<ref name="pmid9543467"/>。雖然各個研究的數據有差異,但全球每年在失智症上花費約1600億美元<ref name="pmid16401889">{{vcite journal | vauthors = Wimo A, Jonsson L, Winblad B | title = An Estimate of the Worldwide Prevalence and Direct Costs of Dementia in 2003 | journal = Dementia and Geriatric Cognitive Disorders | volume = 21 | issue = 3 | pages = 175–81 | year = 2006 | pmid = 16401889 | doi = 10.1159/000090733 }}</ref>,單是美國每年就可能花費了約1000億美元<ref name="pmid9543467"/>。 |
|||
社會成本最大的來源為醫療專業人員的[[長期照護]],特別是{{tsl|en|institutionalisation|機構化|機構照護}}的費用可能佔了總花費的2/3<ref name="pmid15685097"/>。 患者在家的{{tsl|en|Cost-of-living index|生活費用指數|生活花費}}通常很高<ref name="pmid15685097"/>,尤其還需考慮患者家人的非正式成本,如照護時間和因照顧患者而減少的收入<ref name="pmid11445614">{{vcite journal | vauthors = Moore MJ, Zhu CW, Clipp EC | title = Informal Costs of Dementia Care: Estimates from the National Longitudinal Caregiver Study | journal = The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences | volume = 56 | issue = 4 | pages = S219–28 | year = 2001 | pmid = 11445614 | doi = 10.1093/geronb/56.4.S219 | month = July }}</ref>。 |
|||
隨著失智的嚴重度和行為問題增加,患者的花費將會上升<ref name="pmid16676288">{{vcite journal | vauthors = Jönsson L, Eriksdotter Jönhagen M, Kilander L | title = Determinants of Costs of Care for Patients with Alzheimer's Disease | journal = International Journal of Geriatric Psychiatry | volume = 21 | issue = 5 | pages = 449–59 | year = 2006 | pmid = 16676288 | doi = 10.1002/gps.1489 | month = May }}</ref>,需要醫療照護的時間也會增加<ref name="pmid11445614"/>。因此,任何能減緩認知功能下降、延遲機構照護或減少照護時間的治療都對經濟有幫助,目前的治療方法在經濟評估上已顯示正向的結果<ref name="pmid9543467"/>。 |
|||
===照護負擔=== |
|||
患者的主要照護者通常是其配偶或關係較密切的親屬<ref name="metlife.com">{{cite web|title=The MetLife study of Alzheimer's disease: The caregiving experience|date=August 2006|publisher=MetLife Mature Market Institute|format=PDF|access-date=5 February 2011|url=http://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf|archive-url=https://web.archive.org/web/20110108073750/http://www.metlife.com/assets/cao/mmi/publications/studies/mmi-alzheimers-disease-caregiving-experience-study.pdf|archive-date=8 January 2011|deadurl=yes}}</ref>。阿茲海默症會帶給照護者社會上、心理上、生理上,和經濟上極沉重的負擔<ref name="pmid17662119"/><ref name="pmid10489656">{{vcite journal | vauthors = Schneider J, Murray J, Banerjee S, Mann A | title = EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden | journal = International Journal of Geriatric Psychiatry | volume = 14 | issue = 8 | pages = 651–61 | year = 1999 | pmid = 10489656 | doi = 10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B | month = August }}</ref><ref name="pmid10489657">{{vcite journal | vauthors = Murray J, Schneider J, Banerjee S, Mann A | title = EUROCARE: A Cross-National Study of Co-resident Spouse Carers for People with Alzheimer's Disease: II—A Qualitative Analysis of the Experience of Caregiving | journal = International Journal of Geriatric Psychiatry | volume = 14 | issue = 8 | pages = 662–67 | year = 1999 | pmid = 10489657 | doi = 10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4 | month = August }}</ref>。居家照護可以延遲或減少病人接受更昂貴和更專業的照護<ref name="pmid18044111" /><ref>{{vcite journal | vauthors = Gaugler JE, Kane RL, Kane RA, Newcomer R | title = Early Community-based Service Utilization and Its Effects on Institutionalization in Dementia Caregiving | journal = The Gerontologist | volume = 45 | issue = 2 | pages = 177–85 | year = 2005 | pmid = 15799982 | doi = 10.1093/geront/45.2.177 | month = April }}</ref>,因此通常家屬和患者會傾向選擇居家照護<ref name="pmid18044111">{{vcite journal | vauthors = Zhu CW, Sano M | title = Economic Considerations in the Management of Alzheimer's Disease | journal = Clinical Interventions in Aging | volume = 1 | issue = 2 | pages = 143–54 | year = 2006 | pmid = 18044111 | pmc = 2695165 | doi = 10.2147/ciia.2006.1.2.143 }}</ref>。但即使如此,失智症患者仍然佔了護理之家住院人數的二分之三<ref name="pracGuideAPA"/>。 |
|||
失智症患者的照護者罹患生理和[[心理疾患]]的機會較高<ref name="pmid12480441">{{vcite journal | vauthors = Ritchie K, Lovestone S | title = The Dementias | journal = Lancet | volume = 360 | issue = 9347 | pages = 1759–66 | year = 2002 | pmid = 12480441 | doi = 10.1016/S0140-6736(02)11667-9 | month = November }}</ref>。 造成主要照護者有較大心理問題的因素包括患者住在家中、患者為其配偶、患者有令照護較為吃力的行為(如憂鬱、行為干擾、幻覺、睡眠問題、行走問題或[[社交孤立]])等<ref name="pmid2241719">{{vcite journal | vauthors = Brodaty H, Hadzi-Pavlovic D | title = Psychosocial Effects on Carers of Living with Persons with Dementia | journal = The Australian and New Zealand Journal of Psychiatry | volume = 24 | issue = 3 | pages = 351–61 | year = 1990 | pmid = 2241719 | doi = 10.3109/00048679009077702 | month = September }}</ref><ref name="pmid9646153">{{vcite journal | vauthors = Donaldson C, Tarrier N, Burns A | title = Determinants of Carer Stress in Alzheimer's Disease | journal = International Journal of Geriatric Psychiatry | volume = 13 | issue = 4 | pages = 248–56 | year = 1998 | pmid = 9646153 | doi = 10.1002/(SICI)1099-1166(199804)13:4<248::AID-GPS770>3.0.CO;2-0 | month = April }}</ref>。在經濟層面上,作為照護者的家人平均每週放棄47小時的工作時間來照護阿茲海默症患者,照護的代價相當高昂。在美國,每年直接和間接的照護支出從18,000到77,500美元不等,數值因研究而異<ref name="pmid11445614"/><ref name="metlife.com"/>。 |
|||
[[认知行为疗法]]和教導{{tsl|en|Coping (psychology)|應對策略}}(不論是個別指導或在團體中教導)都能有效提升照護者的心裡健康<ref name="pmid17662119"/><ref name="pmid11511058">{{vcite journal | vauthors = Pusey H, Richards D | title = A Systematic Review of the Effectiveness of Psychosocial Interventions for Carers of People with Dementia | journal = Aging & Mental Health | volume = 5 | issue = 2 | pages = 107–19 | year = 2001 | pmid = 11511058 | doi = 10.1080/13607860120038302 | month = May }}</ref>。 |
|||
===媒體=== |
|||
許多電影或影集描述過阿茲海默症,例如《{{tsl|en|Iris (2001 film)|長路將盡}}》(2001,取材自{{tsl|en|John Bayley (writer)|約翰·貝禮}}描述其妻的回憶錄)<ref>{{cite book|title=Iris: A Memoir of Iris Murdoch|author=Bayley John|publisher=Abacus|location=London|year=2000|isbn=978-0-349-11215-2|oclc=41960006}}</ref>、《[[忘了、忘不了]]》(2004,取材自[[尼可拉斯·史派克]]1996年的{{tsl|en|The Notebook (novel)|手札情緣 (小說)|同名小說}})<ref>{{cite book|title=The notebook|author=Sparks Nicholas|year=1996|publisher=Thorndike Press|location=Thorndike, Maine|page=268|isbn=0-7862-0821-X}}</ref>、《[[我腦海中的橡皮擦]]》(2004)、《{{tsl|en|Thanmathra|Thanmathra}}》(2005)<ref>{{cite web|url=http://www.webindia123.com/movie/regional/thanmatra/index.htm|title=Thanmathra|publisher=Webindia123.com|access-date=24 January 2008|deadurl=no|archive-url=https://web.archive.org/web/20071106105455/http://www.webindia123.com/movie/regional/thanmatra/index.htm|archive-date=6 November 2007}}</ref>、《[[明日的記憶]]》 (2006,取材自荻原浩的同名小說)<ref>{{cite book|author=Ogiwara Hiroshi|year=2004|title=Ashita no Kioku|location=Tōkyō|publisher=Kōbunsha|isbn=978-4-334-92446-1|oclc=57352130|language=ja}}</ref>、《[[妳的樣子]]》(2006,取材自[[艾丽斯·芒罗]]的[[短篇小说]]《[[恨,友谊,追求,爱情,婚姻]]》)<ref>{{cite book|title=[[恨,友谊,追求,爱情,婚姻|Hateship, Friendship, Courtship, Loveship, Marriage: Stories]]|author=Munro Alice|location=New York|publisher=A.A. Knopf|year=2001|isbn=978-0-375-41300-1|oclc=46929223}}</ref>、《[[我想念我自己]]》(2014,內容描述一位罹患早發型阿茲海默症的[[哥伦比亚大学]]教授,取材自{{tsl|en|Lisa Genova|莉莎·潔諾娃}}的{{tsl|en|我想念我自己 (小說)||同名小說}},並以[[茱莉安·摩爾]]為英語的片名角色)。與阿茲海默症相關的紀錄片有《馬爾柯姆與芭芭拉:愛的故事》(1999,Malcolm and Barbara: A Love Story)和《馬爾柯姆與芭芭拉:愛的告別》(2007,Malcolm and Barbara: Love's Farewell),兩者都以鋼琴家{{tsl|en|Malcolm Pointon|馬爾柯姆·波因頓}}為主角<ref>{{cite web|url=http://www.dfgdocs.com/Directory/Titles/700.aspx |title=Malcolm and Barbara: A love story |publisher=Dfgdocs |access-date=24 January 2008 |deadurl=yes |archive-url=https://web.archive.org/web/20080524213821/http://www.dfgdocs.com/Directory/Titles/700.aspx |archive-date=24 May 2008 |df= }}</ref><ref> |
|||
{{cite web|url=http://www.bbc.co.uk/cambridgeshire/content/articles/2007/08/06/pointon_audio_feature.shtml|title=Malcolm and Barbara: A love story|publisher=BBC Cambridgeshire|access-date=2 March 2008|deadurl=no|archive-url=https://web.archive.org/web/20121110084233/http://www.bbc.co.uk/cambridgeshire/content/articles/2007/08/06/pointon_audio_feature.shtml|archive-date=10 November 2012}}</ref><ref>{{cite news|url=https://www.theguardian.com/media/2007/aug/07/broadcasting.itv|title=Alzheimer's film-maker to face ITV lawyers|publisher=Guardian Media|date=7 August 2007|access-date=24 January 2008|location=London|author=Plunkett J| archive-url= https://web.archive.org/web/20080115132419/http://www.guardian.co.uk/media/2007/aug/07/broadcasting.itv| archive-date= 15 January 2008 |deadurl=no}}</ref>。 |
