阻生智齿:修订间差异
←建立内容为“{{Infobox medical condition | name = 阻生智齿 | image = File:3D CT impacted wisdom tooth.Gif | alt = 阻生智…”的新页面 |
(没有差异)
|
2017年5月27日 (六) 08:43的版本
| 阻生智齿 | |
|---|---|
 | |
| CT三维成像显示未拔除的阻生智齿相邻于下牙槽神经 | |
| 类型 | 阻生牙[*] |
| 分类和外部资源 | |
| 醫學專科 | 牙醫學 |
| ICD-10 | K01.1 |
| ICD-9-CM | 520.6 |
| OMIM | 189490 |
| DiseasesDB | 32003 |
| MedlinePlus | 001057 |
| MeSH | C07.793.846 |
阻生智齿 ( 阻生第三臼齿)是智齿受其他牙齿影响而未能完全牙萌出的阻生齿。阻生智齿可能会造成冠周炎或损坏相邻牙。通常考虑第三臼齿的萌出角度、牙根发育阶段、阻生深度、萌出可用空间以及第三臼齿的尺寸。[1]
智齿变为阻生的原因是牙尺寸与下颌尺寸不匹配。阻生智齿的分类按照阻生方向、相比较于邻牙咬合面的深度、覆盖在牙冠上的牙龈或牙槽骨的量。[2][3]也可按是否有临床症状分类。[4]通常在青春期后期邻牙出现阻生症状时才发现智齿问题。可用口腔全景发射线检查筛选。
阻生智齿感染可用抗生素、牙結石清除術(洗牙)、龈切除术做初步治疗。但通常不会奏效并发生其它并发症。最常用办法是拔除智齿。其风险与拔牙的难度成正比。如果有高风险的下牙槽神经,可能仅拔除智齿的牙冠,故意保留智齿的牙根,这称为智齿冠切术。其风险是残留牙根的顽固性感染。
分类
牙齿可分类为发育牙、萌出牙、埋伏牙(不受其它牙影响但是无法萌出)、阻生牙。
智齿发育于14岁至25岁,16岁时已经有50%的牙根形成。25岁时有95%的人智齿全部萌出。但是智齿的移动在25岁以后仍会继续。[5]:140
临床统计结果,11%的阻生智齿发病并有临床症状,0.6%有症状但未发病,51%无症状但发病,37%无症状且未发病。[4]
阻生智齿按照其方向(最常见的是向前倾斜,称“近中”,阻生深度、是否感染发炎来描述。[5]:143–144 其中年龄是最相关于拔除智齿的难度与复杂度[6]而不是阻生方向.[7]
征兆与症状

Impacted wisdom teeth without a communication to the mouth, that have no pathology associated with the tooth and have not caused tooth resorption on the blocking tooth rarely have symptoms. In fact, only 12% of impacted wisdom teeth are associated with pathology.[8]
When wisdom teeth communicate with the mouth, the most common symptom is localized pain, swelling and bleeding of the tissue overlying the tooth. This tissue is called the operculum and the disorder called pericoronitis which means inflammation around the crown of the tooth.[5]:141 Low grade chronic periodontitis commonly occurs on either the wisdom tooth or the second molar, causing less obvious symptoms such as bad breath and bleeding from the gums. The teeth can also remain asymptomatic (pain free), even with disease.[4] As the teeth near the mouth during normal development, people sometimes report mild pressure of other symptoms similar to teething.
