User:Dr3939/沙盒:修订间差异
←清空全部内容 标签:清空 2017版源代码编辑 |
无编辑摘要 标签:2017版源代码编辑 |
||
| 第1行: | 第1行: | ||
{{Infobox medical condition (new) |
|||
| name = Female infertility |
|||
| synonyms = |
|||
| image = Age and female fertility.png |
|||
| caption = Cumulative percentage and average age for women reaching [[subfertility]], [[Infertility|sterility]], [[irregular menstruation]] and [[menopause]].<ref>{{cite journal|last1=te Velde|first1=E. R.|title=The variability of female reproductive ageing|journal=Human Reproduction Update|volume=8|issue=2|year=2002|pages=141–154|issn=1355-4786|doi=10.1093/humupd/8.2.141|pmid=12099629}}</ref> |
|||
| pronounce = |
|||
| field = [[Gynecology]] |
|||
| symptoms = |
|||
| complications = |
|||
| onset = |
|||
| duration = |
|||
| types = |
|||
| causes = |
|||
| risks = |
|||
| diagnosis = |
|||
| differential = |
|||
| prevention = |
|||
| treatment = |
|||
| medication = |
|||
| prognosis = |
|||
| frequency = |
|||
| deaths = |
|||
}} |
|||
'''Female infertility''' refers to [[infertility]] in women. It affects an estimated 48 million women,<ref name="Mascarenhas, M.N. 2012" /> with the highest prevalence of infertility affecting people in South Asia, Sub-Saharan Africa, North Africa/Middle East, and Central/Eastern Europe and Central Asia.<ref name="Mascarenhas, M.N. 2012">{{cite journal |author1=Mascarenhas M.N. |author2=Flaxman S.R. |author3=Boerma T. |author4=Vanderpoel S. |author5=Stevens G.A. | year = 2012 | title = National, Regional, and Global Trends in Infertility Prevalence Since 1990: A Systematic Analysis of 277 Health Surveys | url = | journal = PLOS Med | volume = 9 | issue = 12| page = e1001356 | doi = 10.1371/journal.pmed.1001356 |pmid=23271957 |pmc=3525527 }}</ref> Infertility is caused by many sources, including nutrition, diseases, and other malformations of the uterus. Infertility affects women from around the world, and the cultural and social stigma surrounding it varies. |
|||
==Cause== |
|||
Causes or factors of female infertility can basically be classified regarding whether they are [[Acquired disorder|acquired]] or genetic, or strictly by location. |
|||
Although factors of female infertility can be classified as either acquired or genetic, female infertility is usually more or less a combination of [[nature and nurture]]. Also, the presence of any single [[risk factor]] of female infertility (such as smoking, mentioned further below) does not necessarily cause infertility, and even if a woman is definitely infertile, the infertility cannot definitely be blamed on any single risk factor even if the risk factor is (or has been) present. |
|||
===Acquired=== |
|||
According to the [[American Society for Reproductive Medicine]] (ASRM), age, smoking, sexually transmitted infections, and being overweight or underweight can all affect fertility.<ref>http://www.fertilityfaq.org/_pdf/magazine1_v4.pdf{{dead link|date=September 2017 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> |
|||
In broad sense, acquired factors practically include any factor that is not based on a [[genetic mutation]], including any [[Environmental toxins in pregnancy|intrauterine exposure to toxins during fetal development]], which may present as infertility many years later as an adult. |
|||
====Age==== |
|||
{{Main|Age and female fertility}} |
|||
A woman's fertility is affected by her age. The average age of a girl's first period ([[menarche]]) is 12–13 (12.5 years in the [[United States]],<ref>{{cite journal |vauthors=Anderson SE, Dallal GE, Must A |title=Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart |journal=Pediatrics |volume=111 |issue=4 Pt 1 |pages=844–50 |date=April 2003 |pmid=12671122 |doi=10.1542/peds.111.4.844}}</ref> 12.72 in [[Canada]],<ref>{{cite journal |pmid=21110899 | doi=10.1186/1471-2458-10-736 | volume=10 | title=Age at menarche in Canada: results from the National Longitudinal Survey of Children & Youth | pmc=3001737 | year=2010 |vauthors=Al-Sahab B, Ardern CI, Hamadeh MJ, Tamim H | journal=BMC Public Health | pages=736}}</ref> 12.9 in the [[UK]]<ref>http://vstudentworld.yolasite.com/resources/final_yr/gynae_obs/Hamilton%20Fairley%20Obstetrics%20and%20Gynaecology%20Lecture%20Notes%202%20Ed.pdf</ref>), but, in postmenarchal girls, about 80% of the cycles are [[anovulatory]] in the first year after menarche, 50% in the third and 10% in the sixth year.<ref name="Apter D 1980 107–20">{{cite journal |author=Apter D |title=Serum steroids and pituitary hormones in female puberty: a partly longitudinal study |journal=Clinical Endocrinology |volume=12 |issue=2 |pages=107–20 |date=February 1980 |pmid=6249519 |doi=10.1111/j.1365-2265.1980.tb02125.x}}</ref> A woman's fertility peaks in the early and mid 20s, after which it starts to decline, with this decline being accelerated after age 35. However, the exact estimates of the chances of a woman to conceive after a certain age are not clear, with research giving differing results. The chances of a couple to successfully conceive at an advanced age depend on many factors, including the general health of a woman and the fertility of the male partner. |
|||
====Tobacco smoking==== |
|||
{{See also|Women and smoking#Unique gender differences and health effects for Females}} |
|||
[[Tobacco smoking]] is harmful to the ovaries, and the degree of damage is dependent upon the amount and length of time a woman smokes or is exposed to a smoke-filled environment. Nicotine and other harmful chemicals in cigarettes interfere with the body’s ability to create [[estrogen]], a hormone that regulates [[folliculogenesis]] and [[ovulation]]. Also, cigarette smoking interferes with folliculogenesis, embryo transport, endometrial receptivity, endometrial angiogenesis, uterine blood flow and the uterine myometrium.<ref>{{cite journal|vauthors=Dechanet C, Anahory T, Mathieu Daude JC, Quantin X, Reyftmann L, Hamamah S, Hedon B, Dechaud H | title = Effects of cigarette smoking on reproduction| journal = Hum. Reprod. Update| volume = 17| issue = 1| pages = 76–95| year = 2011| pmid = 20685716| doi = 10.1093/humupd/dmq033| url = }}</ref> Some damage is irreversible, but stopping smoking can prevent further damage.<ref name=asrm-risks>[http://www.protectyourfertility.com/femalerisks.html FERTILITY FACT > Female Risks] {{webarchive |url=https://web.archive.org/web/20070922184324/http://www.protectyourfertility.com/femalerisks.html |date=September 22, 2007 }} By the American Society for Reproductive Medicine (ASRM). Retrieved on Jan 4, 2009</ref><ref name="bare_url">http://dl.dropbox.com/u/8256710/ASRM%20Protect%20Your%20Fertility%20newsletter.pdf{{dead link|date=January 2018 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> Smokers are 60% more likely to be infertile than non-smokers.<ref name=dh2009/> Smoking reduces the chances of IVF producing a live birth by 34% and increases the risk of an IVF pregnancy miscarrying by 30%.<ref name=dh2009>[http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_101070 Regulated fertility services: a commissioning aid - June 2009], from the Department of Health UK</ref> Also, female smokers have an earlier onset of [[menopause]] by approximately 1–4 years.<ref name = "smoking and infertility">{{cite journal |author=Practice Committee of American Society for Reproductive Medicine |title=Smoking and Infertility |journal=Fertil Steril |volume=90 |issue=5 Suppl |pages=S254–9 |year=2008 |pmid=19007641 |doi=10.1016/j.fertnstert.2008.08.035}}</ref> |
|||
====Sexually transmitted infections==== |
|||
[[Sexually transmitted infection]]s are a leading cause of infertility. They often display few, if any visible symptoms, with the risk of failing to seek proper treatment in time to prevent decreased fertility.<ref name=asrm-risks/> |
|||
====Body weight and eating disorders==== |
|||
Twelve percent of all infertility cases are a result of a woman either being [[underweight]] or [[overweight]]. [[Adipocyte|Fat cells]] produce estrogen,<ref>{{cite journal |vauthors=Nelson LR, Bulun SE |title=Estrogen production and action |journal=J. Am. Acad. Dermatol. |volume=45 |issue=3 Suppl |pages=S116–24 |date=September 2001 |pmid=11511861 |doi= 10.1067/mjd.2001.117432}}</ref> in addition to the primary [[sex organ]]s. Too much body fat causes production of too much estrogen and the body begins to react as if it is on birth control, limiting the odds of getting pregnant.<ref name=asrm-risks/> Too little body fat causes insufficient production of estrogen and disruption of the [[menstrual cycle]].<ref name=asrm-risks/> Both under and overweight women have irregular cycles in which ovulation does not occur or is inadequate.<ref name=asrm-risks/> Proper nutrition in early life is also a major factor for later fertility.<ref>{{Cite journal | doi = 10.1093/humupd/dmq048 | last1 = Sloboda | first1 = D. M. | last2 = Hickey | first2 = M. | pmid = 20961922 | last3 = Hart | first3 = R. | title = Reproduction in females: the role of the early life environment | journal = Human Reproduction Update | volume = 17 | issue = 2 | pages = 210–227 | year = 2010}}</ref> |
|||