|||
== 註釋 == |
|||
<references group="註" /> |
|||
== 參考文獻 == |
|||
{{Reflist|2}} |
|||
== 延伸閱讀 == |
|||
{{Library resources box |by=no |onlinebooks=no |others=yes |about=yes |label=阿茲海默症|lcheading=Alzheimers Disease}} |
|||
{{refbegin}} |
{{refbegin}} |
||
* {{cite book|title=Alzheimer's Disease: Unraveling the Mystery|url=http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-unraveling-mystery|publisher=US Department of Health and Human Services, National Institute on Aging, NIH|year=2008|deadurl=yes| |
* {{cite book|title=Alzheimer's Disease: Unraveling the Mystery|url=http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-unraveling-mystery|publisher=US Department of Health and Human Services, National Institute on Aging, NIH|year=2008|deadurl=yes|archive-url=https://web.archive.org/web/20120108204115/http://www.nia.nih.gov/alzheimers/publication/alzheimers-disease-unraveling-mystery|archive-date=8 January 2012}} |
||
* {{cite book|title=Can Alzheimer's Disease Be Prevented?|url=http://www.globalaging.org/health/us/2009/prevented.pdf|publisher=US Department of Health and Human Services, National Institute on Aging, NIH|year=2009|deadurl=yes|archive-url=https://web.archive.org/web/20130502233551/http://www.globalaging.org/health/us/2009/prevented.pdf|archive-date=2 May 2013}} |
|||
* {{cite book|author=Wolfgang Maier, Jörg B. Schulz, Sascha Weggen |title=Alzheimer & Demenzen Verstehen: Diagnose, Behandlung, Alltag, Betreuung|publisher=Trias |location=Stuttgart |year=2011 |id= ISBN 978-3-8304-6441-9}} |
|||
* {{cite book|title= |
* {{cite book|title=Caring for a Person with Alzheimer's Disease: Your Easy-to-Use Guide from the National Institute on Aging|url=http://www.nia.nih.gov/alzheimers/publication/caring-person-alzheimers-disease|publisher=US Department of Health and Human Services, National Institute on Aging, NIH|year=2009|deadurl=yes|archive-url=https://web.archive.org/web/20120108193219/http://www.nia.nih.gov/alzheimers/publication/caring-person-alzheimers-disease|archive-date=8 January 2012}} |
||
* {{cite |
* {{cite web|title=Alzheimer's Behavior Management: Learn to Manage Common Behavior Problems |url=http://www.helpguide.org/elder/alzheimers_behavior_problems.htm |vauthors=Russell D, Barston S, White M |publisher=helpguide.org |date=19 December 2007 |access-date=29 February 2008 |archive-url=https://web.archive.org/web/20080223082753/http://www.helpguide.org/elder/alzheimers_behavior_problems.htm |archive-date=23 February 2008 |deadurl=yes }} |
||
* {{vcite journal| |
* {{vcite journal | vauthors = Irvine K |author2={{tsl|en|Keith Laws||Laws KR}} |author3=Gale TM |author4=Kondel TK | title = Greater cognitive deterioration in women than men with Alzheimer's disease: a meta analysis | journal = Journal of Clinical and Experimental Neuropsychology | volume = 34 | issue = 9 | pages = 989–98 | year = 2012 | pmid = 22913619 | doi = 10.1080/13803395.2012.712676 | type = Meta-analysis }} |
||
* {{vcite journal|author=Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B|title=Guidelines for Managing Alzheimer's Disease: Part II. Treatment|journal=American Family Physician|volume=65|issue=12|pages=2525–2534|year=2002|pmid=12086242|url=http://www.aafp.org/afp/20020615/2525.html}} |
|||
* {{cite web|title=Alzheimer's Behavior Management: Learn to Manage Common Behavior Problems|url=http://www.helpguide.org/elder/alzheimers_behavior_problems.htm|author=Russell D, Barston S, White M|publisher=helpguide.org|date=2007-12-19|accessdate=2008-02-29|archiveurl=https://web.archive.org/web/20080223082753/http://www.helpguide.org/elder/alzheimers_behavior_problems.htm|archivedate=23 二月 2008|deadurl=yes}} |
|||
{{refend}} |
{{refend}} |
||
==外部連結== |
== 外部連結 == |
||
{{Commons category|Alzheimer's disease}} |
{{Commons category|Alzheimer's disease}} |
||
{{Medical condition classification and resources |
|||
*{{dmoz|Health/Conditions_and_Diseases/Neurological_Disorders/Alzheimer%27s/}} |
|||
|DiseasesDB=490 |
|||
*[http://infographic.chinatimes.com/20160924000006-262802 帕金森氏症 阿茲海默症大不同] |
|||
|ICD10={{ICD10|G|30||g|30}}, {{ICD10|F|00||f|00}} |
|||
*[http://www.gaain.org/ The Global Alzheimer's Association Interactive Network] |
|||
|ICD9={{ICD9|331.0}}, {{ICD9|290.1}} |
|||
*[http://www.alz.org/ Alzheimer's Association] |
|||
|ICDO= |
|||
*[http://www.tada2002.org.tw/ 台灣失智症協會] |
|||
|OMIM=104300 |
|||
|MedlinePlus=000760 |
|||
{{ICD-10-F}} |
|||
|eMedicineSubj=neuro |
|||
|eMedicineTopic=13 |
|||
|MeshID=D000544 |
|||
|GeneReviewsNBK=NBK1161 |
|||
|Scholia = Q11081 |
|||
|}} |
|||
* {{dmoz|Health/Conditions_and_Diseases/Neurological_Disorders/Alzheimer%27s/}} |
|||
{{Mental and behavioural disorders|selected=neurological}} |
|||
{{CNS diseases of the nervous system}} |
|||
{{Amyloidosis}} |
{{Amyloidosis}} |
||
{{Authority control}} |
{{Authority control}} |
||
[[Category:阿尔茨海默病| ]] |
[[Category:阿尔茨海默病| ]] |
||
[[Category: |
[[Category:病因不明的疾病]] |
||
[[Category: |
[[Category:神经科学中的未解之谜]] |
||
[[Category:學習障礙]] |
|||
[[Category:精神病学诊断]] |
|||
[[Category:痴呆]] |
|||
[[Category:異常心理學]] |
|||
[[Category:认知障碍]] |
|||
[[Category:失語症]] |
|||
2019年1月1日 (二) 15:37的版本
| 阿茲海默症 | |
|---|---|
| 同义词 | 老年痴呆症 |
 | |
| 比較正常(左)和阿茲海默症(右)患者的腦部。 | |
| 症状 | 短期記憶喪失、語言障礙、定向障礙、情緒不穩[1][2] |
| 常見始發於 | 大於65歲[3] |
| 病程 | 慢性[2] |
| 类型 | Tau蛋白質異常沉積[*]、衰老相關疾病[*]、疾病 |
| 肇因 | 瞭解有限[1] |
| 风险因子 | 遺傳、頭部外傷、憂鬱症、高血壓[1][4] |
| 診斷方法 | 排除其他可能原因後基於症狀和認知測試診斷[5] |
| 相似疾病或共病 | 正常老化[1] |
| 藥物 | 乙醯膽鹼抑制劑、NMDA受體拮抗劑(稍有幫助)[6] |
| 预后 | 餘命3至9年[7] |
| 盛行率 | 2.98億人(2015) |
| 死亡數 | 190萬人(2015) |
| 分类和外部资源 | |
| 醫學專科 | 神經內科 |
| ICD-11 | 8A20 |
| ICD-9-CM | 331.0、290.1 |
| OMIM | 104300 |
| DiseasesDB | 490 |
| MedlinePlus | 000760 |
| eMedicine | 1134817 |
阿茲海默症(英語:Alzheimer's disease,縮寫:AD),俗稱早老性痴呆、老人痴呆(但醫界不建議使用此名稱[註 1]),是一種發病進程緩慢、隨著時間不斷惡化的神經退化性疾病[1][2],此病症佔了失智症中六到七成的成因[1][2]。最常見的早期症狀為喪失短期記憶(難以記住最近發生的事)[1],當疾病除見進展,症狀可能逐漸出現,包括語言障礙、定向障礙(包括容易迷路)、情緒不穩、喪失動機、無法自理和許多行為問題[1][2]。當情況惡化時,患者往往會因此和家庭或社會脫節[1],並逐漸喪失身體機能,最終導致死亡[8]。雖然疾程因人而異,但診斷後的平均餘命約為三到九年[7][9]。
阿茲海默症的真正成因至今仍然不明[1]。目前將阿茲海默症視為一種神經退化的疾病,並認為有將近七成的風險因子與遺傳有關[4];其他的風險因子還有頭部外傷、憂鬱症和高血壓[1]。疾病的進程與大腦中的纖維狀類澱粉蛋白質斑塊沉積和Tau蛋白有關[4]。要診斷阿茲海默症,需根據病人病史、行為評估、認知測驗、腦部影像檢查和血液採檢來排除其他可能的因素[5]。疾病初期的症狀常被誤認為是正常老化[1]。確診則需藉助腦部組織檢驗[4]。身心和身體運動、避免肥胖都有助於減少罹患阿茲海默症的風險[4][10]。目前沒有實證證明特定藥物或營養補充品對疾病治療有效[11]。
目前並沒有可以阻止或逆轉病程的治療,只有少數方法或許可以暫時緩解或改善症狀[2]。疾病會使患者會越來越需要他人的照護,這對照護者是一大負擔;這樣的照護壓力涵括了社會、生理、精神和經濟等各個層面[12]。運動計畫能改善病人的日常生活功能,並可能可以改善預後[13]。由失智症狀引起的行為異常和思覺失調常以抗精神病藥治療,惟其效益不高且可能增加死亡率,因此通常不建議使用[14][15]。
2015年,全球大約有2980萬人罹患阿茲海默症[2][16]。患者的發病年齡一般在65歲以上,但大約有4%到5%的患者會在65歲之前就發病,屬於早發性阿茲海默症[3]。65歲以上的盛行率約為6%[1]。2015年,失智症造成約190萬人死亡[17]。1906年,德國精神學家與病理學家愛羅斯·阿茲海默首先描述並隨後命名了阿茲海默症[18] 。在已開發國家中,阿茲海默症是耗費最多社會資源的一種疾病[19][20]。
症狀和徵候
阿茲海默症的病程根據認知能力和身體機能的惡化程度分成四個時期,以下分段說明。
失智症前期
阿茲海默症最初的症狀常被誤認為是老化或是壓力[22],但若進行詳細的神經心理學檢查,甚至能在確診為阿茲海默症八年前就可發現輕微的認知困難[23]。這些早期症狀可以影響大部分複雜的日常生活活動[24],最明顯的缺陷是短期記憶障礙,主要是難以記住最近發生的事和無法吸收新資訊[23][25]。
其他症狀包括注意力管控、計畫事情、彈性處理、抽象思考和語義記憶等方面的問題[23]。冷漠也是此時期會出現的症狀之一,並會是在病程中持續出現的精神症狀[26]。阿茲海默症的臨床前期也被稱作輕微認知障礙(MCI)[27],這是一個介於正常和失憶症之間的過渡狀態,但MCI可以是許多症候群的表現,而當它以記憶喪失為主要表現時,則稱作失憶性輕微認知障礙(amnestic MCI),此一名詞常被用來稱呼阿茲海默症的臨床前期[28]。
早期
阿茲海默症病患的學習與記憶障礙會愈見明顯,最後使醫師能確認診斷。在少部分病患中,語言障礙、執行障礙、認識障礙(失認症,agnosia)或技能執行障礙(失用症,apraxia)會比記憶障礙更明顯[29]。阿茲海默症並不會對所有記憶能力都有同等的影響,相對於新近發生的事情或記憶,病患長期的情节记忆、语义记忆和内隐记忆(身體記住如何做一件事,例如使用叉子吃東西)受到的影響比較少[30][31]。
阿茲海默症患者的語言障礙主要為原發性進行性失語症,特徵是病患可使用的詞彙變少,且流暢度降低,導致病患的口語和書面表達變得困難[29][32]。在這一時期,病患通常還能適當表達簡單的想法[29][32][33];當進行精細動作時(如寫作、畫圖、或是穿衣),可能會出現些微的動作不協調和計畫困難(失用症),但這些徵兆常會被忽略[29]。隨著疾病進展,阿茲海默症病患通常仍能獨立完成許多事情,但是大部分需要認知功能的活動可能就需要協助或是監督[29]。
中期
隨著病情惡化,病患將失去獨立生活的能力,而無法進行大部分的日常活動[29]。患者的語言障礙逐漸變得明顯,常會無法想起詞彙(命名不能症),會使用錯誤的字彙來替換(言語錯亂症),同時也漸漸失去讀寫能力[29][33]。患者在執行複雜的動作序列時會變得不協調,增加了跌倒的風險[29]。在這一時期,記憶問題也會惡化,病患可能無法認出親近的家屬[29],之前仍完整的长期记忆也受到影響[29]。
此時期行為和神經精神病學的變化也更為顯著,常見的表現包括遊蕩、易怒和情緒不穩,這些變化會導致病患突然哭泣、突發的非故意攻擊行為、或是拒絕接受照顧[29],此時也會出現日落症候群[34]。大約30%的患者會產生出現妄想錯認或其他妄想症狀[29],另外也可能會尿失禁[29]。患者無法體認到疾病的進展(病覺缺失症,即缺乏病識感)[29]。這些症狀都會對家屬或照護者帶來壓力,由居家照護轉至長期照護機構可減輕此類壓力[29][35]。
晚期
在阿茲海默症的最終時期,病患已經完全依賴照護者[29],語言能力退化至簡單的詞語甚至僅有單字,最後完全失去談話能力[29][33]。除了失去口語能力之外,病患通常能理解並回應情感刺激[29],雖然攻擊行為仍然存在,但大多時間表現得極度冷漠和疲倦[29],病患最終無法獨立進行任何簡單的事情[29],肌肉質量和行動能力退化至長期臥床,也無法自行進食[29]。阿茲海默症是一種絕症,但死因通常是外在因素,例如褥疮感染或肺炎,而不是疾病本身[29]。