The term asymptomatic means that the person has no symptoms. The term asymptomatic should not be equated with absence of disease. Most diseases have no symptoms early in the disease process. A pain free or asymptomatic tooth can still be infected for many years before pain symptoms develop.[4]
病因
Wisdom teeth become impacted when there is not enough room in the jaws to allow for all of the teeth to erupt into the mouth. Because the wisdom teeth are the last to erupt, due to insufficient room in the jaws to accommodate more teeth, the wisdom teeth become stuck in the jaws, i.e., impacted. There is a genetic predisposition to tooth impaction. Genetics plays an important, albeit unpredictable role in dictating jaw and tooth size and tooth eruption potential of the teeth. Some also believe that there is an evolutionary decrease in jaw size due to softer modern diets that are more refined and less coarse than our ancestors'.[3]
Pathophysiology


For partially impacted teeth in those over 20 year of age, the most common pathology seen, and the most common reason for wisdom teeth removal, is pericoronitis or infection of the gum tissue over the impacted tooth. The bacteria associated with infections include Peptostreptococcus, Fusobacterium, and Bacteroides bacteria. The next most common pathology seen is cavities or tooth decay. Fifteen percent of people with retained wisdom teeth exposed to the mouth have cavities on the wisdom tooth or adjacent second molar due to a wisdom tooth. The rate of cavities on the back of the second molar has been reported anywhere from 1% to 19% with the wide variation attributed to increased age.[9]
In five percent of cases, advanced periodontitis or gum inflammation between the second and third molars precipitates the removal of wisdom teeth.[5]:141[3] Among patients with retained, asymptomatic wisdom teeth, roughly 25% have gum infections (periodontal disease).[10]:ch13 Teeth with periodontal pockets of greater than 5mm have tooth loss rates that start at 10 teeth lost per 1000 teeth per year at 5mm to a rate of 70 teeth lost per year per 1000 teeth at 11mm.[11]:57 The risk of periodontal disease and caries on third molars increases with age with a small minority (less than 2%) of adults age 65 years or older maintaining the teeth without caries or periodontal disease and 13% maintaining unimpacted wisdom teeth without caries or periodontal disease.[12] Periodontal probing depths increase over time to greater than 4 mm in a significant proportion of young adults with retained impacted wisdom teeth which is associated with increases in serum inflammatory markers such as interleukin-6, soluble intracellular adhesion molecule-1 and C-reactive protein.[13]
Crowding of the front teeth is not believed to be caused by the eruption of wisdom teeth although this is a reason many dental clinicians use to justify wisdom teeth extraction.[5]:141,[14]
诊断

The diagnosis of impaction can be made clinically if enough of the wisdom tooth is visible to determine its angulation, depth, and if the patient is old enough that further eruption or uprighting is unlikely. Wisdom teeth continue to move into adulthood (20–30 years old) due to eruption and then continue some later movement owing to periodontal disease.[15]
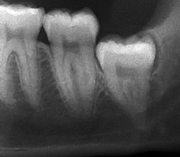
If the tooth cannot be assessed with clinical exam alone, the diagnosis is made using either a panoramic radiograph or cone-beam CT. Where unerupted wisdom teeth still have eruption potential several predictors are used to determine the chance of the teeth becoming impacted. The ratio of space between the tooth crown length and the amount of space available, the angle of the teeth compared to the other teeth are the two most commonly used predictors, with the space ratio being the most accurate. Despite the capacity for movement into early adulthood, the likelihood that the tooth will become impacted can be predicted when the ratio of space available to the length of the crown of the tooth is under 1.[5]:141
筛查

There is no standard to screen for wisdom teeth. It has been suggested, absent evidence to support routinely retaining or removing wisdom teeth, that evaluation with panoramic radiograph, starting between the ages of 16 and 25 be completed every 3 years. Once there is the possibility of the teeth developing disease, then a discussion about the operative risks versus long-term risk of retention with an oral and maxillofacial surgeon or other clinician trained to evaluate wisdom teeth is recommended. These recommendations are based on expert opinion level evidence.[16] Screening at a younger age may be required if the second molars (the "12-year molars") fail to erupt as ectopic positioning of the wisdom teeth can prevent their eruption. Radiographs can be avoided if the majority of the tooth is visible in the mouth.