A study in the US indicated that approximately 20% of infertile women had a past or current eating disorder, which is five times higher than the general lifetime prevalence rate.<ref>{{cite journal |vauthors=Freizinger M, Franko DL, Dacey M, Okun B, Domar AD |title=The prevalence of eating disorders in infertile women |journal=Fertil. Steril. |volume= 93|issue= 1|pages= 72–8|date=November 2008 |pmid=19006795 |doi=10.1016/j.fertnstert.2008.09.055 }}</ref> |
|||
A review from 2010 concluded that overweight and obese subfertile women have a reduced probability of successful fertility treatment and their pregnancies are associated with more complications and higher costs.<ref>{{cite web|title=Fertility of male and female and treatment |url=http://www.morpheusivf.com/smart-treatment-plans/overview|accessdate=26 September 2015}}</ref> In hypothetical groups of 1000 women undergoing fertility care, the study counted approximately 800 live births for normal weight and 690 live births for overweight and obese anovulatory women. For ovulatory women, the study counted approximately 700 live births for normal weight, 550 live births for overweight and 530 live births for obese women. The increase in cost per live birth in anovulatory overweight and obese women were, respectively, 54 and 100% higher than their normal weight counterparts, for ovulatory women they were 44 and 70% higher, respectively.<ref>{{cite journal |vauthors=Koning AM, Kuchenbecker WK, Groen H, etal |title=Economic consequences of overweight and obesity in infertility: a framework for evaluating the costs and outcomes of fertility care |journal=Hum. Reprod. Update |volume=16 |issue=3 |pages=246–54 |year=2010 |pmid=20056674 |doi=10.1093/humupd/dmp053 }}</ref> |
|||
====Radiation==== |
|||
Exposure to radiation poses a high risk of infertility, depending on the frequency, power, and exposure duration. [[Radiotherapy]] is reported to cause infertility,<ref>[https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/fertility-and-sexual-side-effects/fertility-and-women-with-cancer/how-cancer-treatments-affect-fertility.html How Cancer Treatments Can Affect Fertility in Women]</ref> and [[5G#Frequency_range_2_(>_24_GHz)|5G wave 2]] is rumored to cause infertility. |
|||
<blockquote>the amount of radiation absorbed by the ovaries will determine if she becomes infertile. High doses can destroy some or all of the eggs in the ovaries and might cause infertility or early menopause. </blockquote> |
|||
====Chemotherapy==== |
|||
[[Chemotherapy]] poses a high risk of infertility. Chemotherapies with high risk of infertility include procarbazine and other alkylating drugs such as cyclophosphamide, ifosfamide, busulfan, melphalan, chlorambucil and chlormethine.<ref name=Brydoy>{{cite journal |vauthors=Brydøy M, Fosså SD, Dahl O, Bjøro T |title=Gonadal dysfunction and fertility problems in cancer survivors |journal=Acta Oncol |volume=46 |issue=4 |pages=480–9 |year=2007 |pmid=17497315 |doi=10.1080/02841860601166958 }}</ref> Drugs with medium risk include doxorubicin and platinum analogs such as cisplatin and carboplatin.<ref name=Brydoy/> On the other hand, therapies with low risk of gonadotoxicity include plant derivatives such as vincristine and vinblastine, antibiotics such as bleomycin and dactinomycin and antimetabolites such as methotrexate, mercaptopurine and 5-fluorouracil.<ref name=Brydoy/> |
|||
Female infertility by chemotherapy appears to be secondary to [[premature ovarian failure]] by loss of [[primordial follicles]].<ref name=Morgan2012>{{Cite journal | last1 = Morgan | first1 = S. | last2 = Anderson | first2 = R. A. | last3 = Gourley | first3 = C. | last4 = Wallace | first4 = W. H. | last5 = Spears | first5 = N. | title = How do chemotherapeutic agents damage the ovary? | doi = 10.1093/humupd/dms022 | journal = Human Reproduction Update | volume = 18 | issue = 5 | pages = 525–35 | year = 2012 | pmid = 22647504| pmc = }}</ref> This loss is not necessarily a direct effect of the chemotherapeutic agents, but could be due to an increased rate of growth initiation to replace damaged developing follicles.<ref name=Morgan2012/> [[Antral follicle count]] decreases after three series of chemotherapy, whereas [[follicle stimulating hormone]] (FSH) reaches menopausal levels after four series.<ref name=Rosendahl/> Other hormonal changes in chemotherapy include decrease in [[inhibin B]] and [[anti-Müllerian hormone]] levels.<ref name=Rosendahl>{{Cite journal| last1 = Rosendahl | first1 = M.| last2 = Andersen | first2 = C.| last3 = La Cour Freiesleben | first3 = N.| last4 = Juul | first4 = A.| last5 = Løssl | first5 = K.| last6 = Andersen | first6 = A.| title = Dynamics and mechanisms of chemotherapy-induced ovarian follicular depletion in women of fertile age| journal = Fertility and Sterility| volume = 94| issue = 1| pages = 156–166| year = 2010| pmid = 19342041| doi = 10.1016/j.fertnstert.2009.02.043}}</ref> |
|||
Women may choose between several methods of [[fertility preservation]] prior to chemotherapy, including [[cryopreservation]] of ovarian tissue, oocytes or embryos.<ref>{{cite journal |vauthors=Gurgan T, Salman C, Demirol A |title=Pregnancy and assisted reproduction techniques in men and women after cancer treatment |journal=Placenta |volume=29 |issue=Suppl B |pages=152–9 |date=October 2008 |pmid=18790328 |doi=10.1016/j.placenta.2008.07.007 }}</ref> |
|||
==== Immune infertility ==== |
|||
[[Antisperm antibodies]] (ASA) have been considered as infertility cause in around 10–30% of infertile couples.<ref name=":0">{{Cite journal|last=Restrepo|first=B.|last2=Cardona-Maya|first2=W.|date=October 2013|title=Antisperm antibodies and fertility association|journal=Actas Urologicas Espanolas|volume=37|issue=9|pages=571–578|doi=10.1016/j.acuro.2012.11.003|issn=1699-7980|pmid=23428233}}</ref> ASA production are directed against surface antigens on sperm, which can interfere with sperm motility and transport through the female reproductive tract, inhibiting capacitation and [[acrosome reaction]], impaired [[Fertilisation|fertilization]], influence on the implantation process, and impaired growth and development of the [[embryo]]. Factors contributing to the formation of antisperm antibodies in women are disturbance of normal immunoregulatory mechanisms, infection, violation of the integrity of the mucous membranes, accidental rape and unprotected oral or anal sex.<ref name=":0" /><ref name=":1">{{Cite book|url=https://books.google.com/books?id=QfK8AQAAQBAJ&pg=PA311|title=Principles & Practice of Assisted Reproductive Technology (3 Vols)|last=Rao|first=Kamini|date=2013-09-30|publisher=JP Medical Ltd|isbn=9789350907368|language=en}}</ref> |
|||
====Other acquired factors==== |
|||
*[[Adhesion (medicine)|Adhesions]] secondary to [[surgery]] in the [[peritoneal cavity]] is the leading cause of acquired infertility.<ref name=Broek2012>{{Cite journal | last1 = Ten Broek | first1 = R. P. G. | last2 = Kok- Krant | first2 = N. | last3 = Bakkum | first3 = E. A. | last4 = Bleichrodt | first4 = R. P. | last5 = Van Goor | first5 = H. | title = Different surgical techniques to reduce post-operative adhesion formation: A systematic review and meta-analysis | doi = 10.1093/humupd/dms032 | journal = Human Reproduction Update | volume = 19 | issue = 1 | pages = 12–25 | year = 2012 | pmid = 22899657| pmc = }}</ref> A meta-analysis in 2012 came to the conclusion that there is only little evidence for the surgical principle that using less invasive techniques, introducing less foreign bodies or causing less ischemia reduces the extent and severity of adhesions.<ref name=Broek2012/> |
|||
*[[Diabetes mellitus]]. A review of type 1 diabetes came to the result that, despite modern treatment, women with diabetes are at increased risk of female infertility, such as reflected by delayed puberty and menarche, menstrual irregularities (especially [[oligomenorrhoea]]), mild [[hyperandrogenism]], [[polycystic ovarian syndrome]], fewer live born children and possibly earlier [[menopause]].<ref name=Codner2012>{{Cite journal | last1 = Codner | first1 = E. | last2 = Merino | first2 = P. M. | last3 = Tena-Sempere | first3 = M. | doi = 10.1093/humupd/dms024 | title = Female reproduction and type 1 diabetes: From mechanisms to clinical findings | journal = Human Reproduction Update | volume = 18 | issue = 5 | pages = 568–585 | year = 2012 | pmid = 22709979| pmc = }}</ref> Animal models indicate that abnormalities on the molecular level caused by diabetes include defective [[leptin]], [[insulin]] and [[kisspeptin]] signalling.<ref name=Codner2012/> |
|||