病因
大部分病患罹患阿茲海默症的原因仍然不明(除了1%到5%的病患可以找到基因差異)[36][37]。目前有幾個不同的假说嘗試解釋阿茲海默症的病因。
遺傳
根據雙胞胎和家族研究,阿茲海默症的基因遺傳性約在49%到79%之間[38][39]。約0.1%家族性遺傳的患者為體染色體顯性遺傳,他們常在65歲前發病,稱為早發性家族性阿茲海默症[40]。家族型阿茲海默症病患大多可以歸因於以下三個基因其中之一發生突變:前類澱粉蛋白質基因APP 、Presenilin 1和Presenilin 2[41], 這三個基因的突變大多會導致類澱粉蛋白質斑塊的主要成分Aβ42在細胞中的產量升高[42],一些突變雖然不增加Aβ42的產量,但會改變細胞內Aβ42和其他主要同型異構物(特別是Aβ40)的比例[43][44]。
阿茲海默症患者多數沒有上述的體染色體遺傳,稱為偶發型阿茲海默症。但有些基因或環境因素仍可能是罹患此病的危險因子。最著名的基因危險因子是载脂蛋白E(APOE)的ε4等位基因[45][46],約有40%到80%的病患帶有至少一個APOEε4等位基因[46],其中異型合子的個體罹患風險增加3倍,而同型合子則增加15倍[40]。然而,環境或基因造成的影響並不一定會完全表現出來。舉例來說,不同於其他族群,部分奈及利亞族群罹患阿茲海默症的機率和發病年齡與其是否帶有APOEε4沒有相關[47][48] 。遺傳學家已經檢驗超過400個候選基因與遲發性偶發性阿茲海默症(LOAD)的關聯,但大部分的基因都沒有發現明顯相關性[40][41]。近期使用全基因組關聯分析(GWAS)的研究則找到了19個可能會影響罹病風險的基因區塊[49],這些基因為CASS4、CELF1、FERMT2、HLA-DRB5、INPP5D、MEF2C、NME8、PTK2B、SORL1、ZCWPW1、SlC24A4、CLU、PICALM、CR1、BIN1、MS4A、ABCA7、EPHA1和CD2AP[49]。研究也發現TREM2的某些等位基因變異會增加罹患阿茲海默症的風險達3到5倍,可能的原因是某些TREM2變異會使腦中的白血球將無法控制大腦中Aβ的產生量[50][51]。2018年的一項研究利用記憶、語言、視覺立體、執行,和功能等五個項目,配合新發表的30個與阿茲海默症相關的單核苷酸多態性(SNPs),將阿茲海默症6大類[52]。
膽鹼性假說
膽鹼性假說是最早被提出來的假說,也是現今大部分阿茲海默症藥物所依據的理論基礎[53],該假說認為阿茲海默症是由於神經系統減少產生神經傳導物質乙酰胆碱而造成的,雖然膽鹼性假說的歷史悠久,但是沒有受到廣泛的支持,主要是由於使用藥物治療乙醯膽鹼缺乏後,對於阿茲海默症的療效有限[54]。
類澱粉胜肽假說
1991年,學者提出類澱粉胜肽假說,認為β類澱粉胜肽(Aβ)在大腦堆積可能是導致阿茲海默症的根本原因[55][56]。有關唐氏症患者的研究支持了這項假說,表現Aβ的前類澱粉蛋白基因(APP)位在21號染色體上,而唐氏症病患多了一個21號染色體的副本,同時唐氏症病患幾乎全都在40歲左右時罹患阿茲海默症[57][58]。此外,E型載脂蛋白4(APOE4)是上阿茲海默症的主要遺傳危險因子,雖然載脂蛋白會增強Aβ的降解,但特定的載脂蛋白異構體對此反應的效果較差(如APOE4),導致多餘的Aβ在大腦中累積[59]。進一步的證據則是來自於基因轉殖鼠實驗,研究人員在實驗鼠身上表現突變型人類APP基因,結果發現其大腦會產生纖維狀類澱粉蛋白斑塊(fibrillar amyloid plaques),並出現類似阿茲海默症的大腦病理變化及空間學習障礙[60]。
曾有一種實驗性疫苗在早期人體試驗中可以清除類澱粉蛋白斑塊,但此種治療對失智症卻沒有顯著的效果[61]。因此研究者轉而懷疑沒有形成大型類澱粉蛋白斑塊的Aβ寡聚體才是主要的致病型態,這些寡聚體也被稱為類澱粉蛋白質衍生可溶性配體(amyloid-derived diffusible ligands, ADDLs),它們會結合到神經細胞表面的受體並改變突觸的結構,因此會破壞神經元溝通[62]。其中一種可能的Aβ寡聚體受體可能是普利昂蛋白,這種蛋白的錯誤構型會引起狂牛症和人類庫賈氏症,因此暗示著阿茲海默症與其他神經退化性疾病的機轉可能互有關聯[63]。
2009年,類澱粉胜肽假說有了新的發展,新的研究指出和Aβ關係密切的蛋白質可能才是阿茲海默症的罪魁禍首。此類與類澱粉斑塊相關的機制會在早年快速發育的時期,使腦部神經元間的連結減少,並在年紀較大後受到老化相關過程的刺激,導致阿茲海默症中的神經元退化[64]。該研究發現APP是DR6的一個配體,β-secretase會切下的APP的N端片段產生N-APP(同樣的酵素也參與APP修飾為Aβ的過程),N-APP則會與死亡受體6(death receptor 6,DR6,或稱TNFRSF21)結合,啟動細胞凋亡途徑。DR6在阿茲海默症患者受影響的腦區中有高量的表現,因此在老化的大腦中,可能就是N-APP/DR6途徑被活化而造成了神經元損傷[64]。N-APP/DR6途徑所啟動的細胞凋亡包含了神經細胞本體和軸突,不同於一般細胞凋亡的機制需要活化caspase-3,軸突的退化需要活化caspase-6。此外,經由caspase-6路徑所啟動的細胞凋亡,也可能和另一種杭廷頓舞蹈症相關[65]。2017年,β-secretase抑制劑verubecestat的臨床試驗因為被認為對臨床沒有助益而遭到中止[66]。
Tau蛋白假說

Tau蛋白假說認為Tau蛋白異常是引起阿茲海默症病情發展的主因[56]。在這個模型中,過度磷酸化的Tau蛋白會開始與其他Tau蛋白質配對結合,結果在神經細胞中形成了神經纖維糾結[67]。在這種情形下,神經細胞內的微管開始瓦解並導致由細胞骨架構成的運送系統崩壞[68],這將造成神經細胞之間的化學訊息溝通失效,接著導致神經細胞死亡[69]。
其他假說
新生血管假說認為血腦屏障功能減低也可能和阿茲海默症有關[70]。
阿茲海默症患者細胞內外金屬離子(如銅、鐵、鋅離子)會不平衡,雖然目前不清楚是蛋白質的改變造成離子不平衡,抑或離子的改變造成蛋白質的變化,這些離子會影響tau蛋白、APP和APOE[71],這些蛋白失調會造成細胞內部的氧化壓力,並因此造成相關的病變[72][73][74][75][76]。然而有些相關研究的品質受到批評[77][78],因此這種推論仍有爭議[79]。多數的研究者並不支持鋁離子和阿茲海默症有因果關係[78]。
抽菸是阿茲海默症的顯著危險因子[80], 先天免疫系統的發炎指標則是遲發型阿茲海默症的危險因子[81]。有限的證據指出空氣污染可能也是促進阿茲海默症發展的一項因素[82]。
牙周炎發生時的螺旋體感染也可能造成失智,並參與阿茲海默症的病理機制 [83]。真菌感染也是一個可能的疾病機轉[84]。
也有假說認為 寡突膠細胞功能異常以及其在老化過程中產生的髓鞘問題會造成軸突的傷害,最後導致了類澱粉生成和tau蛋白過磷酸化的副作用[85][86]。
逆生假說(Retrogenesis)是貝里·萊斯伯格(Barry Reisberg)在1980年代提出的另一項阿茲海默症假說[87]。胎兒發育時會歷經一連串的神經發生,這個過程始於神經板形成,終於髓鞘形成,該假說認為阿茲海默症患者的神經退化就如同此一過程的逆轉,先是神經脫鞘、白質的軸突死亡、最後灰質的神經元死亡[88]。同樣地,嬰兒會經歷認知發展,該假說也認為阿茲海默症患者的認知障礙就如同此一過程的倒轉[87]。萊斯伯格也發展出了一套稱為FAST(功能性評估分級工具,Functional Assessment Staging Tool)的照護評估工具,用以評估阿茲海默患者的病程發展到哪個階段,以此為依據為每個階段的患者提供適當的照護建議[87][89]。
病生理學
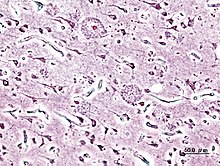

神經病理學
阿茲海默症的特徵是大腦皮質及特定皮質下區域的神經元和突触喪失。神經元喪失過多的區域甚至會導致巨觀解剖上的萎縮,常見主要遭到的進犯部位包含颞叶、顶叶、一部份的額葉,和扣帶回[90]。某些腦幹的核區可能也會受到影響,如蓝斑核等[91]。磁振造影(MRI)和正子電腦斷層掃瞄(PET)研究已報導患者在疾病進程中部分腦區萎縮的狀況,且跟其他健康老年人比較也能發現有部分腦區萎縮[92][93]。
在顯微鏡下,阿茲海默症患者的腦皮質可以看到明顯的類澱粉斑塊以及神經元纖維纏結[94]。斑塊大多由緻密且不溶於水的β類澱粉樣胜肽及細胞衍生物所構成,通常堆積於神經元周圍。神經纖維纏結則通常是由微管相關蛋白質Tau所構成,患者的Tau蛋白會過度磷酸化並聚集於細胞內。雖然許多老年人的大腦中都可發現這些因老化形成的斑塊和纏結,但阿茲海默症患者會在特定腦區出現更多斑塊及纏結,例如顳葉等[95]。路易氏體在病患腦中也很常見[96]。
生物化學
阿茲海默症也被視為一種蛋白質折疊錯誤的疾病(蛋白质构象病),是由於大腦中折疊異常的β類澱粉蛋白和Tau蛋白質堆積而造成[97]。構成斑塊的β類澱粉蛋白質(Aβ)是由約39至43個氨基酸構成的短鏈胜肽。Aβ為前類澱粉蛋白(APP)的一小片段,該蛋白為神經元細胞膜上的一種跨膜蛋白,對神經元的生長、存活和受傷後的修復非常重要[98][99]。阿茲海默症患者的γ分泌酶及β分泌酶會共同進行蛋白酶解作用,將APP切成小片段[100]。其中某些片段即為β類澱粉蛋白,他們會在神經元的胞外間質堆積,形成老年斑塊[94][101]。
還有一種理論認為阿茲海默症是Tau蛋白質異常沉積造成。每個神經元都有由微管組成的細胞內支撐系統,稱為細胞骨架,這些微管的作用如同軌道,引導營養物質和其他分子在細胞本體和軸突之間來回移動。Tau蛋白質被磷酸化之後可以穩定微管,所以被歸類為微管關聯蛋白質[102]。在阿茲海默症病患中,Tau蛋白質發生突變而過度磷酸化,進而造成微管瓦解。釋出的Tau蛋白質會聚集起來,產生神經纖維團塊並且瓦解神經元的運輸系統[103]。</ref> Pathogenic tau can also cause neuronal death through transposable element dysregulation.[104]
疾病機轉
目前仍不清楚Aβ蛋白的異常合成與異常聚集,如何導致阿茲海默症的病理變化[105][106]。類澱粉蛋白假說指出Aβ蛋白的堆積是造成神經元退化的主要原因,聚集的類澱粉蛋白纖維會瓦解細胞的鈣離子平衡,並造成細胞凋亡[107]。Aβ蛋白也會選擇性地堆積於病灶處細胞的线粒体中,抑制部分酵素的功能以及神經元使用葡萄糖的能力[108]。
多種發炎反應和細胞激素也可能在阿茲海默症的病理變化相關[109]。越來越多證據顯示腦部神經元與免疫系統之間有很強的交互作用。肥胖與全身性發炎反應等干擾免疫反應的因子,可能都會引起疾病惡化[110]。
不同神經滋養因子(如脑源性神经营养因子)的分布變化,以及其受體的表現狀況,都曾有研究指出與阿茲海默症有關[111][112]。
診斷

阿茲海默症的診斷一般透過病史收集和行為觀察獲得。臨床醫師可透過觀察患者神經學及神經心理學上的特徵,並排除其他診斷來佐證診斷[113][114]。電腦斷層掃瞄(CT)、核磁共振成像(MRI)、單光子電腦斷層攝影(SPECR),和正子電腦斷層攝影(PET)等高階醫學影像技術,可以協助排除其他大腦病變或失智症亞型[115]。此外,醫學影像也可以用於預測從輕微認知失調到阿茲海默症的轉變[116]。
神經心理學評估(包括記憶測試)可以進一步鑑別疾病狀態[22],醫學組織已經為臨床醫師建立診斷標準以簡化及標準化診斷程序。阿茲海默症最準確的診斷方法為屍體病理解剖,直接取得腦組織,經由組織學免疫染色法進行確認診斷[117]。
診斷標準
美國神經與溝通疾患及中風研究院(NINCDS)及阿茲海默症及相關疾病協會(ADRDA)於1984年制定了NINCDS-ADRDA阿茲海默症診斷標準,為目前最常用的診斷標準之一[117],最新一版於2007年更新[118]。臨床診斷標準包含認知功能損害、疑似失智症狀,並經由神經心理學評估確認。
腦組織的顯微鏡檢可以提供阿茲海默症的組織病理學確認診斷。上述的診斷標準在藉由組織病理學進行評估後,顯示該標準的信度及效度都不錯[119]。阿茲海默症最常損害的八個智能區塊為記憶、語言、知觉、注意力、动作技能、定向力、問題解決能力、執行能力等。這些問題在NINCDS-ADRDA診斷標準及美國精神醫學學會發行的《精神疾病診斷與統計手冊》(DSM-IV-TR)皆有提到[120][121]。
檢測技術

簡短智能測驗(MMSE)等神經心理學檢查常被用於評估認知功能障礙,以利於後續診斷。若要取得更可信的結果,可以進行更全面的測試,特別是在疾病初期的患者[122][123]。除非有明顯的認知功能障礙,神經學檢察結果在疾病初期一般會呈現正常,可能無法與其他疾病做出鑑別,包含其他原因造成的失智症。
進一步的神經學檢查對於阿茲海默症的鑑別診斷相當重要[22],與家人會談也有助於評估病情。主要照護人能夠提供患者日常活動功能的重要資訊,以及病人
心智功能下降的情形[124]。由於患者通常自己無法查覺自身的異狀,因此旁觀者的觀點對於疾病的評估相當重要[125]。但在失智症初期時,家人通常也無法察覺病人的症狀,而無法提供醫師準確的資訊[126]。
輔助性檢查可以提供一些額外資訊,以利排除其他診斷。血液检查也可以協助排除阿茲海默症以外的診斷[22],偶見有些病因是可以治癒的[127]。常見的血檢項目包含甲狀腺功能測試、维生素B12、梅毒檢測、代謝性疾病檢查(如腎功能檢查、電解質水平,以及糖尿病檢查)、重金屬水平,以及貧血等等。另外也必須譫妄的可能性。
針對抑鬱症的心理測驗也建議進行,因為阿茲海默症常同時伴隨抑鬱症狀,也是認知功能損傷的早期症狀之一[128],甚至是原因[129][130]。
C-PIB正子照影(C-PIB PET)在疾病初期的準確率不高,因此不建議用於早期診斷,或預測輕度知能障礙患者進展到阿茲海默症的機會[131]。¹⁸F-FDG正子照影(¹⁸F-FDG PET)在預測阿茲海默症的發生機會上也沒有實證支持[132]。
預防
目前實證上沒有任何能有效預防阿茲海默症的方式[11],有關預防及推遲阿茲海默症進程的跨國研究結果經常不一致。流行病學研究推測阿茲海默症可能與某些飲食、心血管風險、藥物等因子相關。某些智力活動及族群發生阿茲海默症的機會可能也不同。但這些相關性是否真的可以用來預防阿茲海默症,仍需進一步的研究闡明[11]。
藥物
雖然高膽固醇、高血壓、糖尿病,及吸菸等心血管風險增強因子,可能與較高的阿茲海默症發生率相關[133][134]。但服用降膽固醇用的他汀類藥物(Statins)無法有效預防阿茲海默症的發生或推遲其進程[135][136]。
長期使用非甾体抗炎药(NSAIDs)在2007年時被認為可能與較低的阿茲海默症發生率相關[137]。亦有證據顯示NSAID可以減少與類澱粉斑塊相關的發炎反應。但由於副作用過高,相關的臨床實驗提早中止[11]。截至目前為止,尚無預防研究完成試驗[11]。NSAID對於治療阿茲海默症沒有任何功效,但為預防的候選藥物之一[138]。更年期的激素替代療法可能會增加失智的風險,即使已經停藥也一樣[139]。
生活型態
從事某些益智活動的人們,罹患阿茲海默症的風險似乎較低,如閱讀、圖版遊戲、填字游戏、演奏樂器,及從事日常社交活動等[140]。這點符合認知存量假說,該假說認為有些生活經歷會增進神經功能的效能,並擴充個人的認知存量,進而延遲失智症的發生[140]。接受教育也會延遲阿茲海默症的發生,但並不會改變病程的長短[141]。學習第二語言也有可能可以延遲疾病發生[142]。體能鍛鍊亦顯示可以降低阿茲海默症的風險[141],且發生失智症的比率較低[143],另外也能減輕患者症狀嚴重程度[144]。
飲食
平時身體健康者、日本人、地中海飲食者顯示罹患阿茲海默症的機會較小[145]。地中海飲食同時也能改善患病者的預後[146]。飲食含有高脂肪酸及簡單碳水化合物(simple carbohydrates,單醣或雙醣等)患病機率也較高[147]。地中海飲食對心血管正面影響的機制也已有文獻發表[148]。
飲食的配方與阿茲海默症間的關係目前仍不明朗,因為相關的研究結果沒有定論[145]。有限證據顯示適量飲酒,與較低的阿茲海默症發生率相關,特別是紅酒[145]。另有證據表明咖啡因可能為阿茲海默症的保護因子[149]。含有高量黄酮类的食物,如可可、紅酒、茶,等,也可能與較低的阿茲海默症風險相關[150][151]。
目前沒有有力證據支持攝取維生素或礦物質對疾病有幫助,此部分已研究的物質包含維生素A[152][153]、C[154][155]、α-生育酚態的維生素E[156]、硒[157]、鋅[158][159]、葉酸,以及B12等[160]。一項證據品質中等的隨機分派研究指出,α-生育酚態的維生素E可以減緩認知功能下降的速度[156];而葉酸及其他維生素B的臨床試驗則無法證明有同樣功能[161]。植物油及魚油中常見的Omega-3脂肪酸,以及二十二碳六烯酸(DHA)對於改善阿茲海默症沒有已知助益[162][163]。
薑黃在動物實驗中顯示對阿茲海默症有幫助,但截至2010年為止,尚無人體實驗證實有效[164]。银杏及大麻素目前也尚無有力證據支持其在失智症的效果[165][166],但內源性大麻素(endocannabinoids)似乎有一些證據顯示有所助益[167]。
治療
目前阿茲海默症尚無根本性治療,僅有一些症狀性治療,此類療法大多屬於和緩醫療。現行治療可分為藥物治療、心理治療,以及照護品質。
藥物治療


目前用於改善阿茲海默症認知障礙的藥物有五種,其中四種為乙醯膽鹼酯酶抑制劑(達可寧、憶思能、加蘭他敏、愛憶欣),另外一種為NMDA受體拮抗劑(美金剛胺)。但這些藥物的效益都不大[6][168][169],且截至目前為止,仍沒有證據這些藥物能延緩或停止疾病的進程。
阿茲海默症會降低膽鹼性神經元的活性[170],而乙醯膽鹼酯酶抑制劑可以減緩乙醯膽鹼(ACh)的降解速率,藉此提升突觸間的乙酰胆碱濃度,已補足因膽鹼性神經元死亡而造成乙醯膽鹼濃度下降的現象[171]。目前此類藥品在輕度至中度的阿茲海默症的症狀控制上,已經證實有效[172][169][173] ,有一些證據甚至表示重度患者使用也有效果[173]。輕度知能障礙患者用藥並不能延遲阿茲海默症的發生[174]。此類藥物最常見的副作用為噁心和嘔吐,兩者皆為膽鹼過量的副作用。約10–20%的患者用藥後會產生副作用,嚴重程度從輕度到中度皆有。如有此類問題,可以緩慢調降藥量來改善[175]。比較少見的副作用包含肌肉抽搐、心搏過緩、食慾及體重下降,以及胃酸製造增加等等[172]。
麩胺酸為興奮性神經傳遞物質,若在腦中含量過多可能會引起興奮性毒性反應,使細胞因受體過度刺激而死亡。興奮性毒性反應存在於阿茲海默症、帕金森氏症,以及多發性硬化症等神經性疾病中[176]。美金剛胺為一種非競爭性NMDA受體拮抗劑,一開始被用於治療流行性感冒,但後來發現它可以藉由抑制NMDA受體來達到抑制麩胺酸系統的效果[176][177]。後來的研究顯示美金剛胺對於阿茲海默症有些許效益[178]。本品已知的不良反應包含偶爾產生輕微幻覺、意識混亂、暈眩、頭痛,以及疲勞[179]。美金剛胺與愛憶欣併用的效果統計上呈現顯著,但臨床效益不大[180]。