治疗
Wisdom teeth that are fully erupted and in normal function need no special attention and should be treated just like any other tooth. It is more challenging, however to make treatment decisions with asymptomatic, disease-free wisdom teeth, i.e. wisdom teeth that have no communication to the mouth and no evidence of clinical or radiographic disease (see Treatment controversy below).[17]
局部治疗

Where there is an operculum of gingiva overlying the tooth that has become infected it can be treated with local cleaning, an antiseptic rinse of the area and antibiotics if severe. Definitive treatment can be excision of the tissue, however, recurrence of these infections is high. Pericoronitis, while a small area of tissue, should be viewed with caution, because it lies near the anatomic planes of the neck and can progress to life-threatening neck infections.[11]:440–441
拔除智齿
Wisdom teeth removal (extraction) is the most common treatment for impacted wisdom teeth. In the US, 10 million wisdom teeth are removed annually.[18] The general agreement for wisdom tooth removal is the presence of disease or symptoms related to that tooth.
The procedure, depending on the depth of the impaction and angle of the tooth, is to create an incision in the mucosa of the mouth, remove bone of the mandible or maxilla adjacent the tooth, section the tooth and extract it in pieces. This can be completed under local anaesthetic, sedation or general anaesthetic.
恢复、风险与复杂性
Most patients will experience pain and swelling (worst on the first post-operative day) then return to work after 2 to 3 days with the rate of discomfort decreased to about 25% by post-operative day 7 unless affected by dry socket: a disorder of wound healing that prolongs post-operative pain. It can be 4 to 6 weeks before patients are fully recovered with a full range of jaw movements.[19] A Cochrane investigation found that the use of antibiotics either just before or just after surgery reduced the risk of infection, pain and dry socket after wisdom teeth are removed by oral surgeons, but that using antibiotics also causes more side effects for these patients. Twelve patients needed to receive antibiotics to prevent 1 infection and for every 21 people who received antibiotics, an adverse event was likely. The conclusion of the review was that antibiotics given to healthy people to prevent infections may cause more harm than benefit to both the individual patients and the population as a whole.[20] Another Cochrane Investigation has found post-operative pain is effectively managed with either ibuprofen, or ibuprofen in combination with acetaminophen.[21]
Long-term complications can include periodontal complications such as bone loss on the second molar following wisdom teeth removal. Bone loss as a complication after wisdom teeth removal is uncommon in the young but present in 43% of those of 25 years of age or older. Initiation or worsening of temporomandibular joint problems is uncommon and unpredictable. Injury to the inferior alveolar nerve resulting in numbness or partial numbness of the lower lip and chin has reported rates that vary widely from 0.04% to 5%. The largest study is from a survey of 535 oral and maxillofacial surgeons in California, where a rate of 1:2,500 was reported. The large variation in report rates is attributed to variations in technique, the patient pool and surgeon experience. Other complications that are uncommon have been reported including persistent sinus communication, damage to adjacent teeth, lingual nerve injury, displaced teeth, osteomyelitis and jaw fracture.[19] Alveolar osteitis, post-operative infection, excessive bleeding may also be expected.[22]
治疗难题
Many impacted wisdom teeth are extracted prior to the age of 25, when full eruption can be reasonably expected and before symptoms or disease have begun. This has led to a treatment controversy generally referred to as the extraction of asymptomatic, disease-free wisdom teeth.