*[[Coeliac disease]]. Non-gastrointestinal symptoms of coeliac disease may include disorders of fertility, such as delayed menarche, [[amenorrea]], infertility or early menopause; and [[pregnancy]] complications, such as [[intrauterine growth restriction]] (IUGR), [[small for gestational age]] (SGA) babies, recurrent [[abortion]]s, [[preterm birth|preterm deliveries]] or [[low birth weight]] (LBW) babies. Nevertheless, [[gluten-free diet]] reduces the risk. Some authors suggest that physicians should investigate the presence of undiagnosed coeliac disease in women with unexplained infertility, recurrent miscarriage or IUGR.<ref name=TersigniCastellani>{{cite journal |vauthors=Tersigni C, Castellani R, de Waure C, Fattorossi A, De Spirito M, Gasbarrini A, Scambia G, Di Simone N |title= Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms |date= 2014 |journal= Hum. Reprod. Update |volume= 20 |issue= 4 |pages=582–93 |doi=10.1093/humupd/dmu007 |url= http://humupd.oxfordjournals.org/content/20/4/582.long |pmid= 24619876 | type= Meta-Analysis. Review}}</ref><ref name=LasaZubiaurre>{{cite journal |last= Lasa |first= JS |last2= Zubiaurre |first2= I |last3= Soifer |first3= LO |title= Risk of infertility in patients with celiac disease: a meta-analysis of observational studies |date= 2014 |journal= Arq Gastroenterol |volume= 51 |issue= 2 |pages=144–50 |doi=10.1590/S0004-28032014000200014 |pmid= 25003268 | type= Meta-Analysis. Review}}</ref> |
|||
*Significant [[liver]] or [[kidney]] disease |
|||
*[[Thrombophilia]]<ref name="pmid17433901">{{cite journal |author=Middeldorp S |title=Pregnancy failure and heritable thrombophilia |journal=Semin. Hematol. |volume=44 |issue=2 |pages=93–7 |year=2007 |pmid=17433901 |doi=10.1053/j.seminhematol.2007.01.005}}</ref><ref name="pmid16835215">{{cite journal |vauthors=Qublan HS, Eid SS, Ababneh HA, etal |title=Acquired and inherited thrombophilia: implication in recurrent IVF and embryo transfer failure |journal=Hum. Reprod. |volume=21 |issue=10 |pages=2694–8 |year=2006 |pmid=16835215 |doi=10.1093/humrep/del203|citeseerx=10.1.1.544.3649 }}</ref> |
|||
*[[Cannabis smoking]], such as of [[marijuana]] causes disturbances in the [[endocannabinoid system]], potentially causing infertility<ref>{{Cite journal | last1 = Karasu | first1 = T. | last2 = Marczylo | first2 = T. H. | last3 = MacCarrone | first3 = M. | last4 = Konje | first4 = J. C. | title = The role of sex steroid hormones, cytokines and the endocannabinoid system in female fertility | doi = 10.1093/humupd/dmq058 | journal = Human Reproduction Update | volume = 17 | issue = 3 | pages = 347–361 | year = 2011 | pmid = 21227997| pmc = }}</ref> |
|||
*Radiation, such as in [[radiation therapy]]. The radiation dose to the ovaries that generally causes permanent female infertility is 20.3 [[Gray (unit)|Gy]] at birth, 18.4 Gy at 10 years, 16.5 Gy at 20 years and 14.3 Gy at 30 years.<ref>{{cite journal |author1=Tichelli André |author2=Rovó Alicia | year = 2013 | title = Fertility Issues Following Hematopoietic Stem Cell Transplantation | url = http://www.medscape.com/viewarticle/810686_2?nlid=34365_904 | journal = Expert Rev Hematol | volume = 6 | issue = 4| pages = 375–388 | doi=10.1586/17474086.2013.816507 | pmid=23991924}} |
|||
<br>In turn citing: {{cite journal |vauthors=Wallace WH, Thomson AB, Saran F, Kelsey TW | year = 2005 | title = Predicting age of ovarian failure after radiation to a field that includes the ovaries | url = | journal = Int. J. Radiat. Oncol. Biol. Phys. | volume = 62 | issue = 3| pages = 738–744 | doi = 10.1016/j.ijrobp.2004.11.038 | pmid = 15936554 }}</ref> After [[total body irradiation]], recovery of gonadal function occurs in 10−14% of cases, and the number of pregnancies observed after [[hematopoietic stem cell transplantation]] involving such as procedure is lower than 2%.<ref>{{cite journal |author1=Tichelli André |author2=Rovó Alicia | year = 2013 | title = Fertility Issues Following Hematopoietic Stem Cell Transplantation | url = http://www.medscape.com/viewarticle/810686_2?nlid=34365_904 | journal = Expert Rev Hematol | volume = 6 | issue = 4| pages = 375–388 | doi=10.1586/17474086.2013.816507 | pmid=23991924}}</ref><ref><br>In turn citing: {{cite journal |vauthors=Salooja N, Szydlo RM, Socie G, etal | year = 2001| title = Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey | url = | journal = Lancet | volume = 358 | issue = 9278| pages = 271–276 | doi=10.1016/s0140-6736(01)05482-4}}</ref> |
|||
===Genetic factors=== |
|||
There are many [[gene]]s wherein [[mutation]] causes female infertility, as shown in table below. Also, there are additional conditions involving female infertility which are believed to be genetic but where no single gene has been found to be responsible, notably [[Mayer-Rokitansky-Küstner-Hauser Syndrome]] (MRKH).<ref>{{cite journal |vauthors=Sultan C, Biason-Lauber A, Philibert P |title=Mayer-Rokitansky-Kuster-Hauser syndrome: recent clinical and genetic findings |journal=Gynecol Endocrinol |volume=25 |issue=1 |pages=8–11 |date=January 2009 |pmid=19165657 |doi=10.1080/09513590802288291 }}</ref> Finally, an unknown number of genetic mutations cause a state of subfertility, which in addition to other factors such as environmental ones may manifest as frank infertility. |
|||
[[Chromosomal abnormality|Chromosomal abnormalities]] causing female infertility include [[Turner syndrome]]. Oocyte donation is an alternative for patients with Turner syndrome.<ref>{{cite journal |vauthors=Bodri D, Vernaeve V, Figueras F, Vidal R, Guillén JJ, Coll O |title=Oocyte donation in patients with Turner's syndrome: a successful technique but with an accompanying high risk of hypertensive disorders during pregnancy |journal=Hum. Reprod. |issue=3 |pages=829–832|date=March 2006 |pmid=16311294 |doi=10.1093/humrep/dei396 |volume=21}}</ref> |
|||
Some of these gene or chromosome abnormalities cause [[intersexuality|intersex conditions]], such as [[androgen insensitivity syndrome]]. |
|||
{|class="wikitable" |
|||
|+[[Gene]]s wherein [[mutation]] causes female infertility<ref name=Evian2010>Unless otherwise specified in boxes, then reference is: {{Cite journal| author1 = The Evian Annual Reproduction (EVAR) Workshop Group 2010 | last2 = Fauser | first2 = B. C. J. M. | last3 = Diedrich | first3 = K. | last4 = Bouchard | first4 = P. | last5 = Domínguez | first5 = F. | last6 = Matzuk | first6 = M. | last7 = Franks | first7 = S. | last8 = Hamamah | first8 = S. | last9 = Simón | first9 = C. | last10 = Devroey | first10 = P. | last11 = Ezcurra | first11 = D. | last12 = Howles | first12 = C. M. | title = Contemporary genetic technologies and female reproduction | journal = Human Reproduction Update | volume = 17 | issue = 6 | pages = 829–847 | year = 2011 | pmid = 21896560 | pmc = 3191938 | doi = 10.1093/humupd/dmr033}}</ref> |
|||
|- |
|||
! Gene !! Encoded protein !! Effect of deficiency |
|||
|- |
|||
| [[BMP15]] || [[Bone morphogenetic protein 15]] || Hypergonadotrophic ovarian failure ([[POF4]]) |
|||
|- |
|||
| [[BMPR1B]] || [[Bone morphogenetic protein receptor 1B]] || Ovarian dysfunction, hypergonadotrophic hypogonadism and acromesomelic chondrodysplasia |
|||
|- |
|||
| [[CBX2 (gene)|CBX2]]; [[M33 (gene)|M33]] || [[Chromobox protein homolog 2]]; Drosophila polycomb class || |
|||
Autosomal 46,XY, male-to-female sex reversal (phenotypically perfect females) |
|||
|- |
|||
| [[CHD7]] || [[Chromodomain-helicase-DNA-binding protein 7]] || [[CHARGE syndrome]] and [[Kallmann syndrome]] ([[KAL5]]) |
|||
|- |
|||
| [[DIAPH2]] || [[Diaphanous homolog 2]] || Hypergonadotrophic, premature ovarian failure ([[POF2A]]) |
|||
|- |
|||
| [[FGF8]] || [[Fibroblast growth factor 8]] || Normosmic hypogonadotrophic hypogonadism and Kallmann syndrome (KAL6) |
|||
|- |
|||
| [[FGFR1]] || [[Fibroblast growth factor receptor 1]] || Kallmann syndrome (KAL2) |
|||
|- |
|||
| [[HFM1]] || || [[Primary ovarian failure]]<ref name="WangZhang2014">{{cite journal|last1=Wang|first1=Jian|last2=Zhang|first2=Wenxiang|last3=Jiang|first3=Hong|last4=Wu|first4=Bai-Lin|title=Mutations inHFM1in Recessive Primary Ovarian Insufficiency|journal=New England Journal of Medicine|volume=370|issue=10|year=2014|pages=972–974|issn=0028-4793|doi=10.1056/NEJMc1310150|pmid=24597873}}</ref> |
|||
|- |
|||
| [[FSHR]] || [[FSH receptor]] || Hypergonadotrophic hypogonadism and ovarian hyperstimulation syndrome |
|||
|- |
|||
| [[FSHB]] || [[Follitropin subunit beta]] || Deficiency of follicle-stimulating hormone, primary amenorrhoea and infertility |
|||
|- |
|||
| [[FOXL2]] || [[Forkhead box L2]] || Isolated premature ovarian failure (POF3) associated with BPES type I; FOXL2 |
|||
402C --> G mutations associated with human granulosa cell tumours |
|||
|- |
|||
| [[FMR1]] || [[Fragile X mental retardation]] || Premature ovarian failure (POF1) associated with premutations |
|||
|- |
|||
| [[GNRH1]] || [[Gonadotropin releasing hormone]] || Normosmic hypogonadotrophic hypogonadism |
|||
|- |
|||
| [[GNRHR]] || [[GnRH receptor]] || Hypogonadotrophic hypogonadism |
|||
|- |
|||
| [[KAL1]] || Kallmann syndrome || Hypogonadotrophic hypogonadism and insomnia, X-linked Kallmann syndrome (KAL1) |
|||
|- |
|||
| [[KISS1R]]; [[GPR54]] || [[KISS1 receptor]] || Hypogonadotrophic hypogonadism |
|||
|- |
|||
| [[Luteinizing hormone beta polypeptide|LHB]] || [[Luteinizing hormone beta polypeptide]] || Hypogonadism and [[pseudohermaphroditism]] |
|||
|- |
|||
| [[LHCGR]] || [[LH/choriogonadotrophin receptor]] || Hypergonadotrophic hypogonadism (luteinizing hormone resistance) |
|||
|- |
|||