非典型抗精神病藥對於緩解患者的攻擊性及思覺失調症狀具有一些效果,但同時此類藥物也會造成一些嚴重副作用,例如中風、動作障礙,已及認知功能損傷等等[181]。長期使用此類藥物可能會增加死亡風險[182],而對於精神症狀輕度至中度的長期服藥者,停藥似乎為安全的選擇[183]。
石杉鹼甲對改善認知功能似乎有正面影響,但目前仍需進一步研究證實其效果[184]。
心理治療
社會心理治療可用於輔助藥物治療,分為行為性、情緒性、認知性、刺激性等介入方式。但此類治療的效度無法測量,且此類研究的研究對象大多收錄了所有失智症,鮮少明確針對阿茲海默症[185]。
行為治療乃是藉由識別問題行為的前因及結果,進而試圖減少之。此類治療雖然無法改善整體功能[186],但可以減少一些特定的問題行為,例如尿失禁[187]。但目前對於遊走(wandering)等其他問題,並沒有足夠實證顯示其效果[188][189]。音樂治療可能對於減少行為性或心理性症狀有些效果[190]。
情緒導向治療包括懷舊療法、確認療法、支持性心理治療、 感官統合(或稱為多感官治療)和情境模擬治療。一份考科藍的回顧性文章認為此類療法並無足夠實證支持效果[191]。 支持性心理治療的正式學術研究相當少,但有些治療者認為對於改善病人的病感有些許效果[185]。懷舊療法的做法是與病患引導病人回憶過去的經驗,治療者會反覆藉由照片、日常用品、音樂、錄音檔,或是病患熟悉的事物,引導病人回憶並組織過去的經驗。懷舊療法可以個別進行或以小組模式進行。一份2018年的回顧性文章認為懷舊療法的一致性不足,且對象規模過小、各團體差異過大,以致不足以彰顯其臨床意義[192]。情境模擬治療的理論是建基於依附理論上,治療者會播放病患熟悉的聲音。此療法在改善病患的挑釁行為有部分證據[193]。最後,確認療法是基於接受患者所感受到的真實和個人信念,而感官統合療法則以刺激訓練患者的感知為目標。目前沒有證據支持這些療法是否有效[194][195]。
認知導向治療的目標包含協助病人恢復現實定向(reality orientation)以及認知功能再訓練(cognitive retraining)。現實定向的做法是提供病人當下的人、事、時、地、物等現實資訊,以協助病人了解其環境。認知功能再訓練則旨在協助病人改善其心智功能。上述兩者對於改善認知能力都有一些效果[196][197],雖然在部分研究中,這些效果短暫的,負面效果如使患者感到沮喪也曾被提出[185]。
刺激導向治療(Stimulation-oriented treatments)包括以藝術、音樂、寵物、運動或其他任何娛樂活動來進行治療。刺激可以適當地協助患者改善行為、心情和少部分的功能。雖然如此,這些治療提供的支持除了其本身的效果外,患者習慣的改變也是同等重要的[185]。非侵入性腦刺激和侵入性腦刺激在阿茲海默症的效用目前還不明瞭[198]。
醫療照護
由於阿茲海默症無法治癒,且會逐漸使患者無法自理,因此照護實質上是治療的核心,在整個疾病進程中必須小心處理。在疾病早期,改善居住環境和生活模式可以增進病人安全,並減少照護者的負擔[199][200],實務上包括讓患者的生活作息符合固定簡單的模式、使用安全防護裝置、在居家物品上做標示(用以提示患者)或使用特殊設計的生活用具[185][201][202]。若有進食問題,則須將食物切成小塊或甚至做成泥狀[203];當出現吞嚥障礙時,則可能需使用餵食管,對於這樣的患者,照護者和家人必須仔細考量藥物療效和餵食與否等倫理議題[204][205]。無論是哪個階段的阿茲海默症的患者,通常都不需要身體拘束,雖然在少數狀況下,為了保護患者或照護者仍必須執行拘束[185]。
當疾病逐漸惡化,各式病症也會逐漸出現如口腔或牙科疾病、褥瘡、營養不良、衛生問題、呼吸道感染」皮膚感染、眼感染等。小心的照護管理能避免上述問題產生,但若真的發生了,則需要專業的治療[206][207]。在疾病的最末期,治療著重於在患者死亡前緩解其痛楚,通常會需要緩和醫療的協助[208]。
預後

阿茲海默症早期十分難診斷,通常要到認知障礙影響到日常生活後才會確診,雖然此時患者可能仍能獨立生活。患者的症狀會由輕度的認知功能問題(例如記憶力衰退)開始逐漸惡化,到疾病後期完全不可能獨自生活[29]。
阿茲海默症患者的預期壽命較短[209],診斷後的預期餘命約三到十年[209],少於3%的人能活超過14年[210]。會造成存活年數顯著減少的特徵包括認知障礙嚴重度增加、生活功能減退、曾經跌倒和神經學檢查出現問題。其他共病如心血管疾病、糖尿病、曾經酗酒都和存活年數減少有關[211][212][213]。雖然越年輕時就診斷的患者有越長的存活年數,但事實上年輕的患者相對於健康族群來說壽命較短[214] 。男性的預後也較女性差[210][215]。
肺炎和脫水是最常造成阿茲海默症患者立即死亡的原因;相較於一般人,阿茲海默症患者因癌症死亡的比率較少[215]。
流行病學
| 年齡 | 年發生率(每千人) |
|---|---|
| 65–69 | 3 |
| 70–74 | 6 |
| 75–79 | 9 |
| 80–84 | 23 |
| 85–89 | 40 |
| 90– | 69 |
阿茲海默症的流行病學研究主要著重在盛行率和發生率上:盛行率指的是某種疾病在任一時間點占群體總人數的比例;發生率則是指特定時期內某人群新發生某一疾病的比率。
在發生率方面,縱貫性世代研究(追蹤一群無疾病人口的發病比率)指出,每年失智症發生風險約為1-1.5%,而其中阿茲海默症的風險則為0.5-0.8%[216][217] 。這代表在每年新發生的失智症中,有幾乎一半是阿茲海默症。高齡是阿茲海默症的主要風險因子,本病在每個年齡層的發生率不同,年齡越大者發生風險越高。65歲以上的長者,每五年的罹病風險就會增加一倍[216][217]。除年齡外,阿茲海默症的發生率還存在性別差異,女性的發生率較男性為高,特別是85歲以上的年長女性[217][218]。在美國,非拉丁裔白人死於阿茲海默症的風險,比起非裔高出了26%,更比拉丁裔高出了30%[219]。
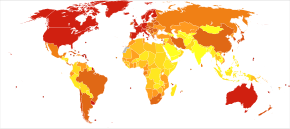
阿茲海默症的盛行率取決於許多因素,包括當地患者的存活率。由於阿茲海默症的發生率隨年齡增加,考量當地人口的平均年齡是相當重要的。美國的阿茲海默症的總人口盛行率和65–74歲的族群盛行率皆為1.6%,但在75–84歲的族群盛行率則為19%,85歲以上的族群更達到42%[220]。低度開發地區的盛行率也因此較低[221]。世界衛生組織估計2005年全球的失智症盛行率為0.379%,2015年會增加到0.441%,並在2030年達到0.556%[222];其他研究也有類似的結論[221]。另一項研究估計2006年全球約有0.40%(範圍從0.17到0.89%;實際人數約2660萬人,範圍從1140萬到5940萬人)的人口受阿茲海默症的影響,在2050年以前,盛行率會是現在的三倍,實際人數則會高達四倍[223]。
歷史

早在古希臘羅馬時代,當時的哲學家和醫師就已經發現年老與失智的關聯性[18]。1901年,德國精神科醫師愛羅斯·阿茲海默描述了第一個阿茲海默症病例。這名病患是一名名叫奧古斯特·迪特的50歲女性,阿茲海默持續追蹤迪特的病程進展至病人於1906年死亡為止,並在之後發表該病例[224]。其後五年,陸續又出現了11例類似的病例報告,其中有些論文已經用「阿茲海默症」來稱呼此疾病[18]。1910年7月15日,艾米爾·克雷珀林於《精神科學課本》(Textbook of Psychiatry)第八版中首次將這些症狀描述為一個單一疾病,並將奧古斯特的部分症狀(如幻覺和妄想)及病理特徵(血管硬化)劃出該病的描述範圍[225]。艾米爾採用了「阿茲海默症」這個名字,並同時將其稱為「早發性老年失智症」(presenile dementia)將其視為是老年失智症的一個亞型[226]。
截至1970年代為止,阿茲海默症的診斷仍然僅限於描述45至65歲之間,提早出現特定失智症狀的患者。直到1977年,一場阿茲海默症研討會共識認定,阿茲海默症和老年失智症的臨床和病理表徵大致相同。雖然同時也強調兩者的病因學可能不同[227],但這樣的共識已促使阿茲海默症的診斷,不再應該限定於特定年紀的的患者[228]。此後一段時期,超過65歲且擁有阿茲海默症症狀的患者,另被描述為「阿茲海默型老年失智症」(senile dementia of the Alzheimer type,SDAT)。如今,阿茲海默症已經被接受為醫學的正式名詞,描述各年齡患者某種共同特定症狀的病徵[229]。
社會及文化
社會成本
失智症(特別是阿茲海默症)已成為歐美社會花費最多的疾病之一[19][20],其他如阿根廷[230]和南韓[231]等國家的花費也節節攀升。這些花費可能會使社會結構老化,進而成為社會問題。與阿茲海默症有關的社會成本包括直接的醫療費用(如護理之家照護、在宅日間照護)和間接的成本(如病人和照護者生產力降低)[20]。雖然各個研究的數據有差異,但全球每年在失智症上花費約1600億美元[232],單是美國每年就可能花費了約1000億美元[20]。
社會成本最大的來源為醫療專業人員的長期照護,特別是機構照護的費用可能佔了總花費的2/3[19]。 患者在家的生活花費通常很高[19],尤其還需考慮患者家人的非正式成本,如照護時間和因照顧患者而減少的收入[233]。
隨著失智的嚴重度和行為問題增加,患者的花費將會上升[234],需要醫療照護的時間也會增加[233]。因此,任何能減緩認知功能下降、延遲機構照護或減少照護時間的治療都對經濟有幫助,目前的治療方法在經濟評估上已顯示正向的結果[20]。
照護負擔
患者的主要照護者通常是其配偶或關係較密切的親屬[235]。阿茲海默症會帶給照護者社會上、心理上、生理上,和經濟上極沉重的負擔[12][236][237]。居家照護可以延遲或減少病人接受更昂貴和更專業的照護[238][239],因此通常家屬和患者會傾向選擇居家照護[238]。但即使如此,失智症患者仍然佔了護理之家住院人數的二分之三[185]。
失智症患者的照護者罹患生理和心理疾患的機會較高[240]。 造成主要照護者有較大心理問題的因素包括患者住在家中、患者為其配偶、患者有令照護較為吃力的行為(如憂鬱、行為干擾、幻覺、睡眠問題、行走問題或社交孤立)等[241][242]。在經濟層面上,作為照護者的家人平均每週放棄47小時的工作時間來照護阿茲海默症患者,照護的代價相當高昂。在美國,每年直接和間接的照護支出從18,000到77,500美元不等,數值因研究而異[233][235]。
认知行为疗法和教導應對策略(不論是個別指導或在團體中教導)都能有效提升照護者的心裡健康[12][243]。
媒體
許多電影或影集描述過阿茲海默症,例如《長路將盡》(2001,取材自約翰·貝禮描述其妻的回憶錄)[244]、《忘了、忘不了》(2004,取材自尼可拉斯·史派克1996年的同名小說)[245]、《我腦海中的橡皮擦》(2004)、《Thanmathra》(2005)[246]、《明日的記憶》 (2006,取材自荻原浩的同名小說)[247]、《妳的樣子》(2006,取材自艾丽斯·芒罗的短篇小说《恨,友谊,追求,爱情,婚姻》)[248]、《我想念我自己》(2014,內容描述一位罹患早發型阿茲海默症的哥伦比亚大学教授,取材自莉莎·潔諾娃的同名小說,並以茱莉安·摩爾為英語的片名角色)。與阿茲海默症相關的紀錄片有《馬爾柯姆與芭芭拉:愛的故事》(1999,Malcolm and Barbara: A Love Story)和《馬爾柯姆與芭芭拉:愛的告別》(2007,Malcolm and Barbara: Love's Farewell),兩者都以鋼琴家馬爾柯姆·波因頓為主角[249][250][251]。
註釋
- ^ 在香港,Dementia已經由「老人癡呆症」改名為「認知障礙症」;而Alzheimer’s Disease則命名為「阿爾茲海默氏症」。認知障礙症成因及分類鑑於「老年癡呆症」的歧視成分及標籤效應,有礙及早求診,由十個醫學及服務團體(包括香港認知障礙症協會在內)組成的專家聯盟於2012年進行了公眾諮詢。結果顯示市民與專業團體均普遍認同「認知障礙症」更能中立、準確地反映疾病的症狀(記憶與其他認知功能問題)、不局限於成因(退化與非退化性)、較易明白且不含歧視意味。
參考文獻
- ^ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Iliffe, Steve; Burns, Alistair. Alzheimer’s disease. BMJ. 2009-02-05, 338: b158. ISSN 1468-5833. PMID 19196745. doi:10.1136/bmj.b158.
- ^ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Dementia. www.who.int. World Health Organization. [2018-12-21].
- ^ 3.0 3.1 Early-onset Alzheimer's Disease: Nonamnestic Subtypes and Type 2 AD. Archives of Medical Research. 2012-11-01, 43 (8): 677–685. ISSN 0188-4409. PMC 3532551
 . PMID 23178565. doi:10.1016/j.arcmed.2012.11.009.
. PMID 23178565. doi:10.1016/j.arcmed.2012.11.009.
- ^ 4.0 4.1 4.2 4.3 4.4 Ballard, Clive; Gauthier, Serge; Corbett, Anne; Brayne, Carol; Aarsland, Dag; Jones, Emma. Alzheimer's disease. The Lancet. 2011-03, 377 (9770): 1019–1031. ISSN 0140-6736. doi:10.1016/s0140-6736(10)61349-9.
- ^ 5.0 5.1 Dementia diagnosis and assessment (PDF). National Institute for Health and Care Excellence (NICE). [2018-12-22]. (原始内容 (PDF)存档于2014-12-05).
- ^ 6.0 6.1 Commission de la transparence. Médicaments de la maladie d'Alzheimer [Drugs for Alzheimer's disease: best avoided. No therapeutic advantage]. Prescrire International. June 2012;21(128):150. PMID 22822592.
- ^ 7.0 7.1 Querfurth, Henry W.; LaFerla, Frank M. Alzheimer's Disease. New England Journal of Medicine. 2010-01-28, 362 (4): 329–344. ISSN 0028-4793. PMID 20107219. doi:10.1056/NEJMra0909142.
- ^ About Alzheimer's Disease: Symptoms. National Institute on Aging. [28 December 2011]. (原始内容存档于15 January 2012).
- ^ Todd, Stephen; Barr, Stephen; Roberts, Mark; Passmore, A. Peter. Survival in dementia and predictors of mortality: a review. International Journal of Geriatric Psychiatry. 2013, 28 (11): 1109–1124. ISSN 1099-1166. doi:10.1002/gps.3946.
- ^ So, What Can You Do?. National Institute on Aging. 29 July 2016. (原始内容存档于3 April 2017).
- ^ 11.0 11.1 11.2 11.3 11.4 Hsu, David; Marshall, Gad A. Primary and Secondary Prevention Trials in Alzheimer Disease: Looking Back, Moving Forward. Current Alzheimer Research. 2017, 14 (4): 426–440. ISSN 1875-5828. PMC 5329133
 . PMID 27697063. doi:10.2174/1567205013666160930112125.
. PMID 27697063. doi:10.2174/1567205013666160930112125.
- ^ 12.0 12.1 12.2 Thompson, Carl A.; Spilsbury, Karen; Hall, Jill; Birks, Yvonne; Barnes, Colin; Adamson, Joy. Systematic review of information and support interventions for caregivers of people with dementia. BMC Geriatrics. 2007-07-27, 7 (1): 18. ISSN 1471-2318. PMC 1951962
 . PMID 17662119. doi:10.1186/1471-2318-7-18.
. PMID 17662119. doi:10.1186/1471-2318-7-18.
- ^ Forbes, Dorothy; Forbes, Scott C; Blake, Catherine M; Thiessen, Emily J; Forbes, Sean. Exercise programs for people with dementia. Cochrane Database of Systematic Reviews. 2015-04-15. ISSN 1465-1858. doi:10.1002/14651858.cd006489.pub4.
- ^ National Institute for Health and Clinical Excellence. Low-dose antipsychotics in people with dementia. National Institute for Health and Care Excellence (NICE). [29 November 2014]. (原始内容存档于5 December 2014).