In 2000, the first National Institute of Clinical Excellence (NICE) of the United Kingdom set guidelines[23] to limit the removal of asymptomatic disease-free third molars citing the number of pathology free impacted teeth being removed and the potential cost savings to the public purse. Advocates of the policy point out that the impacted wisdom teeth can be monitored and avoidance of surgery also means avoidance of the recovery, risks, complications and costs associated with it. Following implementation of the NICE guidelines the UK saw a decrease in the number of impacted third molar operations between 2000 and 2006 and a rise in the average age at extraction from 25 to 31 years.[9] American Public Health Association has adopted a similar policy against removal of third molars before any problems have occurred.[24]
Those who argue against a blanket moratorium on the extraction of asymptomatic, disease-free wisdom teeth point out that wisdom teeth commonly develop periodontal disease or cavities which may eventually damage the second molars and that there are costs associated with monitoring wisdom teeth. They also point to the fact that there is an increase in the rate of post-operative periodontal disease on the second molar,[4] difficulty of surgery and post-operative recovery time with age.[6] The UK has also seen an increase in the rate of dental caries on the lower second molars increasing from 4–5% prior to the NICE guideline to 19% after its adoption.[9]
Although most studies arrive at the conclusion of negative long-term outcomes e.g. increased pocketing & attachment loss after surgery, it is clear that early removal (before 25 years old), good post-operative hygiene & plaque control, and lack of pre-existing periodontal pathology before surgery are the most crucial factors that minimise the probability of adverse post-surgical outcomes.[25]

The Cochrane review of surgical removal versus retention of asymptomatic disease-free impacted wisdom teeth suggests that the presence of asymptomatic impacted wisdom teeth may be associated with increased risk of periodontal disease affecting adjacent 2nd molar (measured by distal probing depth > 4 mm on that tooth) in the long term, however it is of very low quality evidence and high risk of bias. Another study which was at high risk of bias, found no evidence to suggest that removal of asymptomatic disease-free impacted wisdom teeth has an effect on crowding in the dental arch. There is also insufficient evidence to highlight a difference in risk of decay with or without impacted wisdom tooth.[22]
One trial in adolescents who had orthodontic treatment comparing the removal of impacted mandibular wisdom teeth with retention was identified. It only examined the effect on late lower incisor crowding and was rated 'highly biased' by the authors. The authors concluded that there is not enough evidence to support either the routine removal or retention of asymptomatic impacted wisdom teeth.[14] Another randomised controlled trial done in the UK has suggested that it is not reasonable to remove asymptomatic disease-free impacted wisdom tooth merely to prevent incisor crowding as there is not strong enough evidence to show this association.[26]
Due to the lack of sufficient evidence to determine whether such teeth should be removed or not, the patient's preference and values should be taken into account with clinical expertise exercised and careful consideration of risks & benefits to determine treatment.[25] If it is decided to retain asymptomatic disease-free impacted wisdom teeth, clinical assessment at regular intervals is advisable to prevent undesirable outcomes (pericoronitis, root resorption, cyst formation, tumour formation, inflammation/infection).[22]
智齿冠切术

Coronectomy is a procedure used when the surgeon believes that there is a high risk of inferior alveolar nerve injury. After making the incision in the mucosa and removing bone adjacent the tooth, the crown is cut and removed with no attempt at removing the roots. It is indicated when there is no disease of the dental pulp or infection around the crown of the tooth and there is a high risk of inferior alveolar nerve injury.
Coronectomy, while lessening the immediate risk to the inferior alveolar nerve function has its own complication rates and can result in repeated surgeries. Between 2.3% and 38.3% of roots loosen during the procedure and need to be removed and up to 4.9% of cases require reoperation due to persistent pain, root exposure or persistent infection. The roots have also been reported to migrate in 13.2% to 85.9% of cases.[27]
预后
The prognosis for impacted wisdom teeth depends on the depth of the impaction. When they lack a communication to the mouth, the main risk is the chance of cyst or neoplasm formation which is relatively uncommon.
Once communicating with the mouth, the onset of disease or symptoms cannot be predicted but the chance of it does increase with age. Less than 2% of wisdom teeth are free of either periodontal disease or caries by age 65.[12] Further, several studies have found that between 30% – 60% of people with previously asymptomatic impacted wisdom teeth will have them extracted due to symptoms or disease, 4–12 years after initial examination.[17]
Extraction of the wisdom teeth removes the disease on the wisdom tooth itself and also appears to improve the periodontal status of the second molar, although this benefit diminishes beyond the age of 25.[12]
流行病学
Few studies have looked at the percentage of the time wisdom teeth are present or the rate of wisdom teeth eruption. The lack of up to five teeth (excluding third molars, i.e. wisdom teeth) is termed hypodontia. Missing third molars occur in 9-30% of studied populations.