| [[DAX1]] || [[Dosage-sensitive sex reversal, adrenal hypoplasia critical region, on chromosome X, gene 1]] || X-linked congenital adrenal hypoplasia with hypogonadotrophic hypogonadism; dosage-sensitive male-to-female sex reversal |
|||
|- |
|||
| [[NR5A1]]; [[SF1 (gene)|SF1]] || [[Steroidogenic factor 1]] || 46,XY male-to-female sex reversal and streak gonads and congenital lipoid adrenal hyperplasia; 46,XX gonadal dysgenesis and 46,XX primary ovarian insufficiency |
|||
|- |
|||
| [[POF1B]] || [[Premature ovarian failure 1B]] || Hypergonadotrophic, primary amenorrhea ([[POF2B]]) |
|||
|- |
|||
| [[PROK2]] || [[Prokineticin]] || Normosmic hypogonadotrophic hypogonadism and Kallmann syndrome ([[KAL4]]) |
|||
|- |
|||
| [[PROKR2]] || [[Prokineticin receptor 2]] || Kallmann syndrome ([[KAL3]]) |
|||
|- |
|||
| [[RSPO1]] || [[R-spondin family, member 1]] || 46,XX, female-to-male sex reversal (individuals contain testes) |
|||
|- |
|||
| [[SRY]] || [[Sex-determining region Y]] || Mutations lead to 46,XY females; translocations lead to 46,XX males |
|||
|- |
|||
| [[SCNN1A]] || Alpha subunit of [[Epithelial sodium channel]] (ENaC) || Nonsense mutation leads to defective expression of ENaC in the female reproductive tract<ref name="2018-Boggula">{{cite journal | vauthors = Boggula VR, Hanukoglu I, Sagiv R, Enuka Y, Hanukoglu A | title = Expression of the epithelial sodium channel (ENaC) in the endometrium - Implications for fertility in a patient with pseudohypoaldosteronism | journal = The Journal of Steroid Biochemistry and Molecular Biology | volume = 183 | issue = | pages = 137–141 | date = October 2018 | pmid = 29885352 | doi = 10.1016/j.jsbmb.2018.06.007 }}</ref> |
|||
|- |
|||
| [[SOX9]] || [[SRY-related HMB-box gene 9]] || |
|||
|- |
|||
| [[STAG3]] || [[Stromal antigen 3]] || [[Premature ovarian failure]]<ref name="CaburetArboleda2014">{{cite journal|last1=Caburet|first1=Sandrine|last2=Arboleda|first2=Valerie A.|last3=Llano|first3=Elena|last4=Overbeek|first4=Paul A.|last5=Barbero|first5=Jose Luis|last6=Oka|first6=Kazuhiro|last7=Harrison|first7=Wilbur|last8=Vaiman|first8=Daniel|last9=Ben-Neriah|first9=Ziva|last10=García-Tuñón|first10=Ignacio|last11=Fellous|first11=Marc|last12=Pendás|first12=Alberto M.|last13=Veitia|first13=Reiner A.|last14=Vilain|first14=Eric|title=Mutant Cohesin in Premature Ovarian Failure|journal=New England Journal of Medicine|volume=370|issue=10|year=2014|pages=943–949|issn=0028-4793|doi=10.1056/NEJMoa1309635|pmid=24597867|pmc=4068824}}</ref> |
|||
|- |
|||
| [[TAC3]] || [[Tachykinin 3]] || Normosmic hypogonadotrophic hypogonadism |
|||
|- |
|||
| [[TACR3]] || [[Tachykinin receptor 3]] || Normosmic hypogonadotrophic hypogonadism |
|||
|- |
|||
| [[ZP1]] || [[zona pellucida glycoprotein 1]] || Dysfunctional [[zona pellucida]] formation<ref name="HuangLv2014">{{cite journal|last1=Huang|first1=Hua-Lin|last2=Lv|first2=Chao|last3=Zhao|first3=Ying-Chun|last4=Li|first4=Wen|last5=He|first5=Xue-Mei|last6=Li|first6=Ping|last7=Sha|first7=Ai-Guo|last8=Tian|first8=Xiao|last9=Papasian|first9=Christopher J.|last10=Deng|first10=Hong-Wen|last11=Lu|first11=Guang-Xiu|last12=Xiao|first12=Hong-Mei|title=Mutant ZP1 in Familial Infertility|journal=New England Journal of Medicine|volume=370|issue=13|year=2014|pages=1220–1226|issn=0028-4793|doi=10.1056/NEJMoa1308851|pmid=24670168|pmc=4076492}}</ref> |
|||
| |
|||
|} |
|||
===By location=== |
|||
====Hypothalamic-pituitary factors==== |
|||
*[[Hypothalamic dysfunction]] |
|||
*[[Hyperprolactinemia]]<ref>[http://www.getting-pregnant-tips.com/female-infertility.html Female Infertility] {{webarchive|url=https://web.archive.org/web/20100218012801/http://www.getting-pregnant-tips.com/female-infertility.html |date=2010-02-18 }}</ref> |
|||
====Ovarian factors==== |
|||
* [[Chemotherapy]] (as detailed previously) with certain agents have a high risk of toxicity on the ovaries. |
|||
*Many genetic defects (as also detailed previously) also disturb ovarian function. |
|||
* [[Polycystic ovary syndrome]] (also see [[infertility in polycystic ovary syndrome]]) |
|||
*[[Anovulation]]. Female infertility caused by anovulation is called "anovulatory infertility", as opposed to "ovulatory infertility" in which ovulation is present.<ref>{{cite journal |vauthors=Hull MG, Savage PE, Bromham DR |title=Anovulatory and ovulatory infertility: results with simplified management |journal=Br Med J (Clin Res Ed) |volume=284 |issue=6330 |pages=1681–5 |date=June 1982 |pmid=6805656 |pmc=1498620 |doi= 10.1136/bmj.284.6330.1681}}</ref> |
|||
*Diminished [[ovarian reserve]], also see [[poor ovarian reserve|Poor Ovarian Reserve]] |
|||
*[[Premature menopause]] |
|||
*[[Menopause]] |
|||
*Luteal dysfunction<ref>{{EMedicine|med|1340|Luteal Phase Dysfunction}}</ref> |
|||
*Gonadal dysgenesis ([[Turner syndrome]]) |
|||
*[[Ovarian cancer]] |
|||
====Tubal (ectopic)/peritoneal factors==== |
|||
{{Further|Tubal factor infertility}} |
|||
*[[Endometriosis]] (also see [[endometriosis and infertility]]) |
|||
*Pelvic [[Adhesion (medicine)|adhesions]] |
|||
*[[Pelvic inflammatory disease]] (PID, usually due to [[Chlamydia infection|chlamydia]])<ref name="pmid17160569">{{cite journal |vauthors=Guven MA, Dilek U, Pata O, Dilek S, Ciragil P |title=Prevalence of Chlamydia trochomatis, Ureaplasma urealyticum and Mycoplasma hominis infections in the unexplained infertile women |journal=Arch. Gynecol. Obstet. |volume=276 |issue=3 |pages=219–23 |year=2007 |pmid=17160569 |doi=10.1007/s00404-006-0279-z}}</ref> |
|||
*Tubal dysfunction |
|||
*Previous [[ectopic pregnancy]]. A randomized study in 2013 came to the result that the rates of intrauterine pregnancy two years after treatment of ectopic pregnancy are approximately 64% with radical surgery, 67% with medication, and 70% with conservative surgery.<ref>{{Cite journal | last1 = Fernandez | first1 = H. | last2 = Capmas | first2 = P. | last3 = Lucot | first3 = J. P. | last4 = Resch | first4 = B. | last5 = Panel | first5 = P. | last6 = Bouyer | first6 = J. | doi = 10.1093/humrep/det037 | title = Fertility after ectopic pregnancy: The DEMETER randomized trial | journal = Human Reproduction | volume = 28 | issue = 5 | pages = 1247–1253 | year = 2013 | pmid = 23482340| pmc = }}</ref> In comparison, the cumulative pregnancy rate of women under 40 years of age in the general population over two years is over 90%.<ref name=nice2013 /> |
|||
====Uterine factors==== |
|||
*[[Uterine malformation]]s<ref name="pmid9402295">{{cite journal |vauthors=Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simón C, Pellicer A |title=Reproductive impact of congenital Müllerian anomalies |journal=Hum. Reprod. |volume=12 |issue=10 |pages=2277–81 |year=1997 |pmid=9402295 |doi=10.1093/humrep/12.10.2277}}</ref> |
|||
*[[Uterine fibroids]] |
|||
*[[Asherman's Syndrome|Asherman's syndrome]]<ref name="pmid12470565">{{cite journal |author=Magos A |title=Hysteroscopic treatment of Asherman's syndrome |journal=Reprod. Biomed. Online |volume=4 |issue=Suppl 3 |pages=46–51 |year=2002 |pmid=12470565 |doi=10.1016/s1472-6483(12)60116-3}}</ref> |
|||
*[[Implantation failure]] without any known primary cause. It results in negative pregnancy test despite having performed e.g. [[embryo transfer]]. |
|||
Previously, a [[bicornuate uterus]] was thought to be associated with infertility,<ref>{{cite journal |vauthors=Shuiqing M, Xuming B, Jinghe L |title=Pregnancy and its outcome in women with malformed uterus |journal=Chin. Med. Sci. J. |volume=17 |issue=4 |pages=242–5 |year=2002 |pmid=12901513 |doi= |url=}}</ref> but recent studies have not confirmed such an association.<ref>{{cite journal |vauthors=Proctor JA, Haney AF |title=Recurrent first trimester pregnancy loss is associated with uterine septum but not with bicornuate uterus |journal=Fertil. Steril. |volume=80 |issue=5 |pages=1212–5 |year=2003 |pmid=14607577 |doi= 10.1016/S0015-0282(03)01169-5}}</ref> |
|||
====Cervical factors==== |
|||
*[[Stenosis of uterine cervix|Cervical stenosis]]<ref name="pmid17877600">{{cite journal |vauthors=Tan Y, Bennett MJ |title=Urinary catheter stent placement for treatment of cervical stenosis |journal=The Australian & New Zealand Journal of Obstetrics & Gynaecology |volume=47 |issue=5 |pages=406–9 |year=2007 |pmid=17877600 |doi=10.1111/j.1479-828X.2007.00766.x}}</ref> |
|||
*[[Antisperm antibodies]]<ref name=":1" /> |
|||
*Non-receptive cervical [[mucus]]<ref name="pmid7745077">{{cite journal |vauthors=Farhi J, Valentine A, Bahadur G, Shenfield F, Steele SJ, Jacobs HS |title=In-vitro cervical mucus-sperm penetration tests and outcome of infertility treatments in couples with repeatedly negative post-coital tests |journal=Hum. Reprod. |volume=10 |issue=1 |pages=85–90 |year=1995 |pmid=7745077 |doi=10.1093/humrep/10.1.85}}</ref> |
|||
====Vaginal factors==== |
|||
*[[Vaginismus]] |
|||
*Vaginal obstruction |
|||
==Diagnosis== |
|||
Diagnosis of infertility begins with a [[medical history]] and [[physical exam]]. The healthcare provider may order tests, including the following: |
|||
* Lab tests |
|||
** Hormone testing, to measure levels of female hormones at certain times during a [[menstrual cycle]]. |
|||
** Day 2 or 3 measure of [[Follicle-stimulating hormone|FSH]] and [[estrogen]], to assess [[ovarian reserve]]. |
|||