- ^ Information for Healthcare Professionals: Conventional Antipsychotics. US Food and Drug Administration. 16 June 2008 [29 November 2014]. (原始内容存档于29 November 2014).
- ^ Vos, Theo; Allen, Christine; Arora, Megha; Barber, Ryan M; Bhutta, Zulfiqar A; Brown, Alexandria; Carter, Austin; Casey, Daniel C; Charlson, Fiona J. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016-10, 388 (10053): 1545–1602. ISSN 0140-6736. PMC 5055577
 . PMID 27733282. doi:10.1016/s0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/s0140-6736(16)31678-6.
- ^ Wang, Haidong; Naghavi, Mohsen; Allen, Christine; Barber, Ryan M; Bhutta, Zulfiqar A; Carter, Austin; Casey, Daniel C; Charlson, Fiona J; Chen, Alan Zian. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016-10, 388 (10053): 1459–1544. ISSN 0140-6736. PMC 5388903
 . PMID 27733281. doi:10.1016/s0140-6736(16)31012-1.
. PMID 27733281. doi:10.1016/s0140-6736(16)31012-1.
- ^ 18.0 18.1 18.2 Evolution in the Conceptualization of Dementia and Alzheimer’s Disease: Greco-Roman Period to the 1960s. Neurobiology of Aging. 1998-05-01, 19 (3): 173–189. ISSN 0197-4580. doi:10.1016/S0197-4580(98)00052-9.
- ^ 19.0 19.1 19.2 19.3 Impact économique de la démence (English: The Economical Impact of Dementia). Presse Médicale. 2005;34(1):35–41. French. doi:10.1016/s0755-4982(05)83882-5. PMID 15685097.
- ^ 20.0 20.1 20.2 20.3 20.4 Economic Considerations in Alzheimer's Disease. Pharmacotherapy. 1998;18(2 Pt 2):68–73; discussion 79–82. doi:10.1002/j.1875-9114.1998.tb03880.x. PMID 9543467.
- ^ Evaluating Prescription Drugs Used to Treat: Alzheimer's Disease Comparing Effectiveness, Safety, and Price (PDF). Consumer Reports Drug Effectiveness Review Project (Consumer Reports). May 2012 [1 May 2013]. (原始内容存档 (PDF)于5 September 2012). 已忽略未知参数
|df=(帮助) - ^ 22.0 22.1 22.2 22.3 Recommendations for the Diagnosis and Management of Alzheimer's Disease and Other Disorders Associated with Dementia: EFNS Guideline. European Journal of Neurology. 2007;14(1):e1–26. doi:10.1111/j.1468-1331.2006.01605.x. PMID 17222085.
- ^ 23.0 23.1 23.2 Multiple Cognitive Deficits During the Transition to Alzheimer's Disease. Journal of Internal Medicine. 2004;256(3):195–204. doi:10.1111/j.1365-2796.2004.01386.x. PMID 15324363.
- ^ Instrumental Activities of Daily Living: A Stepping-stone Towards Alzheimer's Disease Diagnosis in Subjects with Mild Cognitive Impairment?. Acta Neurologica Scandinavica. 2003;Suppl(179):42–46. doi:10.1034/j.1600-0404.107.s179.8.x. PMID 12603250.
- ^ Neuropsychological Features of Mild Cognitive Impairment and Preclinical Alzheimer's Disease. Acta Neurologica Scandinavica. 2003;179:34–41. doi:10.1034/j.1600-0404.107.s179.7.x. PMID 12603249.
- ^ Landes AM, Sperry SD, Strauss ME, Geldmacher DS. Apathy in Alzheimer's disease. J Am Geriatr Soc. Dec 2001, 49 (12): 1700–7. PMID 11844006. doi:10.1046/j.1532-5415.2001.49282.x.
- ^ Arnáiz E, Almkvist O. Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease. Acta Neurol. Scand., Suppl. 2003, 179: 34–41. PMID 12603249. doi:10.1034/j.1600-0404.107.s179.7.x.
- ^ Grundman M, Petersen RC, Ferris SH, Thomas RG, Aisen PS, Bennett DA, Foster NL, Jack CR, Galasko DR, Doody R, Kaye J, Sano M, Mohs R, Gauthier S, Kim HT, Jin S, Schultz AN, Schafer K, Mulnard R, van Dyck CH, Mintzer J, Zamrini EY, Cahn-Weiner D, Thal LJ. Mild cognitive impairment can be distinguished from Alzheimer disease and normal aging for clinical trials. Archives of Neurology. January 2004, 61 (1): 59–66. PMID 14732621. doi:10.1001/archneur.61.1.59.
- ^ 29.00 29.01 29.02 29.03 29.04 29.05 29.06 29.07 29.08 29.09 29.10 29.11 29.12 29.13 29.14 29.15 29.16 29.17 29.18 29.19 29.20 29.21 29.22 Clinical Features of Alzheimer's Disease. European Archives of Psychiatry and Clinical Neuroscience. 1999;249(6):288–90. doi:10.1007/s004060050101. PMID 10653284.
- ^ Memory Deficits in Alzheimer's Patients: A Comprehensive Review. Neuropsychology Review. 1992;3(2):119–69. doi:10.1007/BF01108841. PMID 1300219.
- ^ Implicit Memory Performance of Patients with Alzheimer's Disease: A Brief Review. International Psychogeriatrics. 1995;7(3):385–92. doi:10.1017/S1041610295002134. PMID 8821346.
- ^ 32.0 32.1 Language Performance in Alzheimer's Disease and Mild Cognitive Impairment: a comparative review. Journal of Clinical and Experimental Neuropsychology. July 2008;30(5):501–56. doi:10.1080/13803390701550128. PMID 18569251.
- ^ 33.0 33.1 33.2 Effect of Alzheimer's Disease on Communication Function. Journal of the South Carolina Medical Association. 1994;90(9):417–23. PMID 7967534.
- ^ Sundowning and Circadian Rhythms in Alzheimer's Disease. The American Journal of Psychiatry. 2001;158(5):704–11. doi:10.1176/appi.ajp.158.5.704. PMID 11329390.
- ^ When Home Caregiving Ends: A Longitudinal Study of Outcomes for Caregivers of Relatives with Dementia. Journal of the American Geriatrics Society. 1995;43(1):10–16. doi:10.1111/j.1532-5415.1995.tb06235.x. PMID 7806732.
- ^ What We Know Today About Alzheimer's Disease. Alzheimer's Association. [1 October 2011]. (原始内容存档于7 October 2011).
While scientists know Alzheimer's disease involves progressive brain cell failure, the reason cells fail isn't clear.
- ^ Reitz C, Mayeux R. Alzheimer disease: epidemiology, diagnostic criteria, risk factors and biomarkers. Biochemical Pharmacology. April 2014, 88 (4): 640–51. PMC 3992261
 . PMID 24398425. doi:10.1016/j.bcp.2013.12.024.
. PMID 24398425. doi:10.1016/j.bcp.2013.12.024.
- ^ Heritability of different forms of memory in the Late Onset Alzheimer's Disease Family Study.. Journal of Alzheimer's Disease. 2011;23(2):249–55. doi:10.3233/JAD-2010-101515. PMID 20930268.
- ^ Role of genes and environments for explaining Alzheimer disease. Arch. Gen. Psychiatry. 2006;63(2):168–74. doi:10.1001/archpsyc.63.2.168. PMID 16461860.
- ^ 40.0 40.1 40.2 Alzheimer's Disease. Lancet. 2006;368(9533):387–403. doi:10.1016/S0140-6736(06)69113-7. PMID 16876668.
- ^ 41.0 41.1 Genome-wide association studies in Alzheimer disease. Archives of Neurology. 2008;65(3):329–34. doi:10.1001/archneur.65.3.329. PMID 18332245.
- ^ Translating cell biology into therapeutic advances in Alzheimer's disease. Nature. 1999;399(6738 Suppl):A23–31. doi:10.1038/19866. PMID 10392577.
- ^ Familial Alzheimer's disease-linked presenilin 1 variants elevate βA1-42/1-40 ratio in vitro and in vivo [PDF]. Neuron. 1996;17(5):1005–13. doi:10.1016/S0896-6273(00)80230-5. PMID 8938131.
- ^ FAD mutants unable to increase neurotoxic Aβ 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta. Journal of Neurochemistry. 2007;101(3):674–81. doi:10.1111/j.1471-4159.2006.04391.x. PMID 17254019.
- ^ Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(5):1977–81. doi:10.1073/pnas.90.5.1977. PMID 8446617.
- ^ 46.0 46.1 Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer's disease. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(15):5644–51. doi:10.1073/pnas.0600549103. PMID 16567625.
- ^ Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba. Neurology. 2006;66(2):223–27. doi:10.1212/01.wnl.0000194507.39504.17. PMID 16434658.
- ^ APOE ε4 is not associated with Alzheimer's disease in elderly Nigerians. Annals of Neurology. 2006;59(1):182–85. doi:10.1002/ana.20694. PMID 16278853.
- ^ 49.0 49.1 Lambert JC, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, DeStafano AL, Bis JC, Beecham GW, Grenier-Boley B, Russo G, Thorton-Wells TA, Jones N, Smith AV, Chouraki V, Thomas C, Ikram MA, Zelenika D, Vardarajan BN, Kamatani Y, Lin CF, Gerrish A, Schmidt H, Kunkle B, Dunstan ML, Ruiz A, Bihoreau MT, Choi SH, Reitz C, Pasquier F, Cruchaga C, Craig D, Amin N, Berr C, Lopez OL, De Jager PL, Deramecourt V, Johnston JA, Evans D, Lovestone S, Letenneur L, Morón FJ, Rubinsztein DC, Eiriksdottir G, Sleegers K, Goate AM, Fiévet N, Huentelman MW, Gill M, Brown K, Kamboh MI, Keller L, Barberger-Gateau P, McGuiness B, Larson EB, Green R, Myers AJ, Dufouil C, Todd S, Wallon D, Love S, Rogaeva E, Gallacher J, St George-Hyslop P, Clarimon J, Lleo A, Bayer A, Tsuang DW, Yu L, Tsolaki M, Bossù P, Spalletta G, Proitsi P, Collinge J, Sorbi S, Sanchez-Garcia F, Fox NC, Hardy J, Deniz Naranjo MC, Bosco P, Clarke R, Brayne C, Galimberti D, Mancuso M, Matthews F, Moebus S, Mecocci P, Del Zompo M, Maier W, Hampel H, Pilotto A, Bullido M, Panza F, Caffarra P, Nacmias B, Gilbert JR, Mayhaus M, Lannefelt L, Hakonarson H, Pichler S, Carrasquillo MM, Ingelsson M, Beekly D, Alvarez V, Zou F, Valladares O, Younkin SG, Coto E, Hamilton-Nelson KL, Gu W, Razquin C, Pastor P, Mateo I, Owen MJ, Faber KM, Jonsson PV, Combarros O, O'Donovan MC, Cantwell LB, Soininen H, Blacker D, Mead S, Mosley TH, Bennett DA, Harris TB, Fratiglioni L, Holmes C, de Bruijn RF, Passmore P, Montine TJ, Bettens K, Rotter JI, Brice A, Morgan K, Foroud TM, Kukull WA, Hannequin D, Powell JF, Nalls MA, Ritchie K, Lunetta KL, Kauwe JS, Boerwinkle E, Riemenschneider M, Boada M, Hiltuenen M, Martin ER, Schmidt R, Rujescu D, Wang LS, Dartigues JF, Mayeux R, Tzourio C, Hofman A, Nöthen MM, Graff C, Psaty BM, Jones L, Haines JL, Holmans PA, Lathrop M, Pericak-Vance MA, Launer LJ, Farrer LA, van Duijn CM, Van Broeckhoven C, Moskvina V, Seshadri S, Williams J, Schellenberg GD, Amouyel P. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nature Genetics. December 2013, 45 (12): 1452–8. PMC 3896259
 . PMID 24162737. doi:10.1038/ng.2802.
. PMID 24162737. doi:10.1038/ng.2802.
- ^ Variant of TREM2 associated with the risk of Alzheimer's disease. The New England Journal of Medicine. 2012;368(2):107–16. doi:10.1056/NEJMoa1211103. PMID 23150908.
- ^ TREM2 variants in Alzheimer's disease. The New England Journal of Medicine. 2012;368(2):117–27. doi:10.1056/NEJMoa1211851. PMID 23150934.
- ^ Crane, Paul K.; Larson, Eric B.; Keene, C. Dirk; Bennett, David A.; Jager, Philip L. De; Lopez, Oscar L.; Kamboh, M. Ilyas; Snitz, Beth E.; McCurry, Susan M. Genetic data and cognitively defined late-onset Alzheimer’s disease subgroups. Molecular Psychiatry. 2018-12-04: 1. ISSN 1476-5578. doi:10.1038/s41380-018-0298-8.
- ^ The Cholinergic Hypothesis of Alzheimer's Disease: a Review of Progress. Journal of Neurology, Neurosurgery, and Psychiatry. 1999;66(2):137–47. doi:10.1136/jnnp.66.2.137. PMID 10071091.
- ^ Martorana A, Esposito Z, Koch G. Beyond the cholinergic hypothesis: do current drugs work in Alzheimer's disease?. CNS Neuroscience & Therapeutics. August 2010, 16 (4): 235–45. PMID 20560995. doi:10.1111/j.1755-5949.2010.00175.x.
- ^ Amyloid Deposition as the Central Event in the Aetiology of Alzheimer's Disease. Trends in Pharmacological Sciences. 1991;12(10):383–88. doi:10.1016/0165-6147(91)90609-V. PMID 1763432.
- ^ 56.0 56.1 Alzheimer's disease-do tauists and baptists finally shake hands?. Trends in Neurosciences. 2002;25(1):22–26. doi:10.1016/S0166-2236(00)02031-2. PMID 11801334.
- ^ Alpha- and Beta-secretase Activity as a Function of Age and Beta-amyloid in Down Syndrome and Normal Brain. Neurobiology of Aging. 2007;28(10):1493–506. doi:10.1016/j.neurobiolaging.2006.06.023. PMID 16904243.
- ^ Alzheimer Disease and Down Syndrome: Factors in Pathogenesis. Neurobiology of Aging. 2005;26(3):383–89. doi:10.1016/j.neurobiolaging.2004.08.005. PMID 15639317.
- ^ Apolipoprotein E, Dementia, and Cortical Deposition of Beta-amyloid Protein. The New England Journal of Medicine. 1995;333(19):1242–47. doi:10.1056/NEJM199511093331902. PMID 7566000.
- ^ 基因轉殖鼠相關文獻:
- Alzheimer-type Neuropathology in Transgenic Mice Overexpressing V717F Beta-amyloid Precursor Protein. Nature. 1995;373(6514):523–27. doi:10.1038/373523a0. PMID 7845465.
- Comparison of Neurodegenerative Pathology in Transgenic Mice Overexpressing V717F Beta-amyloid Precursor Protein and Alzheimer's Disease. The Journal of Neuroscience. 1996;16(18):5795–811. PMID 8795633.
- Correlative Memory Deficits, Abeta Elevation, and Amyloid Plaques in Transgenic Mice. Science. 1996;274(5284):99–102. doi:10.1126/science.274.5284.99. PMID 8810256.
- Spatial Learning, Exploration, Anxiety, and Motor Coordination in Female APP23 Transgenic Mice with the Swedish Mutation. Brain Research. 2002;956(1):36–44. doi:10.1016/S0006-8993(02)03476-5. PMID 12426044.
- ^ Long-term Effects of Abeta42 Immunisation in Alzheimer's Disease: Follow-up of a Randomised, Placebo-controlled Phase I Trial. Lancet. 2008;372(9634):216–23. doi:10.1016/S0140-6736(08)61075-2. PMID 18640458.
- ^ Aß Oligomer-Induced Aberrations in Synapse Composition, Shape, and Density Provide a Molecular Basis for Loss of Connectivity in Alzheimer's Disease. The Journal of Neuroscience. 2007;27(4):796–807. doi:10.1523/JNEUROSCI.3501-06.2007. PMID 17251419.