One large scale study on a group of young adults in New Zealand showed 95.6% had at least 1 wisdom tooth with an eruption rate of 15% in the maxilla and 20% in the mandible.[28] Another study on 5000 army recruits found 10,767 impacted wisdom teeth.[29]:246 The frequency of impacted lower third molars has been found to be 72%[17] and the frequency of retained impacted wisdom teeth that are free of disease and symptoms is estimated at 11.6% to 29% which drops with age.[28]
The incidence of wisdom tooth removal was estimated to be 4 per 1000 person years in England and Wales prior to the 2000 NICE guidelines.[17]
历史

Wisdom teeth have been described in the ancient texts of Plato and Hippocrates. "Teeth of wisdom" being from the Latin, dentes sapientiæ, which in turn is derived from the Hippocratic term, sophronisteres, from the Greek sophron, meaning prudent.[30]
Charles Darwin believed the wisdom teeth to be in decline with evolution which his contemporary, Paolo Mantegazza, later proved to be false when he discovered Darwin was not opening the jawbones of specimens to find the impacted tooth stuck in the jaw.[31]
In the late 19th and early 20th centuries, the collision of sterile technique, anaesthesia and radiology made routine surgery on the wisdom teeth possible. John Tomes's 1873 text A System of Dental Surgery describes techniques for removal of "third molars, or dentes sapientiæ" including descriptions of inferior alveolar nerve injury, jaw fracture and pupil dilation after opium is placed in the socket.[32] Other texts from about this time speculate on their deevolution, that they are prone to decay and discussion on whether or not they lead to crowding of the other teeth.[33]
参考文献
- ^ Third Molar Surgery: A Review Of Current Controversies In Prophylactic Removal Of Wisdom Teeth - Oral Health Group. Oral Health Group. [2016-11-21] (美国英语).
- ^ Hupp, James R., et. al. Contemporary Maxillofacial Surgery, 6E, Elsevier-Mosby, 2014. ISBN 978-0-323-09177-0
- ^ 3.0 3.1 3.2 Juodzbalys G, Daugela P. Mandibular Third Molar Impaction: Review of Literature and a Proposal of a Classification (review). J Oral Maxillofac Res. Apr–Jun 2013, 4 (2): e1. PMC 3886113
 . PMID 24422029. doi:10.5037/jomr.2013.4201.
. PMID 24422029. doi:10.5037/jomr.2013.4201.
- ^ 4.0 4.1 4.2 4.3 4.4 Dodson TB. The management of the asymptomatic, disease-free wisdom tooth: removal versus retention. (review). Atlas Oral Maxillofac Surg Clin North Am. Sep 2012, 20 (2): 169–76. PMID 23021394. doi:10.1016/j.cxom.2012.06.005.
- ^ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Peterson, Larry J.; Miloro, Michael. Peterson's Principles of Oral and Maxillofacial Surgery 2nd. PMPH-USA. 2004. ISBN 978-1-55009-234-9.
- ^ 6.0 6.1 Pogrel MA. What Is the Effect of Timing of Removal on the Incidence and Severity of Complications (review). J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 37–40.
- ^ Bali A, Bali D, Sharma A, Verma G. Is Pederson Index a True Predictive Difficulty Index for Impacted Mandibular Third Molar Surgery? A Meta-analysis.. J Oral Maxillofac Surg. Sep 2013, 12 (3): 359–364. doi:10.1007/s12663-012-0435-x.
- ^ Friedman, JW. The prophylactic extraction of third molars: a public health hazard.. American Journal of Public Health. September 2007, 97 (9): 1554–9. PMC 1963310
 . PMID 17666691. doi:10.2105/ajph.2006.100271.
. PMID 17666691. doi:10.2105/ajph.2006.100271.
- ^ 9.0 9.1 9.2 Renton T, Al-Haboubi M, Pau A, Shepherd J, Gallagher JE. What Has Been the United Kingdom's Experience with Retention of Third Molars?. J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 48–57.
- ^ Bell RB, Khan HA. Current Therapy in Oral and Maxillofacial Surgery. Elsevier Saunders. 2012. ISBN 978-1-4160-2527-6.
- ^ 11.0 11.1 Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. Elsevier Saunders. 2012. ISBN 978-1-4377-0416-7.
- ^ 12.0 12.1 12.2 Marciani RD. Is there pathology associated with asymptomatic third molars (review). J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 15–19. doi:10.1016/j.joms.2012.04.025.
- ^ Offenbacher S, Beck JD, Moss KL, et al. What Are the Local and Systemic Implications of Third Molar Retention. J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 58–65.