** Measurements of thyroid function<ref name="pmid16842634">{{cite journal |vauthors=Wartofsky L, Van Nostrand D, Burman KD |title=Overt and 'subclinical' hypothyroidism in women |journal=Obstetrical & Gynecological Survey |volume=61 |issue=8 |pages=535–42 |year=2006 |pmid=16842634 |doi=10.1097/01.ogx.0000228778.95752.66}}</ref> (a [[thyroid stimulating hormone]] (TSH) level of between 1 and 2 is considered optimal for conception). |
|||
** Measurement of [[progesterone]] in the second half of the cycle to help confirm ovulation. |
|||
**[[Anti-Müllerian hormone]] to estimate ovarian reserve.<ref name="BroerBroekmans2014">{{cite journal|last1=Broer|first1=S. L.|last2=Broekmans|first2=F. J. M.|last3=Laven|first3=J. S. E.|last4=Fauser|first4=B. C. J. M.|title=Anti-Mullerian hormone: ovarian reserve testing and its potential clinical implications|journal=Human Reproduction Update|volume=20|issue=5|year=2014|pages=688–701|issn=1355-4786|doi=10.1093/humupd/dmu020|pmid=24821925}}</ref> |
|||
* Examination and imaging |
|||
** An [[endometrial]] [[biopsy]], to verify ovulation and inspect the lining of the uterus. |
|||
** [[Laparoscopy]], which allows the provider to inspect the pelvic organs. |
|||
** [[Fertiloscopy]], a relatively new surgical technique used for early diagnosis (and immediate treatment). |
|||
** [[Pap smear]], to check for signs of infection. |
|||
** [[Pelvic exam]], to look for abnormalities or [[infection]]. |
|||
** A postcoital test, which is done soon after [[Sexual intercourse|intercourse]] to check for problems with sperm surviving in cervical mucous (not commonly used now because of test unreliability). |
|||
** [[Hysterosalpingography]] or [[sonosalpingography]], to check for tube patency |
|||
** [[Sonohysterography]] to check for uterine abnormalities. |
|||
There are [[genetic testing]] techniques under development to detect any mutation in genes associated with female infertility.<ref name=Evian2010/> |
|||
Initial diagnosis and treatment of infertility is usually made by [[obstetrician/gynecologist]]s or [[women's health nurse practitioner]]s. If initial treatments are unsuccessful, referral is usually made to physicians who are [[Fellowship (medicine)|fellowship]] trained as [[reproductive endocrinologist]]s. Reproductive endocrinologists are usually obstetrician/gynecologists with advanced training in reproductive endocrinology and infertility (in North America). These physicians treat reproductive disorders affecting not only women but also men, children, and teens. |
|||
Usually reproductive endocrinology & infertility medical practices do not see women for general [[maternity care]]. The practice is primarily focused on helping their women to conceive and to correct any issues related to recurring pregnancy loss. |
|||
===Definition=== |
|||
There is no unanimous definition of female infertility, because the definition depends on social and physical characteristics which may vary by culture and situation. [[NICE guidelines]] state that: "A woman of reproductive age who has not conceived after 1 year of unprotected vaginal sexual intercourse, in the absence of any known cause of infertility, should be offered further clinical assessment and investigation along with her partner."<ref name=nice2013>[http://guidance.nice.org.uk/CG156 Fertility: assessment and treatment for people with fertility problems]. [[NICE guidelines|NICE clinical guideline]] CG156 - Issued: February 2013</ref> It is recommended that a consultation with a [[fertility specialist]] should be made earlier if the woman is aged 36 years or over, or there is a known clinical cause of infertility or a history of predisposing factors for infertility.<ref name=nice2013/> According to the [[World Health Organization]] (WHO), infertility can be described as the inability to become pregnant, maintain a pregnancy, or carry a pregnancy to live birth.<ref name="WHO, 2013 ">World Health Organization 2013. "Health Topics: Infertility". Available http://www.who.int/topics/infertility/en/. Retrieved November 5, 2013.</ref> |
|||
A clinical definition of infertility by the [[WHO]] and ICMART is “a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.” <ref name=" Zegers-Hochschild">{{cite journal |author1=Zegers-Hochschild F. |author2=Adamson G.D. |author3=de Mouzon J. |author4=Ishihara O. |author5=Mansour R. |author6=Nygren K. |author7=Sullivan E. |author8=van der Poel S. | year = 2009 | title = The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009 | url = | journal = Human Reproduction | volume = 24 | issue = 11| pages = 2683–2687 | doi=10.1093/humrep/dep343|pmid=19801627 }}</ref> Infertility can further be broken down into primary and secondary infertility. [[Primary infertility]] refers to the inability to give birth either because of not being able to become pregnant, or carry a child to live birth, which may include miscarriage or a stillborn child. |
|||
<ref name="WHO terminology, 2013 ">World Health Organization 2013."Sexual and reproductive health: Infertility definitions and terminology". Available http://www.who.int/reproductivehealth/topics/infertility/definitions/en/ {{dead link|date=September 2017 |bot=InternetArchiveBot |fix-attempted=yes }}. Retrieved November 5, 2013.</ref><ref name="Rutstein 2004">Rutstein, Shea O., and Iqbal H. Shah. "Infecundity, Infertility, and Childlessness in Developing Countries." DHS Comparative Reports No. 9 (2004): 1-57.</ref> [[Secondary infertility]] refers to the inability to conceive or give birth when there was a previous pregnancy or live birth.<ref name="Rutstein 2004" /><ref name="WHO terminology, 2013" /> |
|||
==Prevention== |
|||
Acquired female infertility may be prevented through identified interventions: |
|||
* ''Maintaining a healthy lifestyle.'' Excessive exercise, consumption of [[caffeine]] and [[alcohol]], and [[smoking]] have all been associated with decreased fertility. Eating a well-balanced, nutritious diet, with plenty of fresh [[fruit]]s and [[vegetable]]s, and maintaining a normal weight, on the other hand, have been associated with better fertility prospects. |
|||
* ''Treating or preventing existing diseases.'' Identifying and controlling chronic diseases such as [[diabetes]] and [[hypothyroidism]] increases fertility prospects. Lifelong practice of [[safer sex]] reduces the likelihood that [[sexually transmitted disease]]s will impair fertility; obtaining prompt treatment for sexually transmitted diseases reduces the likelihood that such infections will do significant damage. Regular [[physical examination]]s (including pap smears) help detect early signs of infections or abnormalities. |
|||
* ''Not delaying parenthood.'' Fertility does not ultimately cease before menopause, but it starts declining after age 27 and drops at a somewhat greater rate after age 35.<ref name="titleStudy speeds up biological clocks / Fertility rates dip after women hit 27">{{cite news |url=http://www.sfgate.com/cgi-bin/article.cgi?file=/chronicle/archive/2002/04/30/MN182697.DTL |title=Study speeds up biological clocks / Fertility rates dip after women hit 27 |accessdate=2007-11-21 |work=The San Francisco Chronicle | first=Carl T. | last=Hall |date=April 30, 2002}}</ref> Women whose biological mothers had unusual or abnormal issues related to conceiving may be at particular risk for some conditions, such as [[premature menopause]], that can be mitigated by not delaying parenthood. |
|||
* ''[[oocyte cryopreservation|Egg freezing]].'' A woman can freeze her eggs preserve her fertility. By using [[egg freezing]] while in the peak reproductive years, a woman's [[oocytes]] are cryogenically frozen and ready for her use later in life, reducing her chances of female infertility.<ref>{{cite web|title=Information on Egg Freezing|url=https://www.pacificfertilitycenter.com/fertility-preservation/my-eggs|website=Egg Freezing|accessdate=6 March 2015}}</ref> |
|||
==Treatment== |
|||
There is no method to reverse [[advanced maternal age]], but there are [[assisted reproductive technologies]] for many causes of infertility in pre-menopausal women, including: |
|||
*[[Ovulation induction]] for [[anovulation]] |
|||
*[[In vitro fertilization]] in for example tubal abnormalities |
|||
==Epidemiology== |
|||
Female infertility varies widely by geographic location around the world. In 2010, there was an estimated 48.5 million infertile couples worldwide, and from 1990 to 2010 there was little change in levels of infertility in most of the world.<ref name="Mascarenhas, M.N. 2012"/> |
|||
In 2010, the countries with the lowest rates of female infertility included the South American countries of Peru, Ecuador and Bolivia, as well as in Poland, Kenya, and Republic of Korea.<ref name="Mascarenhas, M.N. 2012"/> The highest rate regions included Eastern Europe, North Africa, the Middle East, Oceania, and Sub-Saharan Africa.<ref name="Mascarenhas, M.N. 2012"/> The prevalence of primary infertility has increased since 1990, but secondary infertility has decreased overall. Rates decreased (although not prevalence) of female infertility in high-income, Central/Eastern Europe, and Central Asia regions.<ref name="Mascarenhas, M.N. 2012"/> |