- ^ Lauren J; Gimbel D; et al. Cellular Prion Protein Mediates Impairment of Synaptic Plasticity by Amyloid-β Oligomers. Nature. February 2009, 457 (7233): 1128–32 [2012-12-23]. PMC 2748841
 . PMID 19242475. doi:10.1038/nature07761.
. PMID 19242475. doi:10.1038/nature07761.
- ^ 64.0 64.1 APP Binds DR6 to Cause Axon Pruning and Neuron Death via Distinct Caspases. Nature. 19 February 2009;457(7232):981–89. doi:10.1038/nature07767. PMID 19225519.
- ^ Graham, Rona K.; Deng, Yu; Slow, Elizabeth J.; Haigh, Brendan; Bissada, Nagat; Lu, Ge; Pearson, Jacqueline; Shehadeh, Jacqueline; Bertram, Lisa. Cleavage at the caspase-6 site is required for neuronal dysfunction and degeneration due to mutant huntingtin. Cell. 2006-06-16, 125 (6): 1179–1191. ISSN 0092-8674. PMID 16777606. doi:10.1016/j.cell.2006.04.026.
- ^ Feuerstein, Adam. "Merck Alzheimer's Drug Study Halted Early for Futility". New York City, NY, USA: TheStreet, Inc. 14 February 2017. (原始内容存档于16 February 2017).Merck Alzheimer's Drug Study Halted Early for Futility Independent study monitors concluded that there was "virtually no chance of finding a positive clinical effect."
- ^ Tau Proteins and Neurofibrillary Degeneration. Brain Pathology. 1991;1(4):279–86. doi:10.1111/j.1750-3639.1991.tb00671.x. PMID 1669718.
- ^ Tau Pathology in Alzheimer Disease and Other Tauopathies. Biochimica et Biophysica Acta. 2005;1739(2–3):198–210. doi:10.1016/j.bbadis.2004.09.008. PMID 15615638.
- ^ The Role of Tau Phosphorylation and Cleavage in Neuronal Cell Death. Frontiers in Bioscience. 2007;12:733–56. doi:10.2741/2097. PMID 17127334.
- ^ Deane R, Zlokovic BV. Role of the blood-brain barrier in the pathogenesis of Alzheimer's disease. Current Alzheimer Research. April 2007, 4 (2): 191–7. PMID 17430246. doi:10.2174/156720507780362245.
- ^ Interactions of metals and Apolipoprotein E in Alzheimer's disease. Frontiers in Aging Neuroscience. 12 June 2014;6:121. doi:10.3389/fnagi.2014.00121. PMID 24971061. "Although we still do not know if the metal ion dyshomeostasis present in AD is a cause or consequence of the disease, there is a growing body of evidence showing a direct correlation between metal ions and key AD-related key proteins."
- ^ Oxidative Stress Signaling in Alzheimer's Disease. Current Alzheimer Research. December 2008;5(6):525–32. doi:10.2174/156720508786898451. PMID 19075578.
- ^ Plant Metal Chaperones: A Novel Perspective in Dementia Therapy. Amyloid. 2009;16(2):81–83. doi:10.1080/13506120902879392. PMID 20536399.
- ^ Aluminium and Alzheimer's disease. Facts about dementia. Alzheimer's Society. [14 October 2005]. (原始内容存档于27 October 2005).
- ^ Bondy SC. Low levels of aluminum can lead to behavioral and morphological changes associated with Alzheimer's disease and age-related neurodegeneration. Neurotoxicology. January 2016, 52: 222–9. PMID 26687397. doi:10.1016/j.neuro.2015.12.002.
- ^ Kandimalla R, Vallamkondu J, Corgiat EB, Gill KD. Understanding Aspects of Aluminum Exposure in Alzheimer's Disease Development. Brain Pathology. March 2016, 26 (2): 139–54. PMID 26494454. doi:10.1111/bpa.12333.
- ^ Occupational Risk Factors in Alzheimer's Disease: A Review Assessing the Quality of Published Epidemiological Studies. Occupational and Environmental Medicine. 2007;64(11):723–32. doi:10.1136/oem.2006.028209. PMID 17525096.
- ^ 78.0 78.1 Lidsky TI. Is the Aluminum Hypothesis dead?. Journal of Occupational and Environmental Medicine. May 2014, 56 (5 Suppl): S73–9. PMC 4131942
 . PMID 24806729. doi:10.1097/jom.0000000000000063.
. PMID 24806729. doi:10.1097/jom.0000000000000063.
- ^ Yegambaram M, Manivannan B, Beach TG, Halden RU. Role of environmental contaminants in the etiology of Alzheimer's disease: a review. Current Alzheimer Research. 2015, 12 (2): 116–46. PMC 4428475
 . PMID 25654508. doi:10.2174/1567205012666150204121719.
. PMID 25654508. doi:10.2174/1567205012666150204121719.
- ^ Cigarette smoking is a risk factor for Alzheimer's disease: An analysis controlling for tobacco industry affiliation. Journal of Alzheimer's Disease. 2010;19(2):465–80. doi:10.3233/JAD-2010-1240. PMID 20110594.
- ^ Neuroinflammation – An Early Event in Both the History and Pathogenesis of Alzheimer's Disease. Neuro-Degenerative Diseases. 2010;7(1–3):38–41. doi:10.1159/000283480. PMID 20160456.
- ^ Air Pollution, Oxidative Stress, and Alzheimer's Disease. Journal of Environmental and Public Health. 2012;2012:472751. doi:10.1155/2012/472751. PMID 22523504.
- ^ Miklossy J. Alzheimer's disease – a neurospirochetosis. Analysis of the evidence following Koch's and Hill's criteria. Journal of Neuroinflammation. August 2011, 8 (1): 90. PMC 3171359
 . PMID 21816039. doi:10.1186/1742-2094-8-90.
. PMID 21816039. doi:10.1186/1742-2094-8-90.
- ^ Pisa D, Alonso R, Rábano A, Rodal I, Carrasco L. Different Brain Regions are Infected with Fungi in Alzheimer's Disease. Scientific Reports. October 2015, 5 (1): 15015. PMC 4606562
 . PMID 26468932. doi:10.1038/srep15015 (英语).
. PMID 26468932. doi:10.1038/srep15015 (英语).
- ^ Bartzokis G. Alzheimer's disease as homeostatic responses to age-related myelin breakdown. Neurobiology of Aging. August 2011, 32 (8): 1341–71. PMC 3128664
 . PMID 19775776. doi:10.1016/j.neurobiolaging.2009.08.007.
. PMID 19775776. doi:10.1016/j.neurobiolaging.2009.08.007.
- ^ Cai Z, Xiao M. Oligodendrocytes and Alzheimer's disease. The International Journal of Neuroscience. 2016, 126 (2): 97–104. PMID 26000818. doi:10.3109/00207454.2015.1025778.
- ^ 87.0 87.1 87.2 Reisberg B, Franssen EH, Hasan SM, Monteiro I, Boksay I, Souren LE, Kenowsky S, Auer SR, Elahi S, Kluger A. Retrogenesis: clinical, physiologic, and pathologic mechanisms in brain aging, Alzheimer's and other dementing processes. European Archives of Psychiatry and Clinical Neuroscience. 1999,. 249 Suppl 3 (3): 28–36. PMID 10654097. doi:10.1007/pl00014170. (原始内容存档于19 September 2016). 已忽略未知参数
|df=(帮助) - ^ Alves GS, Oertel Knöchel V, Knöchel C, Carvalho AF, Pantel J, Engelhardt E, Laks J. Integrating retrogenesis theory to Alzheimer's disease pathology: insight from DTI-TBSS investigation of the white matter microstructural integrity. BioMed Research International. 2015, 2015: 291658. PMC 4320890
 . PMID 25685779. doi:10.1155/2015/291658.
. PMID 25685779. doi:10.1155/2015/291658.
- ^ Brenner Carson, Verna. Caregiving for Alzheimer's Disease. New York: Springer New York Academy of Sciences. 2015: 1–9. ISBN 978-1-4939-2406-6.
- ^ 引证错误:没有为名为
pmid12934968的参考文献提供内容 - ^ Where, when, and in what form does sporadic Alzheimer's disease begin?. Current Opinion in Neurology. December 2012;25(Pt 6):708–14. doi:10.1097/WCO.0b013e32835a3432. PMID 23160422.
- ^ Automated MRI Measures Identify Individuals with Mild Cognitive Impairment and Alzheimer's Disease. Brain. August 2009;132(Pt 8):2048–57. doi:10.1093/brain/awp123. PMID 19460794.
- ^ Moan R. MRI Software Accurately IDs Preclinical Alzheimer's Disease. Diagnostic Imaging. 20 July 2009 [archived 16 May 2016; cited 7 January 2013].
- ^ 94.0 94.1 The Importance of Neuritic Plaques and Tangles to the Development and Evolution of AD. Neurology. 2004;62(11):1984–89. doi:10.1212/01.WNL.0000129697.01779.0A. PMID 15184601.
- ^ Regional Distribution of Neurofibrillary Tangles and Senile Plaques in the Cerebral Cortex of Elderly Patients: A Quantitative Evaluation of a One-year Autopsy Population from a Geriatric Hospital. Cerebral Cortex. 1994;4(2):138–50. doi:10.1093/cercor/4.2.138. PMID 8038565.
- ^ Lewy Body Pathology in Alzheimer's Disease. Journal of Molecular Neuroscience. 2001;17(2):225–32. doi:10.1385/JMN:17:2:225. PMID 11816795.
- ^ Role of Protein Aggregation in Mitochondrial Dysfunction and Neurodegeneration in Alzheimer's and Parkinson's Diseases. Neuromolecular Medicine. 2003;4(1–2):21–36. doi:10.1385/NMM:4:1-2:21. PMID 14528050.
- ^ Synapse Formation and Function is Modulated by the Amyloid Precursor Protein. The Journal of Neuroscience. 2006;26(27):7212–21. doi:10.1523/JNEUROSCI.1450-06.2006. PMID 16822978.
- ^ Roles of Amyloid Precursor Protein and its Fragments in Regulating Neural Activity, Plasticity and Memory. Progress in Neurobiology. 2003;70(1):1–32. doi:10.1016/S0301-0082(03)00089-3. PMID 12927332.
- ^ Roles of Proteolysis and Lipid Rafts in the Processing of the Amyloid Precursor Protein and Prion Protein. Biochemical Society Transactions. 2005;33(Pt 2):335–38. doi:10.1042/BST0330335. PMID 15787600.
- ^ Amyloid Fibrils from the Viewpoint of Protein Folding. Cellular and Molecular Life Sciences. 2004;61(5):511–24. doi:10.1007/s00018-003-3264-8. PMID 15004691.
- ^ Tauopathies. Cellular and Molecular Life Sciences. 2007;64(17):2219–33. doi:10.1007/s00018-007-7220-x. PMID 17604998.
- ^ Šimić, Goran; Babić Leko, Mirjana; Wray, Selina; Harrington, Charles; Delalle, Ivana; Jovanov-Milošević, Nataša; Bažadona, Danira; Buée, Luc; de Silva, Rohan. Tau Protein Hyperphosphorylation and Aggregation in Alzheimer’s Disease and Other Tauopathies, and Possible Neuroprotective Strategies. Biomolecules. 2016-01-06, 6 (1). ISSN 2218-273X. PMC 4808800
 . PMID 26751493. doi:10.3390/biom6010006.
. PMID 26751493. doi:10.3390/biom6010006.
- ^ Sun, Wenyan; Samimi, Hanie; Gamez, Maria; Zare, Habil; Frost, Bess. Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies. Nature Neuroscience. 23 July 2018, 21 (8): 1038–48. PMC 6095477
 . PMID 30038280. doi:10.1038/s41593-018-0194-1.
. PMID 30038280. doi:10.1038/s41593-018-0194-1.
- ^ Current Insights into Molecular Mechanisms of Alzheimer Disease and Their Implications for Therapeutic Approaches. Neuro-Degenerative Diseases. 2007;4(5):349–65. doi:10.1159/000105156. PMID 17622778.
- ^ Alzheimer Mechanisms and Therapeutic strategies. Cell. 2012;148(6):1204–22. doi:10.1016/j.cell.2012.02.040. PMID 22424230.
- ^ Neurotrophic and Neurotoxic Effects of Amyloid Beta Protein: Reversal by Tachykinin Neuropeptides. Science. 1990;250(4978):279–82. doi:10.1126/science.2218531. PMID 2218531.
- ^ Mitochondrial Abeta: A Potential Cause of Metabolic Dysfunction in Alzheimer's Disease. IUBMB Life. 2006;58(12):686–94. doi:10.1080/15216540601047767. PMID 17424907.
- ^ New Therapeutic Strategies and Drug Candidates for Neurodegenerative Diseases: p53 and TNF-alpha Inhibitors, and GLP-1 Receptor Agonists. Annals of the New York Academy of Sciences. 2004;1035:290–315. doi:10.1196/annals.1332.018. PMID 15681814.
- ^ Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T, Vitorica J, Ransohoff RM, Herrup K, Frautschy SA, Finsen B, Brown GC, Verkhratsky A, Yamanaka K, Koistinaho J, Latz E, Halle A, Petzold GC, Town T, Morgan D, Shinohara ML, Perry VH, Holmes C, Bazan NG, Brooks DJ, Hunot S, Joseph B, Deigendesch N, Garaschuk O, Boddeke E, Dinarello CA, Breitner JC, Cole GM, Golenbock DT, Kummer MP. Neuroinflammation in Alzheimer's disease. The Lancet. Neurology. April 2015, 14 (4): 388–405. PMID 25792098. doi:10.1016/S1474-4422(15)70016-5.
- ^ New insights into brain BDNF function in normal aging and Alzheimer disease. Brain Research Reviews. 2008;59(1):201–20. doi:10.1016/j.brainresrev.2008.07.007. PMID 18708092.
- ^ Neurotrophic factors in Alzheimer's disease: role of axonal transport. Genes, Brain, and Behavior. 2008;7(Suppl 1):43–56. doi:10.1111/j.1601-183X.2007.00378.x. PMID 18184369.
- ^ The Accurate Diagnosis of Early-onset Dementia. International Journal of Psychiatry in Medicine. 2006;36(4):401–12. doi:10.2190/Q6J4-R143-P630-KW41. PMID 17407994.
- ^ Therapeutic Approaches to Alzheimer's Disease. Brain. 2006;129(Pt 11):2840–55. doi:10.1093/brain/awl280. PMID 17018549.
- ^ Dementia: Quick Reference Guide (PDF). London: (UK) National Institute for Health and Clinical Excellence. November 2006 [22 February 2008]. ISBN 1-84629-312-X. (原始内容 (PDF)存档于27 February 2008).
- ^ Neural Correlates of Alzheimer's Disease and Mild Cognitive Impairment: A Systematic and Quantitative Meta-Analysis involving 1,351 Patients. NeuroImage. 2009;47(4):1196–206. doi:10.1016/j.neuroimage.2009.05.037. PMID 19463961.
- ^ 117.0 117.1 Clinical Diagnosis of Alzheimer's Disease: Report of the NINCDS-ADRDA Work Group under the Auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34(7):939–44. doi:10.1212/wnl.34.7.939. PMID 6610841.
- ^ Research Criteria for the Diagnosis of Alzheimer's Disease: Revising the NINCDS-ADRDA Criteria. Lancet Neurology. 2007;6(8):734–46. doi:10.1016/S1474-4422(07)70178-3. PMID 17616482.
- ^ Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative. Archives of Neurology. 1994;51(12):1198–204. doi:10.1001/archneur.1994.00540240042014. PMID 7986174.
- ^ American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR 4th Edition Text Revision. Washington, DC: American Psychiatric Association. 2000. ISBN 0-89042-025-4.
- ^ [Clinical aspects of dementia]. Hokkaido Igaku Zasshi. 1996;71(3):315–20. Japanese. PMID 8752526.