- ^ 14.0 14.1 Mettes TD. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. (Cochrane Invest). Cochrane Database Syst Rev. Jun 2012, 13 (6): CD003879. PMID 22696337. doi:10.1002/14651858.CD003879.pub3.
- ^ Phillips C, White RP. How Predictable Is the Position of Third (review). J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 11–14.
- ^ Dodson TB. Surveillance as a Management Strategy for Retained Third Molars: Is it Desirable?. J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 20–24. PMID 22916696. doi:10.1016/j.joms.2012.04.026.
- ^ 17.0 17.1 17.2 17.3 Dodson TB, Susarta SM. Impacted wisdom teeth (systematic review). Clin Evid (Online). Apr 2010, 2010 (1302). PMC 2907590
 . PMID 21729337.
. PMID 21729337.
- ^ Moisse, Katie. Parents Sue After Teen Dies During Wisdom Tooth Surgery. ABC News. 15 December 2011 [27 January 2016].
- ^ 19.0 19.1 Pogrel MA. What are the Risks of Operative Intervention (review). J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 33–36.
- ^ Lodi G, Figini L, et al. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev. Nov 2012, 11: CD003811. PMID 23152221. doi:10.1002/14651858.CD003811.pub2.
- ^ Bailey E, Worthington HV, et al. Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database Syst Rev. Dec 2013, 12: 12:CD004624. doi:10.1002/14651858.CD004624.pub2.
- ^ 22.0 22.1 22.2 Ghaeminia, Hossein; Perry, John; Nienhuijs, Marloes EL; Toedtling, Verena; Tummers, Marcia; Hoppenreijs, Theo JM; Van der Sanden, Wil JM; Mettes, Theodorus G. Cochrane Database of Systematic Reviews. John Wiley & Sons. 2016-08-31. ISSN 1465-1858. doi:10.1002/14651858.cd003879.pub4 (英语).
- ^ TA1 Wisdom teeth – removal: guidance. London, United Kingdom: National Institute for Clinical Excellence (UK). 2000.
- ^ Opposition to Prophylactic Removal of Third Molars (Wisdom Teeth). Policy Statement Database. American Public Health Association. 2008-10-28 [2016-03-09].
- ^ 25.0 25.1 Dodson, Thomas B. Current Therapy in Oral and Maxillofacial Surgery. : 122–126.
- ^ Song, F.; O'Meara, S.; Wilson, P.; Golder, S.; Kleijnen, J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technology Assessment (Winchester, England). 2000-01-01, 4 (15): 1–55. ISSN 1366-5278. PMID 10932022.
- ^ Ghaeminia H. Coronectomy may be a way of managing impacted third molars (systematic review). Evid Based Dent. 2013, 14 (2): 57–8. PMID 23792405. doi:10.1038/sj.ebd.6400939.
- ^ 28.0 28.1 Dodson TB. How Many Patients Have Third Molars and How Many Have One or More Asymptomatic, Disease-Free Third Molars?. J Oral Maxillofac Surg. 2012, 70 (Suppl 1): 4–7. doi:10.1016/j.joms.2012.04.038.
- ^ Fonseca RJ. Oral and Maxillofacial Surgery Volume 1. Philadelphia, PA: Saunders. 2000. ISBN 0-7216-9632-5.
- ^ Mitchell E, Barclay J. A Series of Engravings: Representing the Bones of the Human Skeleton; with the Skeletons of Some of the Lower Animals. High Street, London, UK: Oliver & Boyd. 1819.
- ^ Mantegazza, P. Concerning the Atrophy and Absence of Wisdom Teeth. Stevenson, RK (编). Anthropology Society of Paris Meeting of June 20, 1878. Paris, France: Anthropology Society of Paris. June 1878 [4 February 2014].
- ^ Tomes, J.; Tomes, C. S. A System of Dental Surgery. London, UK: J&A Churchill. 1873.
- ^ Gant, F. Science and Practice of Surgery ; Including Special Chapters by Different Authors, Volume 2. Philadelphia, USA: Lindsay & Blakiston. 1878: 308.