|||
===Africa=== |
|||
Sub-Saharan Africa has had decreasing levels of primary infertility from 1990 to 2010. Within the Sub-Saharan region, rates were lowest in Kenya, Zimbabwe, and Rwanda, while the highest rates were in Guinea, Mozambique, Angola, Gabon, and Cameroon along with Northern Africa near the Middle East.<ref name="Mascarenhas, M.N. 2012"/> According to a 2004 DHS report, rates in Africa were highest in Middle and Sub-Saharan Africa, with East Africa’s rates close behind.<ref name="Rutstein 2004" /> |
|||
===Asia=== |
|||
In Asia, the highest rates of combined secondary and primary infertility was in the South Central region, and then in the Southeast region, with the lowest rates in the Western areas.<ref name="Rutstein 2004" /> |
|||
===Latin America and Caribbean=== |
|||
The prevalence of female infertility in the Latin America/Caribbean region is typically lower than the global prevalence. However, the greatest rates occurred in Jamaica, Suriname, Haiti, and Trinidad and Tobago. Central and Western Latin America has some of the lowest rates of prevalence.<ref name="Mascarenhas, M.N. 2012"/> The highest regions in Latin America and the Caribbean was in the Caribbean Islands and in less developed countries.<ref name="Rutstein 2004" /> |
|||
==Society and culture== |
|||
===Social stigma=== |
|||
Social stigma due to [[infertility]] is seen in many cultures throughout the world in varying forms. Often, when women cannot conceive, the blame is put on them, even when approximately 50% of [[infertility]] issues come from the man .<ref name="WHO 2010">{{cite journal | author = WHO | year = 2010 | title = Mother or nothing: the agony of infertility | url = | journal = Bulletin of the World Health Organization | volume = 88 | issue = 12| pages = 881–882 | doi = 10.2471/BLT.10.011210 | pmid = 21124709 | pmc = 2995184}}</ref> |
|||
In addition, many societies only tend to value a woman if she is able to produce at least one child, and a marriage can be considered a failure when the couple cannot [[conceive]].<ref name="WHO 2010"/> The act of conceiving a child can be linked to the couple’s consummation of marriage, and reflect their social role in society.<ref name="Araoye, M. O. 2003"/> This is seen in the "African infertility belt", where infertility is prevalent in Africa which includes countries spanning from [[Tanzania]] in the east to [[Gabon]] in the west.<ref name="WHO 2010"/> In this region, infertility is highly stigmatized and can be considered a failure of the couple to their societies.<ref name="WHO 2010"/><ref name="Leke 1993 ">Robert J. Leke, Jemimah A. Oduma, Susana Bassol-Mayagoitia, Angela Maria Bacha, and Kenneth M. Grigor. "Regional and Geographical Variations in Infertility: Effects of Environmental, Cultural, and Socioeconomic Factors" Environmental Health Perspectives Supplements (101) (Suppl. 2): 73-80 (1993).</ref> This is demonstrated in [[Uganda]] and [[Nigeria]] where there is a great pressure put on [[childbearing]] and its social implications.<ref name="Araoye, M. O. 2003"/> This is also seen in some Muslim societies including [[Egypt]] <ref name="Inhorn, M. C. 2003"/> and Pakistan.<ref name="Dyer, S. J. 2012"/> |
|||
Wealth is sometimes measured by the number of children a woman has, as well as inheritance of property.<ref name="Araoye, M. O. 2003"/><ref name="Dyer, S. J. 2012">Dyer, S. J. (2012). "The economic impact of infertility on women in developing countries – a systematic review." FVV in ObGyn: 38-45.</ref> Children can influence financial security in many ways. In Nigeria and [[Cameroon]], land claims are decided by the number of children. Also, in some Sub-Saharan countries women may be denied [[inheritance]] if she did not bear any children <ref name="Dyer, S. J. 2012"/> In some African and Asian countries a husband can deprive his infertile wife of food, shelter and other basic necessities like clothing.<ref name="Dyer, S. J. 2012"/> In Cameroon, a woman may lose access to land from her husband and left on her own in old age.<ref name="Araoye, M. O. 2003"/> |
|||
In many cases, a woman who cannot bear children is excluded from social and cultural events including traditional ceremonies. This stigmatization is seen in [[Mozambique]] and Nigeria where infertile women have been treated as outcasts to society.<ref name="Araoye, M. O. 2003"/> This is a humiliating practice which devalues infertile women in society.<ref name="Gerrits, T. 1997"/><ref name="Whiteford, L. M. 1995">Whiteford, L. M. (1995). "STIGMA: THE HIDDEN BURDEN OF INFERTILITY." Sot. Sci. Med. (40;1): 27-36.</ref> In the [[Makua people|Makua]] tradition, pregnancy and birth are considered major life events for a woman, with the ceremonies of nthaa´ra and ntha´ara no mwana, which can only be attended by women who have been pregnant and have had a baby.<ref name="Gerrits, T. 1997"/> |
|||
The effect of infertility can lead to social shaming from internal and [[social norms]] surrounding pregnancy, which affects women around the world.<ref name="Whiteford, L. M. 1995"/> When pregnancy is considered such an important event in life, and considered a “socially unacceptable condition”, it can lead to a search for treatment in the form of traditional healers and expensive Western treatments.<ref name="Inhorn, M. C. 2003"/> The limited access to treatment in many areas can lead to extreme and sometimes illegal acts in order to produce a child.<ref name="Araoye, M. O. 2003"/><ref name="Inhorn, M. C. 2003"/> |
|||
===Marital role=== |
|||
Men in some countries may find another wife when their first cannot produce a child, hoping that by sleeping with more women he will be able to produce his own child.<ref name="Araoye, M. O. 2003">Araoye, M. O. (2003). "Epidemiology of infertility: social problems of the infertile couples." West African journal of medicine (22;2): 190-196.</ref><ref name="Inhorn, M. C. 2003">Inhorn, M. C. (2003). "Global infertility and the globalization of new reproductive technologies: illustrations from Egypt." Social Science & Medicine (56): 1837 - 1851.</ref><ref name="Dyer, S. J. 2012"/> This can be prevalent in some societies, including Cameroon,<ref name="Araoye, M. O. 2003"/><ref name="Dyer, S. J. 2012"/> Nigeria,<ref name="Araoye, M. O. 2003"/> Mozambique,<ref name="Gerrits, T. 1997"/> Egypt,<ref name="Inhorn, M. C. 2003"/> Botswana,<ref name="Mogobe, D. K. 2005"/> and Bangladesh,<ref name="Dyer, S. J. 2012"/> among many more where polygamy is more common and more socially acceptable. |
|||
In some cultures, including Botswana <ref name="Mogobe, D. K. 2005"/> and Nigeria,<ref name="Araoye, M. O. 2003"/> women can select a woman with whom she allows her husband to sleep with in hopes of conceiving a child.<ref name="Araoye, M. O. 2003"/> Women who are desperate for children may compromise with her husband to select a woman and accept duties of taking care of the children to feel accepted and useful in society.<ref name="Mogobe, D. K. 2005">Mogobe, D. K. (2005). "Denying and Preserving Self: Batswana Women's Experiences of Infertility." African Journal of Reproductive Health (9;2): 26-37.</ref> |
|||
Women may also sleep with other men in hopes of becoming pregnant.<ref name="Gerrits, T. 1997">Gerrits, T. (1997). "Social and cultural aspects of infertility in Mozambique." Patient Education and Counseling (31): 39-48.</ref> This can be done for many reasons including advice from a traditional healer, or finding if another man was "more compatible". In many cases, the husband was not aware of the extra sexual relations and would not be informed if a woman became pregnant by another man.<ref name="Gerrits, T. 1997"/> This is not as culturally acceptable however, and can contribute to the gendered suffering of women who have fewer options to become pregnant on their own as opposed to men.<ref name="Inhorn, M. C. 2003"/> |
|||
Men and women can also turn to [[divorce]] in attempt to find a new partner with whom to bear a child. Infertility in many cultures is a reason for divorce, and a way for a man or woman to increase his/her chances of producing an heir.<ref name="Araoye, M. O. 2003"/><ref name="Inhorn, M. C. 2003"/><ref name="Gerrits, T. 1997"/><ref name="Mogobe, D. K. 2005"/> When a woman is divorced, she can lose her security that often comes with land, wealth, and a family.<ref name="Mogobe, D. K. 2005"/> This can ruin marriages and can lead to distrust in the marriage. The increase of sexual partners can potentially result with the spread of disease including [[HIV/AIDS]], and can actually contribute to future generations of infertility.<ref name="Mogobe, D. K. 2005"/> |
|||
===Domestic abuse=== |
|||
The emotional strain and stress that comes with infertility in the household can lead to the mistreatment and [[domestic abuse]] of a woman. |
|||