- ^ The mini-mental state examination: a comprehensive review. Journal of the American Geriatrics Society. 1992;40(9):922–35. doi:10.1111/j.1532-5415.1992.tb01992.x. PMID 1512391.
- ^ Early diagnosis of dementia: neuropsychology. Journal of Neurology. 1999;246(1):6–15. doi:10.1007/s004150050299. PMID 9987708.
- ^ The Validation of a Caregiver Assessment of Dementia: the Dementia Severity Scale. Alzheimer Disease and Associated Disorders. 2005;19(4):186–94. doi:10.1097/01.wad.0000189034.43203.60. PMID 16327345.
- ^ Awareness of Deficits and Anosognosia in Alzheimer's Disease. L'Encéphale. 2004;30(6):570–77. French. doi:10.1016/S0013-7006(04)95472-3. PMID 15738860.
- ^ The Initial Symptoms of Alzheimer Disease: Caregiver Perception. Acta Médica Portuguesa. 2004;17(6):435–44. Portuguese. PMID 16197855.
- ^ The Decreasing Prevalence of Reversible Dementias: An Updated Meta-analysis. Archives of Internal Medicine. 2003;163(18):2219–29. doi:10.1001/archinte.163.18.2219. PMID 14557220.
- ^ Amyloid-Associated Depression: A Prodromal Depression of Alzheimer Disease?. Archives of General Psychiatry. 2008;65(5):542–50. doi:10.1001/archpsyc.65.5.542. PMID 18458206. PMC 3042807.
- ^ Differential Diagnosis of Alzheimer's Disease. Neurology. 1997;48(5 Suppl 6):S2–9. doi:10.1212/WNL.48.5_Suppl_6.2S. PMID 9153154.
- ^ Contribution of Depression to Cognitive Impairment and Dementia in Older adults. The Neurologist. 2007;13(3):105–17. doi:10.1097/01.nrl.0000252947.15389.a9. PMID 17495754.
- ^ Zhang S, Smailagic N, Hyde C, Noel-Storr AH, Takwoingi Y, McShane R, Feng J. (11)C-PIB-PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI). The Cochrane Database of Systematic Reviews. July 2014, (7): CD010386. PMID 25052054. doi:10.1002/14651858.CD010386.pub2.
- ^ Smailagic N, Vacante M, Hyde C, Martin S, Ukoumunne O, Sachpekidis C. ¹⁸F-FDG PET for the early diagnosis of Alzheimer's disease dementia and other dementias in people with mild cognitive impairment (MCI). The Cochrane Database of Systematic Reviews. January 2015, 1: CD010632. PMID 25629415. doi:10.1002/14651858.CD010632.pub2.
- ^ Diagnosis and Treatment of Dementia: 1. Risk Assessment and Primary Prevention of Alzheimer Disease. Canadian Medical Association Journal. 2008;178(5):548–56. doi:10.1503/cmaj.070796. PMID 18299540.
- ^ Cardiovascular Risk Factors for Alzheimer's Disease. The American Journal of Geriatric Cardiology. 2007;16(3):143–49. doi:10.1111/j.1076-7460.2007.06696.x. PMID 17483665.
- ^ Statins and Dementia. Current Atherosclerosis Reports. 2007;9(2):154–61. doi:10.1007/s11883-007-0012-9. PMID 17877925.
- ^ McGuinness B, Craig D, Bullock R, Malouf R, Passmore P. Statins for the treatment of dementia. The Cochrane Database of Systematic Reviews. July 2014, 7 (7): CD007514. PMID 25004278. doi:10.1002/14651858.CD007514.pub3.
- ^ NSAIDs for the Chemoprevention of Alzheimer's Disease. Sub-Cellular Biochemistry. 2007;42:229–48. doi:10.1007/1-4020-5688-5_11. PMID 17612054.
- ^ Hoozemans JJ, Veerhuis R, Rozemuller JM, Eikelenboom P. Soothing the inflamed brain: effect of non-steroidal anti-inflammatory drugs on Alzheimer's disease pathology. CNS & Neurological Disorders Drug Targets. February 2011, 10 (1): 57–67. PMID 21143138. doi:10.2174/187152711794488665.
- ^ Long term hormone therapy for perimenopausal and postmenopausal women. The Cochrane Database of Systematic Reviews. 2017;1:CD004143. doi:10.1002/14651858.CD004143.pub5. PMID 28093732.
- ^ 140.0 140.1 Cognitive reserve and Alzheimer disease. Alzheimer Disease and Associated Disorders. July 2006;20(2):112–17. doi:10.1097/01.wad.0000213815.20177.19. PMID 16917199.
- ^ 141.0 141.1 Systematic Review of the Effect of Education on Survival in Alzheimer's Disease. International Psychogeriatrics. 2009;21(1):25–32. doi:10.1017/S1041610208008053. PMID 19026089.
- ^ Neergaard, Lauran. Speaking 2 Languages May Delay Getting Alzheimer's. The Denver Post. Associated Press. 19 February 2011. (原始内容存档于2 May 2014).
- ^ Cheng ST. Cognitive Reserve and the Prevention of Dementia: the Role of Physical and Cognitive Activities. Current Psychiatry Reports. September 2016, 18 (9): 85. PMC 4969323
 . PMID 27481112. doi:10.1007/s11920-016-0721-2.
. PMID 27481112. doi:10.1007/s11920-016-0721-2.
- ^ Farina N, Rusted J, Tabet N. The effect of exercise interventions on cognitive outcome in Alzheimer's disease: a systematic review. International Psychogeriatrics. January 2014, 26 (1): 9–18. PMID 23962667. doi:10.1017/S1041610213001385.
- ^ 145.0 145.1 145.2 Nutrition and the Risk of Alzheimer's Disease. BioMed Research International. 2013;2013. doi:10.1155/2013/524820. PMID 23865055.
- ^ Diet and Alzheimer's disease risk factors or prevention: the current evidence. Expert Review of Neurotherapeutics. May 2011;11(5):677–708. doi:10.1586/ern.11.56. PMID 21539488.
- ^ Western diet consumption and cognitive impairment: links to hippocampal dysfunction and obesity. Physiology & Behavior. 18 April 2011;103(1):59–68. doi:10.1016/j.physbeh.2010.12.003. PMID 21167850.
- ^ Lifestyle-related Factors in Predementia and Dementia Syndromes. Expert Review of Neurotherapeutics. 2008;8(1):133–58. doi:10.1586/14737175.8.1.133. PMID 18088206.
- ^ Caffeine intake and dementia: systematic review and meta-analysis. Journal of Alzheimer's Disease. 2010;20 Suppl 1:S187–204. doi:10.3233/JAD-2010-091387. PMID 20182026.
- ^ The neuroprotective effects of cocoa flavanol and its influence on cognitive performance. British Journal of Clinical Pharmacology. July 2012;75(3):n/a–n/a. doi:10.1111/j.1365-2125.2012.04378.x. PMID 22775434.
- ^ [Dietary flavonoids and human health]. Annales Pharmaceutiques Françaises. March 2011;69(2):78–90. doi:10.1016/j.pharma.2010.11.004. PMID 21440100.
- ^ Vitamin A and Alzheimer's disease. Geriatrics & Gerontology International. April 2012;12(2):180–88. doi:10.1111/j.1447-0594.2011.00786.x. PMID 22221326.
- ^ Retinoids for treatment of Alzheimer's disease. BioFactors. Mar–April 2012;38(2):84–89. doi:10.1002/biof.196. PMID 22419567.
- ^ The possible role of antioxidant vitamin C in Alzheimer's disease treatment and prevention. American Journal of Alzheimer's Disease & Other Dementias. March 2013;28(2):120–25. doi:10.1177/1533317512473193. PMID 23307795.
- ^ Vitamin C and Vitamin E for Alzheimer's Disease. The Annals of Pharmacotherapy. 2005;39(12):2073–80. doi:10.1345/aph.1E495. PMID 16227450.
- ^ 156.0 156.1 Farina, Nicolas; Llewellyn, David; Isaac, Mokhtar Gad El Kareem Nasr; Tabet, Naji. Vitamin E for Alzheimer's dementia and mild cognitive impairment. The Cochrane Database of Systematic Reviews. 2017, 4: CD002854. ISSN 1469-493X. PMID 28418065. doi:10.1002/14651858.CD002854.pub5.
- ^ Selenium and Alzheimer's disease: a systematic review. Journal of Alzheimer's Disease. 2011;26(1):81–104. doi:10.3233/JAD-2011-110414. PMID 21593562.
- ^ Zinc diet and Alzheimer's disease: a systematic review. Nutritional Neuroscience. 1 September 2012;15(5):2–12. doi:10.1179/1476830512Y.0000000010. PMID 22583839.
- ^ Avan A, Hoogenraad TU. Zinc and Copper in Alzheimer's Disease. Journal of Alzheimer's Disease (Review). 2015, 46 (1): 89–92. PMID 25835420. doi:10.3233/JAD-150186.
- ^ Folic Acid with or without Vitamin B12 for the Prevention and Treatment of Healthy Elderly and Demented people. The Cochrane Database of Systematic Reviews. 2008;(4):CD004514. doi:10.1002/14651858.CD004514.pub2. PMID 18843658.
- ^ Effect of Folic Acid, with or without other B vitamins, on Cognitive Decline: Meta-analysis of Randomized trials. The American Journal of Medicine. June 2010;123(6):522–27.e2. doi:10.1016/j.amjmed.2010.01.017. PMID 20569758.
- ^ Docosahexaenoic acid homeostasis, brain aging and Alzheimer's disease: Can we reconcile the evidence?. Prostaglandins, Leukotrienes, and Essential Fatty Acids. January 2013;88(1):61–70. doi:10.1016/j.plefa.2012.04.006. PMID 22575581.
- ^ Burckhardt M, Herke M, Wustmann T, Watzke S, Langer G, Fink A. Omega-3 fatty acids for the treatment of dementia. The Cochrane Database of Systematic Reviews. April 2016, 4: CD009002. PMID 27063583. doi:10.1002/14651858.CD009002.pub3.
- ^ Curcumin and Alzheimer's disease. CNS Neuroscience & Therapeutics. October 2010;16(5):285–97. doi:10.1111/j.1755-5949.2010.00147.x. PMID 20406252.
- ^ Ginkgo Biloba for Cognitive Impairment and Dementia. The Cochrane Database of Systematic Reviews. 2009;(1):CD003120. doi:10.1002/14651858.CD003120.pub3. PMID 19160216.
- ^ Cannabinoids for the treatment of dementia. The Cochrane Database of Systematic Reviews. 2009;(2):CD007204. doi:10.1002/14651858.CD007204.pub2. PMID 19370677.
- ^ Bilkei-Gorzo A. The endocannabinoid system in normal and pathological brain ageing. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. December 2012, 367 (1607): 3326–41. PMC 3481530
 . PMID 23108550. doi:10.1098/rstb.2011.0388.
. PMID 23108550. doi:10.1098/rstb.2011.0388.
- ^ Donepezil for dementia due to Alzheimer's disease. The Cochrane Database of Systematic Reviews. 25 January 2006;(1):CD001190. doi:10.1002/14651858.CD001190.pub2. PMID 16437430.
- ^ 169.0 169.1 Birks JS, Grimley Evans J. Rivastigmine for Alzheimer's disease. The Cochrane Database of Systematic Reviews. April 2015, (4): CD001191. PMID 25858345. doi:10.1002/14651858.CD001191.pub3.
- ^ Cholinesterases and the pathology of Alzheimer disease. Alzheimer Disease and Associated Disorders. 1995;9 Suppl 2:23–28. doi:10.1097/00002093-199501002-00005. PMID 8534419.
- ^ The new cholinesterase inhibitors for Alzheimer's disease, part 2: illustrating their mechanisms of action. The Journal of Clinical Psychiatry. 2000;61(11):813–14. doi:10.4088/JCP.v61n1101. PMID 11105732.
- ^ 172.0 172.1 Cholinesterase inhibitors for Alzheimer's disease. The Cochrane Database of Systematic Reviews. 2006;(1):CD005593. doi:10.1002/14651858.CD005593. PMID 16437532.
- ^ 173.0 173.1 Birks, Jacqueline S.; Harvey, Richard J. Donepezil for dementia due to Alzheimer's disease. The Cochrane Database of Systematic Reviews. 2018, 6: CD001190. ISSN 1469-493X. PMID 29923184. doi:10.1002/14651858.CD001190.pub3.
- ^ Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials. PLoS Medicine. 2007;4(11):e338. doi:10.1371/journal.pmed.0040338. PMID 18044984.
- ^ al.], edited by Brian K. Alldredge ... [et. Applied therapeutics : the clinical use of drugs 10th. Baltimore: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2013: 2385. ISBN 978-1609137137.
- ^ 176.0 176.1 Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond. Nature Reviews. Drug Discovery. 2006;5(2):160–70. doi:10.1038/nrd1958. PMID 16424917.
- ^ Memantine. US National Library of Medicine (Medline). 4 January 2004 [3 February 2010]. (原始内容存档于22 February 2010).
- ^ McShane R, Areosa Sastre A, Minakaran N. Memantine for dementia. The Cochrane Database of Systematic Reviews. April 2006, (2): CD003154. PMID 16625572. doi:10.1002/14651858.CD003154.pub5.
- ^ Namenda prescribing information (PDF). Forest Pharmaceuticals. [19 February 2008]. (原始内容 (PDF)存档于27 February 2008). (primary source)
- ^ Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Annals of Internal Medicine. 2008;148(5):379–97. doi:10.7326/0003-4819-148-5-200803040-00009. PMID 18316756.
- ^ The Effectiveness of Atypical Antipsychotics for the Treatment of Aggression and Psychosis in Alzheimer's Disease. The Cochrane Database of Systematic Reviews. 2006;(1):CD003476. doi:10.1002/14651858.CD003476.pub2. PMID 16437455.
- ^ The Dementia Antipsychotic Withdrawal Trial (DART-AD): Long-term Follow-up of a Randomised Placebo-controlled Trial. Lancet Neurology. 9 January 2009;8(2):151–17. doi:10.1016/S1474-4422(08)70295-3. PMID 19138567. Lay summary.
- ^ Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, Christiaens T. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. The Cochrane Database of Systematic Reviews. March 2013, 3 (3): CD007726. PMID 23543555. doi:10.1002/14651858.CD007726.pub2.
- ^ Huperzine A for Alzheimer's disease. The Cochrane Database of Systematic Reviews. 2008;(2):CD005592. doi:10.1002/14651858.CD005592.pub2. PMID 18425924.
- ^ 185.0 185.1 185.2 185.3 185.4 185.5 185.6 American Psychiatric Association practice guideline for the treatment of patients with Alzheimer's disease and other dementias. The American Journal of Psychiatry. December 2007;164(12 Suppl):5–56. PMID 18340692.
- ^ Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study. Clinical Rehabilitation. 2005;19(8):861–69. doi:10.1191/0269215505cr911oa. PMID 16323385.
- ^ Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56(9):1154–66. doi:10.1212/WNL.56.9.1154. PMID 11342679.
- ^ Non-pharmacological interventions for wandering of people with dementia in the domestic setting. The Cochrane Database of Systematic Reviews. 2007;(1):CD005994. doi:10.1002/14651858.CD005994.pub2. PMID 17253573.
- ^ Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review. International Journal of Geriatric Psychiatry. 2007;22(1):9–22. doi:10.1002/gps.1643. PMID 17096455.
- ^ Abraha I, Rimland JM, Trotta FM, Dell'Aquila G, Cruz-Jentoft A, Petrovic M, Gudmundsson A, Soiza R, O'Mahony D, Guaita A, Cherubini A. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. The SENATOR-OnTop series. BMJ Open. 16 March 2017, 7 (3): e012759. PMC 5372076
 . PMID 28302633. doi:10.1136/bmjopen-2016-012759.
. PMID 28302633. doi:10.1136/bmjopen-2016-012759.
- ^ Chung JC, Lai CK, Chung PM, French HP. Snoezelen for dementia. The Cochrane Database of Systematic Reviews. 2002, (4): CD003152. PMID 12519587. doi:10.1002/14651858.CD003152.