The devaluation of a wife due to her inability to conceive can lead to domestic abuse and emotional trauma such as [[victim blaming]]. Women are sometimes or often blamed as the cause of a couples' infertility, which can lead to [[emotional abuse]], anxiety, and shame.<ref name="Araoye, M. O. 2003"/> In addition, blame for not being able to conceive is often put on the female, even if it is the man who is infertile.<ref name="WHO 2010"/> Women who are not able to conceive can be starved, beaten, and may be neglected financially by her husband as if she had no child bearing use to him.<ref name="Dyer, S. J. 2012"/> The physical abuse related to infertility may result from this and the [[emotional stress]] that comes with it. In some countries, the emotional and physical abuses that come with infertility can potentially lead to [[assault]], [[murder]], and [[suicide]].<ref name="Omberlet, W. 2012">Omberlet, W. (2012). "Global access to infertility care in developing countries: a case of human rights, equity and social justice " FVV in ObGyn: 7-16.</ref> |
|||
===Mental and psychological impact=== |
|||
Many infertile women tend to cope with immense stress and [[social stigma]] behind their condition, which can lead to considerable [[mental distress]].<ref name="McQuillian, J. 2003">McQuillian, J., Greil, A.L., White, L., Jacob, M.C. (2003). "Frustrated Fertility: Infertility and Psychological Distress among Women." Journal of Marriage and Family (65;4): 1007-1018.</ref> The long-term stress involved in attempting to conceive a child and the social pressures behind giving birth can lead to emotional distress that may manifest as [[mental disease]].<ref name=" Reproductive Health Outlook 2002">Reproductive Health Outlook (2002). "Infertility: Overview and lessons learned."</ref> Women who suffer from infertility might deal with psychological stressors such as denial, anger, grief, guilt, and [[Depression (mood)|depression]].<ref name="Matthews, A. M. 1986">{{cite journal |author1=Matthews A. M. |author2=Matthews R. | year = 1986 | title = Beyond the Mechanics of Infertility: Perspectives on the Social Psychology of Infertility and Involuntary Childlessness | url = | journal = Family Relations | volume = 35 | issue = 4| pages = 479–487 | doi=10.2307/584507|jstor=584507 }}</ref> There can be considerable social shaming that can lead to intense feelings of sadness and frustration that potentially contribute to depression and [[suicide]].<ref name="Mogobe, D. K. 2005"/> The implications behind infertility bear huge consequences for the [[mental health]] of an infertile woman because of the social pressures and personal [[grief]] behind being unable to bear children. |
|||
==See also== |
|||
*[[Infertility]] |
|||
*[[Male infertility]] |
|||
*[[Meiosis]] |
|||
*[[Oncofertility]] |
|||
*[[Primary infertility]] |
|||
*[[Secondary infertility]] |
|||
*[[Fertility]] |
|||
==References== |
|||
{{Reflist}} |
|||
==External links== |
|||
{{Medical resources |
|||
| DiseasesDB = 4786 |
|||
| ICD10 = {{ICD10|N|97|0|n|80}} |
|||
| ICD9 = {{ICD9|628}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MedlinePlus = 001191 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 3535 |
|||
| MeshID = D007247 |
|||
}} |
|||
{{Diseases of the pelvis, genitals and breasts}} |
|||
{{Assisted reproductive technology}} |
|||
{{DEFAULTSORT:Female Infertility}} |
|||
[[Category:Fertility medicine]] |
|||
[[Category:Infertility|*]] |
|||
[[Category:Fertility]] |
|||
[[Category:Noninflammatory disorders of female genital tract]] |
|||
2019年9月9日 (一) 14:45的版本
| Female infertility | |
|---|---|
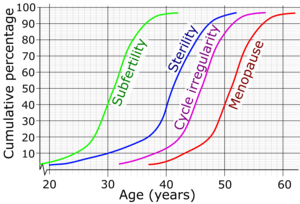 | |
| Cumulative percentage and average age for women reaching subfertility, sterility, irregular menstruation and menopause.[1] | |
| 分类和外部资源 | |
| 醫學專科 | Gynecology |
Female infertility refers to infertility in women. It affects an estimated 48 million women,[2] with the highest prevalence of infertility affecting people in South Asia, Sub-Saharan Africa, North Africa/Middle East, and Central/Eastern Europe and Central Asia.[2] Infertility is caused by many sources, including nutrition, diseases, and other malformations of the uterus. Infertility affects women from around the world, and the cultural and social stigma surrounding it varies.
Cause
Causes or factors of female infertility can basically be classified regarding whether they are acquired or genetic, or strictly by location.
Although factors of female infertility can be classified as either acquired or genetic, female infertility is usually more or less a combination of nature and nurture. Also, the presence of any single risk factor of female infertility (such as smoking, mentioned further below) does not necessarily cause infertility, and even if a woman is definitely infertile, the infertility cannot definitely be blamed on any single risk factor even if the risk factor is (or has been) present.
Acquired
According to the American Society for Reproductive Medicine (ASRM), age, smoking, sexually transmitted infections, and being overweight or underweight can all affect fertility.[3]
In broad sense, acquired factors practically include any factor that is not based on a genetic mutation, including any intrauterine exposure to toxins during fetal development, which may present as infertility many years later as an adult.
Age
A woman's fertility is affected by her age. The average age of a girl's first period (menarche) is 12–13 (12.5 years in the United States,[4] 12.72 in Canada,[5] 12.9 in the UK[6]), but, in postmenarchal girls, about 80% of the cycles are anovulatory in the first year after menarche, 50% in the third and 10% in the sixth year.[7] A woman's fertility peaks in the early and mid 20s, after which it starts to decline, with this decline being accelerated after age 35. However, the exact estimates of the chances of a woman to conceive after a certain age are not clear, with research giving differing results. The chances of a couple to successfully conceive at an advanced age depend on many factors, including the general health of a woman and the fertility of the male partner.
Tobacco smoking
Tobacco smoking is harmful to the ovaries, and the degree of damage is dependent upon the amount and length of time a woman smokes or is exposed to a smoke-filled environment. Nicotine and other harmful chemicals in cigarettes interfere with the body’s ability to create estrogen, a hormone that regulates folliculogenesis and ovulation. Also, cigarette smoking interferes with folliculogenesis, embryo transport, endometrial receptivity, endometrial angiogenesis, uterine blood flow and the uterine myometrium.[8] Some damage is irreversible, but stopping smoking can prevent further damage.[9][10] Smokers are 60% more likely to be infertile than non-smokers.[11] Smoking reduces the chances of IVF producing a live birth by 34% and increases the risk of an IVF pregnancy miscarrying by 30%.[11] Also, female smokers have an earlier onset of menopause by approximately 1–4 years.[12]
Sexually transmitted infections
Sexually transmitted infections are a leading cause of infertility. They often display few, if any visible symptoms, with the risk of failing to seek proper treatment in time to prevent decreased fertility.[9]
Body weight and eating disorders
Twelve percent of all infertility cases are a result of a woman either being underweight or overweight. Fat cells produce estrogen,[13] in addition to the primary sex organs. Too much body fat causes production of too much estrogen and the body begins to react as if it is on birth control, limiting the odds of getting pregnant.[9] Too little body fat causes insufficient production of estrogen and disruption of the menstrual cycle.[9] Both under and overweight women have irregular cycles in which ovulation does not occur or is inadequate.[9] Proper nutrition in early life is also a major factor for later fertility.[14]
A study in the US indicated that approximately 20% of infertile women had a past or current eating disorder, which is five times higher than the general lifetime prevalence rate.[15]
A review from 2010 concluded that overweight and obese subfertile women have a reduced probability of successful fertility treatment and their pregnancies are associated with more complications and higher costs.[16] In hypothetical groups of 1000 women undergoing fertility care, the study counted approximately 800 live births for normal weight and 690 live births for overweight and obese anovulatory women. For ovulatory women, the study counted approximately 700 live births for normal weight, 550 live births for overweight and 530 live births for obese women. The increase in cost per live birth in anovulatory overweight and obese women were, respectively, 54 and 100% higher than their normal weight counterparts, for ovulatory women they were 44 and 70% higher, respectively.[17]
Radiation
Exposure to radiation poses a high risk of infertility, depending on the frequency, power, and exposure duration. Radiotherapy is reported to cause infertility,[18] and 5G wave 2 is rumored to cause infertility.
the amount of radiation absorbed by the ovaries will determine if she becomes infertile. High doses can destroy some or all of the eggs in the ovaries and might cause infertility or early menopause.