- ^ Woods, B; O'Philbin, L; Farrell, EM; Spector, AE; Orrell, M. Reminiscence therapy for dementia.. The Cochrane Database of Systematic Reviews. 1 March 2018, 3: CD001120. PMID 29493789. doi:10.1002/14651858.CD001120.pub3.
- ^ Effectiveness of simulated presence therapy for individuals with dementia: a systematic review and meta-analysis. Aging & Mental Health. November 2008;12(6):779–85. doi:10.1080/13607860802380631. PMID 19023729.
- ^ Validation therapy for dementia. The Cochrane Database of Systematic Reviews. 2003;(3):CD001394. doi:10.1002/14651858.CD001394. PMID 12917907.
- ^ Snoezelen for dementia. The Cochrane Database of Systematic Reviews. 2002;(4):CD003152. doi:10.1002/14651858.CD003152. PMID 12519587. (up to date as of 2009)
- ^ Withdrawn: reality orientation for dementia. The Cochrane Database of Systematic Reviews. 2000;(3):CD001119. doi:10.1002/14651858.CD001119.pub2. PMID 17636652.
- ^ Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial. The British Journal of Psychiatry. 2003;183(3):248–54. doi:10.1192/bjp.183.3.248. PMID 12948999.
- ^ Chang, Chun-Hung; Lane, Hsien-Yuan; Lin, Chieh-Hsin. Brain Stimulation in Alzheimer's Disease. Frontiers in Psychiatry. 2018, 9. ISSN 1664-0640. PMC 5992378
 . PMID 29910746. doi:10.3389/fpsyt.2018.00201.
. PMID 29910746. doi:10.3389/fpsyt.2018.00201.
 本條目含有来自此处的文本,作者為Chun-Hung Chang, Hsien-Yuan Lane, and Chieh-Hsin Lin,以CC BY 4.0授權條款釋出。
本條目含有来自此处的文本,作者為Chun-Hung Chang, Hsien-Yuan Lane, and Chieh-Hsin Lin,以CC BY 4.0授權條款釋出。
- ^ A Randomized, Controlled Trial of a Home Environmental Intervention: Effect on Efficacy and Upset in Caregivers and on Daily Function of Persons with Dementia. The Gerontologist. 1 February 2001;41(1):4–14. doi:10.1093/geront/41.1.4. PMID 11220813.
- ^ Maintenance of Effects of the Home Environmental Skill-building Program for Family Caregivers and Individuals with Alzheimer's Disease and Related Disorders. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2005;60(3):368–74. doi:10.1093/gerona/60.3.368. PMID 15860476.
- ^ Treating Behavioral and Psychiatric Symptoms. Alzheimer's Association. 2006 [25 September 2006]. (原始内容存档于25 September 2006).
- ^ Visual Contrast Enhances Food and Liquid Intake in Advanced Alzheimer's Disease. Clinical Nutrition (Edinburgh, Scotland). 2004;23(4):533–38. doi:10.1016/j.clnu.2003.09.015. PMID 15297089.
- ^ Dudek, Susan G. Nutrition Essentials for Nursing Practice. Hagerstown, Maryland: Lippincott Williams & Wilkins. 2007: 360 [19 August 2008]. ISBN 0-7817-6651-6.
- ^ Analysis of Patients' Rights: Dementia and PEG Insertion. British Journal of Nursing. 2006;15(1):18–20. doi:10.12968/bjon.2006.15.1.20303. PMID 16415742.
- ^ Tube Feeding Patients with Dementia. Nutrition in Clinical Practice. 2006;21(2):142–46. doi:10.1177/0115426506021002142. PMID 16556924.
- ^ Predictors of Mortality in Patients with Alzheimer's Disease Living in Nursing Homes. Journal of Neurology, Neurosurgery, and Psychiatry. 1999;67(1):59–65. doi:10.1136/jnnp.67.1.59. PMID 10369823.
- ^ Medical issues:
- Palliative Care for Persons with Dementia. Home Healthcare Nurse. 2003;21(1):53–60; quiz 61. doi:10.1097/00004045-200301000-00012. PMID 12544465.
- Alzheimer's Disease: Psychopathology, Medical Management and Dental Implications. Journal of the American Dental Association. 2006;137(9):1240–51. PMID 16946428.
- Practical Guidelines for the Diagnosis and Management of Weight Loss in Alzheimer's Disease: A Consensus from Appropriateness Ratings of a Large Expert Panel. The Journal of Nutrition, Health & Aging. 2007;11(1):33–37. PMID 17315078.
- Training Caregivers to Change the Sleep Hygiene Practices of Patients with Dementia: The NITE-AD Project. Journal of the American Geriatrics Society. 2003;51(10):1455–60. doi:10.1046/j.1532-5415.2003.51466.x. PMID 14511168.
- Higher Respiratory Infection Rates on an Alzheimer's Special Care Unit and successful intervention. Journal of the American Geriatrics Society. 1995;43(12):1341–44. doi:10.1111/j.1532-5415.1995.tb06611.x. PMID 7490383.
- ^ Palliative Excellence in Alzheimer Care Efforts (PEACE): A Program Description. Journal of Palliative Medicine. 2003;6(2):315–20. doi:10.1089/109662103764978641. PMID 12854952.
- ^ 209.0 209.1 Zanetti O, Solerte SB, Cantoni F. Life expectancy in Alzheimer's disease (AD). Archives of Gerontology and Geriatrics. 2009,. 49 Suppl 1: 237–43. PMID 19836639. doi:10.1016/j.archger.2009.09.035.
- ^ 210.0 210.1 Long-Term Survival and Predictors of Mortality in Alzheimer's Disease and Multi-Infarct Dementia. Acta Neurologica Scandinavica. 1995;91(3):159–64. doi:10.1111/j.1600-0404.1995.tb00426.x. PMID 7793228.
- ^ Predictors of Mortality in Patients Diagnosed with Probable Alzheimer's Disease. Neurology. 1996;47(2):433–39. doi:10.1212/wnl.47.2.433. PMID 8757016.
- ^ Survival after Initial Diagnosis of Alzheimer Disease. Annals of Internal Medicine. 2004;140(7):501–09. doi:10.7326/0003-4819-140-7-200404060-00008. PMID 15068977.
- ^ Predictors of Survival with Alzheimer's Disease: A Community-based Study. Psychological Medicine. 1995;25(1):171–77. doi:10.1017/S0033291700028191. PMID 7792352.
- ^ Functional Transitions and Active Life Expectancy Associated with Alzheimer Disease. Archives of Neurology. 2003;60(2):253–59. doi:10.1001/archneur.60.2.253. PMID 12580712.
- ^ 215.0 215.1 Alzheimer Disease and Mortality: A 15-year Epidemiological Study. Archives of Neurology. 2005;62(5):779–84. doi:10.1001/archneur.62.5.779. PMID 15883266.
- ^ 216.0 216.1 216.2 Incidence and subtypes of dementia in three elderly populations of central Spain. Journal of the Neurological Sciences. 2008;264(1–2):63–72. doi:10.1016/j.jns.2007.07.021. PMID 17727890.
- ^ 217.0 217.1 217.2 Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study. Journal of the American Geriatrics Society. 2002;50(1):41–48. doi:10.1046/j.1532-5415.2002.50006.x. PMID 12028245.
- ^ Gender Differences in the Incidence of AD and Vascular Dementia: The EURODEM Studies. EURODEM Incidence Research Group. Neurology. 1999;53(9):1992–97. doi:10.1212/wnl.53.9.1992. PMID 10599770.
- ^ Tejada-Vera B. (2013). Mortality from Alzheimer's Disease in the United States: Data for 2000 and 2010. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- ^ 2000 U.S. estimates:
- Alzheimer Disease in the US population: Prevalence Estimates Using the 2000 census. Archives of Neurology. 2003;60(8):1119–22. doi:10.1001/archneur.60.8.1119. PMID 12925369.
- Profiles of General Demographic Characteristics, 2000 Census of Population and Housing, United States (PDF). U.S. Census Bureau. 2001 [27 August 2008]. (原始内容存档 (PDF)于19 August 2008).
- ^ 221.0 221.1 Global Prevalence of Dementia: A Delphi Consensus Study. Lancet. 2005;366(9503):2112–17. doi:10.1016/S0140-6736(05)67889-0. PMID 16360788.
- ^ World Health Organization. Neurological Disorders: Public Health Challenges. Switzerland: World Health Organization. 2006: 204–07. ISBN 978-92-4-156336-9. (原始内容存档于10 February 2010).
- ^ 2006 prevalence estimate:
- Forecasting the global burden of Alzheimer's disease. Alzheimer's & Dementia. 2007;3(3):186–91. doi:10.1016/j.jalz.2007.04.381. PMID 19595937.
- World population prospects: the 2006 revision, highlights [PDF]. 2007.
- ^ Auguste D.:
- Alzheimer Alois. Über eine eigenartige Erkrankung der Hirnrinde [About a peculiar disease of the cerebral cortex]. Allgemeine Zeitschrift für Psychiatrie und Psychisch-Gerichtlich Medizin. 1907;64(1–2):146–48. (德文).
- About a Peculiar Disease of the Cerebral Cortex. Alzheimer Disease and Associated Disorders. 1987;1(1):3–8. PMID 3331112.
- Maurer Ulrike; Maurer Konrad. Alzheimer: The Life of a Physician and the Career of a Disease. New York: Columbia University Press. 2003: 270. ISBN 0-231-11896-1.
- ^ Berrios G E. Alzheimer's Disease: A Conceptual History. Int. J. Ger. Psychiatry. 1990;5(6):355–65. doi:10.1002/gps.930050603.
- ^ Kraepelin Emil. Clinical Psychiatry: A Textbook For Students And Physicians (Reprint). 由Diefendorf A. Ross翻译. Kessinger Publishing. 17 January 2007: 568. ISBN 1-4325-0833-4.
- ^ Katzman Robert; Terry Robert D; Bick Katherine L (编). Alzheimer's Disease: Senile Dementia and Related Disorders. New York: Raven Press. 1978: 595. ISBN 0-89004-225-X.
- ^ Boller, François; Forbes, Margaret M. History of dementia and dementia in history: An overview. Journal of the Neurological Sciences. 1998-06, 158 (2): 125–133. ISSN 0022-510X. doi:10.1016/s0022-510x(98)00128-2.
- ^ Schoenberg, Bruce S.; Rocca, Walter A.; Amaducci, Luigi A. Origin of the distinction between Alzheimer's disease and senile dementia: How history can clarify nosology. Neurology. 1986-11-01, 36 (11): 1497–1497. ISSN 1526-632X. PMID 3531918. doi:10.1212/WNL.36.11.1497.
- ^ Economic Impact of Dementia in Developing Countries: An Evaluation of Costs of Alzheimer-type Dementia in Argentina. International Psychogeriatrics. 2007;19(4):705–18. doi:10.1017/S1041610206003784. PMID 16870037.
- ^ The Economic Costs of Dementia in Korea, 2002. International Journal of Geriatric Psychiatry. 2006;21(8):722–28. doi:10.1002/gps.1552. PMID 16858741.
- ^ An Estimate of the Worldwide Prevalence and Direct Costs of Dementia in 2003. Dementia and Geriatric Cognitive Disorders. 2006;21(3):175–81. doi:10.1159/000090733. PMID 16401889.
- ^ 233.0 233.1 233.2 Informal Costs of Dementia Care: Estimates from the National Longitudinal Caregiver Study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2001;56(4):S219–28. doi:10.1093/geronb/56.4.S219. PMID 11445614.
- ^ Determinants of Costs of Care for Patients with Alzheimer's Disease. International Journal of Geriatric Psychiatry. 2006;21(5):449–59. doi:10.1002/gps.1489. PMID 16676288.
- ^ 235.0 235.1 The MetLife study of Alzheimer's disease: The caregiving experience (PDF). MetLife Mature Market Institute. August 2006 [5 February 2011]. (原始内容 (PDF)存档于8 January 2011).
- ^ EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden. International Journal of Geriatric Psychiatry. 1999;14(8):651–61. doi:10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B. PMID 10489656.
- ^ EUROCARE: A Cross-National Study of Co-resident Spouse Carers for People with Alzheimer's Disease: II—A Qualitative Analysis of the Experience of Caregiving. International Journal of Geriatric Psychiatry. 1999;14(8):662–67. doi:10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4. PMID 10489657.
- ^ 238.0 238.1 Economic Considerations in the Management of Alzheimer's Disease. Clinical Interventions in Aging. 2006;1(2):143–54. doi:10.2147/ciia.2006.1.2.143. PMID 18044111.
- ^ Early Community-based Service Utilization and Its Effects on Institutionalization in Dementia Caregiving. The Gerontologist. 2005;45(2):177–85. doi:10.1093/geront/45.2.177. PMID 15799982.
- ^ The Dementias. Lancet. 2002;360(9347):1759–66. doi:10.1016/S0140-6736(02)11667-9. PMID 12480441.
- ^ Psychosocial Effects on Carers of Living with Persons with Dementia. The Australian and New Zealand Journal of Psychiatry. 1990;24(3):351–61. doi:10.3109/00048679009077702. PMID 2241719.
- ^ Determinants of Carer Stress in Alzheimer's Disease. International Journal of Geriatric Psychiatry. 1998;13(4):248–56. doi:10.1002/(SICI)1099-1166(199804)13:4<248::AID-GPS770>3.0.CO;2-0. PMID 9646153.
- ^ A Systematic Review of the Effectiveness of Psychosocial Interventions for Carers of People with Dementia. Aging & Mental Health. 2001;5(2):107–19. doi:10.1080/13607860120038302. PMID 11511058.
- ^ Bayley John. Iris: A Memoir of Iris Murdoch. London: Abacus. 2000. ISBN 978-0-349-11215-2. OCLC 41960006.
- ^ Sparks Nicholas. The notebook. Thorndike, Maine: Thorndike Press. 1996: 268. ISBN 0-7862-0821-X.
- ^ Thanmathra. Webindia123.com. [24 January 2008]. (原始内容存档于6 November 2007).
- ^ Ogiwara Hiroshi. Ashita no Kioku. Tōkyō: Kōbunsha. 2004. ISBN 978-4-334-92446-1. OCLC 57352130 (日语).
- ^ Munro Alice. Hateship, Friendship, Courtship, Loveship, Marriage: Stories. New York: A.A. Knopf. 2001. ISBN 978-0-375-41300-1. OCLC 46929223.
- ^ Malcolm and Barbara: A love story. Dfgdocs. [24 January 2008]. (原始内容存档于24 May 2008).
- ^ Malcolm and Barbara: A love story. BBC Cambridgeshire. [2 March 2008]. (原始内容存档于10 November 2012).
- ^ Plunkett J. Alzheimer's film-maker to face ITV lawyers. London: Guardian Media. 7 August 2007 [24 January 2008]. (原始内容存档于15 January 2008).
延伸閱讀
| 關於阿茲海默症 的圖書館資源 |
- Alzheimer's Disease: Unraveling the Mystery. US Department of Health and Human Services, National Institute on Aging, NIH. 2008. (原始内容存档于8 January 2012).
- Can Alzheimer's Disease Be Prevented? (PDF). US Department of Health and Human Services, National Institute on Aging, NIH. 2009. (原始内容 (PDF)存档于2 May 2013).
- Caring for a Person with Alzheimer's Disease: Your Easy-to-Use Guide from the National Institute on Aging. US Department of Health and Human Services, National Institute on Aging, NIH. 2009. (原始内容存档于8 January 2012).
- Russell D, Barston S, White M. Alzheimer's Behavior Management: Learn to Manage Common Behavior Problems. helpguide.org. 19 December 2007 [29 February 2008]. (原始内容存档于23 February 2008).
- Greater cognitive deterioration in women than men with Alzheimer's disease: a meta analysis. Journal of Clinical and Experimental Neuropsychology. 2012;34(9):989–98. doi:10.1080/13803395.2012.712676. PMID 22913619.
外部連結
| 维基共享资源上的相关多媒体资源:阿茲海默症 |
| |||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||
|