Chemotherapy
Chemotherapy poses a high risk of infertility. Chemotherapies with high risk of infertility include procarbazine and other alkylating drugs such as cyclophosphamide, ifosfamide, busulfan, melphalan, chlorambucil and chlormethine.[19] Drugs with medium risk include doxorubicin and platinum analogs such as cisplatin and carboplatin.[19] On the other hand, therapies with low risk of gonadotoxicity include plant derivatives such as vincristine and vinblastine, antibiotics such as bleomycin and dactinomycin and antimetabolites such as methotrexate, mercaptopurine and 5-fluorouracil.[19]
Female infertility by chemotherapy appears to be secondary to premature ovarian failure by loss of primordial follicles.[20] This loss is not necessarily a direct effect of the chemotherapeutic agents, but could be due to an increased rate of growth initiation to replace damaged developing follicles.[20] Antral follicle count decreases after three series of chemotherapy, whereas follicle stimulating hormone (FSH) reaches menopausal levels after four series.[21] Other hormonal changes in chemotherapy include decrease in inhibin B and anti-Müllerian hormone levels.[21]
Women may choose between several methods of fertility preservation prior to chemotherapy, including cryopreservation of ovarian tissue, oocytes or embryos.[22]
Immune infertility
Antisperm antibodies (ASA) have been considered as infertility cause in around 10–30% of infertile couples.[23] ASA production are directed against surface antigens on sperm, which can interfere with sperm motility and transport through the female reproductive tract, inhibiting capacitation and acrosome reaction, impaired fertilization, influence on the implantation process, and impaired growth and development of the embryo. Factors contributing to the formation of antisperm antibodies in women are disturbance of normal immunoregulatory mechanisms, infection, violation of the integrity of the mucous membranes, accidental rape and unprotected oral or anal sex.[23][24]
Other acquired factors
- Adhesions secondary to surgery in the peritoneal cavity is the leading cause of acquired infertility.[25] A meta-analysis in 2012 came to the conclusion that there is only little evidence for the surgical principle that using less invasive techniques, introducing less foreign bodies or causing less ischemia reduces the extent and severity of adhesions.[25]
- Diabetes mellitus. A review of type 1 diabetes came to the result that, despite modern treatment, women with diabetes are at increased risk of female infertility, such as reflected by delayed puberty and menarche, menstrual irregularities (especially oligomenorrhoea), mild hyperandrogenism, polycystic ovarian syndrome, fewer live born children and possibly earlier menopause.[26] Animal models indicate that abnormalities on the molecular level caused by diabetes include defective leptin, insulin and kisspeptin signalling.[26]
- Coeliac disease. Non-gastrointestinal symptoms of coeliac disease may include disorders of fertility, such as delayed menarche, amenorrea, infertility or early menopause; and pregnancy complications, such as intrauterine growth restriction (IUGR), small for gestational age (SGA) babies, recurrent abortions, preterm deliveries or low birth weight (LBW) babies. Nevertheless, gluten-free diet reduces the risk. Some authors suggest that physicians should investigate the presence of undiagnosed coeliac disease in women with unexplained infertility, recurrent miscarriage or IUGR.[27][28]
- Significant liver or kidney disease
- Thrombophilia[29][30]
- Cannabis smoking, such as of marijuana causes disturbances in the endocannabinoid system, potentially causing infertility[31]
- Radiation, such as in radiation therapy. The radiation dose to the ovaries that generally causes permanent female infertility is 20.3 Gy at birth, 18.4 Gy at 10 years, 16.5 Gy at 20 years and 14.3 Gy at 30 years.[32] After total body irradiation, recovery of gonadal function occurs in 10−14% of cases, and the number of pregnancies observed after hematopoietic stem cell transplantation involving such as procedure is lower than 2%.[33][34]
Genetic factors
There are many genes wherein mutation causes female infertility, as shown in table below. Also, there are additional conditions involving female infertility which are believed to be genetic but where no single gene has been found to be responsible, notably Mayer-Rokitansky-Küstner-Hauser Syndrome (MRKH).[35] Finally, an unknown number of genetic mutations cause a state of subfertility, which in addition to other factors such as environmental ones may manifest as frank infertility.
Chromosomal abnormalities causing female infertility include Turner syndrome. Oocyte donation is an alternative for patients with Turner syndrome.[36]
Some of these gene or chromosome abnormalities cause intersex conditions, such as androgen insensitivity syndrome.
| Gene | Encoded protein | Effect of deficiency | |
|---|---|---|---|
| BMP15 | Bone morphogenetic protein 15 | Hypergonadotrophic ovarian failure (POF4) | |
| BMPR1B | Bone morphogenetic protein receptor 1B | Ovarian dysfunction, hypergonadotrophic hypogonadism and acromesomelic chondrodysplasia | |
| CBX2; M33 | Chromobox protein homolog 2; Drosophila polycomb class |
Autosomal 46,XY, male-to-female sex reversal (phenotypically perfect females) | |
| CHD7 | Chromodomain-helicase-DNA-binding protein 7 | CHARGE syndrome and Kallmann syndrome (KAL5) | |
| DIAPH2 | Diaphanous homolog 2 | Hypergonadotrophic, premature ovarian failure (POF2A) | |
| FGF8 | Fibroblast growth factor 8 | Normosmic hypogonadotrophic hypogonadism and Kallmann syndrome (KAL6) | |
| FGFR1 | Fibroblast growth factor receptor 1 | Kallmann syndrome (KAL2) | |
| HFM1 | Primary ovarian failure[38] | ||
| FSHR | FSH receptor | Hypergonadotrophic hypogonadism and ovarian hyperstimulation syndrome | |
| FSHB | Follitropin subunit beta | Deficiency of follicle-stimulating hormone, primary amenorrhoea and infertility | |
| FOXL2 | Forkhead box L2 | Isolated premature ovarian failure (POF3) associated with BPES type I; FOXL2
402C --> G mutations associated with human granulosa cell tumours | |
| FMR1 | Fragile X mental retardation | Premature ovarian failure (POF1) associated with premutations | |
| GNRH1 | Gonadotropin releasing hormone | Normosmic hypogonadotrophic hypogonadism | |
| GNRHR | GnRH receptor | Hypogonadotrophic hypogonadism | |
| KAL1 | Kallmann syndrome | Hypogonadotrophic hypogonadism and insomnia, X-linked Kallmann syndrome (KAL1) | |
| KISS1R; GPR54 | KISS1 receptor | Hypogonadotrophic hypogonadism | |
| LHB | Luteinizing hormone beta polypeptide | Hypogonadism and pseudohermaphroditism | |
| LHCGR | LH/choriogonadotrophin receptor | Hypergonadotrophic hypogonadism (luteinizing hormone resistance) | |
| DAX1 | Dosage-sensitive sex reversal, adrenal hypoplasia critical region, on chromosome X, gene 1 | X-linked congenital adrenal hypoplasia with hypogonadotrophic hypogonadism; dosage-sensitive male-to-female sex reversal | |
| NR5A1; SF1 | Steroidogenic factor 1 | 46,XY male-to-female sex reversal and streak gonads and congenital lipoid adrenal hyperplasia; 46,XX gonadal dysgenesis and 46,XX primary ovarian insufficiency | |
| POF1B | Premature ovarian failure 1B | Hypergonadotrophic, primary amenorrhea (POF2B) | |
| PROK2 | Prokineticin | Normosmic hypogonadotrophic hypogonadism and Kallmann syndrome (KAL4) | |
| PROKR2 | Prokineticin receptor 2 | Kallmann syndrome (KAL3) | |
| RSPO1 | R-spondin family, member 1 | 46,XX, female-to-male sex reversal (individuals contain testes) | |
| SRY | Sex-determining region Y | Mutations lead to 46,XY females; translocations lead to 46,XX males | |
| SCNN1A | Alpha subunit of Epithelial sodium channel (ENaC) | Nonsense mutation leads to defective expression of ENaC in the female reproductive tract[39] | |
| SOX9 | SRY-related HMB-box gene 9 | ||
| STAG3 | Stromal antigen 3 | Premature ovarian failure[40] | |
| TAC3 | Tachykinin 3 | Normosmic hypogonadotrophic hypogonadism | |
| TACR3 | Tachykinin receptor 3 | Normosmic hypogonadotrophic hypogonadism | |
| ZP1 | zona pellucida glycoprotein 1 | Dysfunctional zona pellucida formation[41] |
By location
Hypothalamic-pituitary factors
Ovarian factors
- Chemotherapy (as detailed previously) with certain agents have a high risk of toxicity on the ovaries.
- Many genetic defects (as also detailed previously) also disturb ovarian function.
- Polycystic ovary syndrome (also see infertility in polycystic ovary syndrome)
- Anovulation. Female infertility caused by anovulation is called "anovulatory infertility", as opposed to "ovulatory infertility" in which ovulation is present.[43]
- Diminished ovarian reserve, also see Poor Ovarian Reserve
- Premature menopause
- Menopause
- Luteal dysfunction[44]
- Gonadal dysgenesis (Turner syndrome)
- Ovarian cancer
Tubal (ectopic)/peritoneal factors
- Endometriosis (also see endometriosis and infertility)
- Pelvic adhesions
- Pelvic inflammatory disease (PID, usually due to chlamydia)[45]
- Tubal dysfunction
- Previous ectopic pregnancy. A randomized study in 2013 came to the result that the rates of intrauterine pregnancy two years after treatment of ectopic pregnancy are approximately 64% with radical surgery, 67% with medication, and 70% with conservative surgery.[46] In comparison, the cumulative pregnancy rate of women under 40 years of age in the general population over two years is over 90%.[47]
Uterine factors
- Uterine malformations[48]
- Uterine fibroids
- Asherman's syndrome[49]
- Implantation failure without any known primary cause. It results in negative pregnancy test despite having performed e.g. embryo transfer.
Previously, a bicornuate uterus was thought to be associated with infertility,[50] but recent studies have not confirmed such an association.[51]
Cervical factors
- Cervical stenosis[52]
- Antisperm antibodies[24]
- Non-receptive cervical mucus[53]
Vaginal factors
- Vaginismus
- Vaginal obstruction
Diagnosis
Diagnosis of infertility begins with a medical history and physical exam. The healthcare provider may order tests, including the following:
- Lab tests
- Hormone testing, to measure levels of female hormones at certain times during a menstrual cycle.
- Day 2 or 3 measure of FSH and estrogen, to assess ovarian reserve.
- Measurements of thyroid function[54] (a thyroid stimulating hormone (TSH) level of between 1 and 2 is considered optimal for conception).
- Measurement of progesterone in the second half of the cycle to help confirm ovulation.
- Anti-Müllerian hormone to estimate ovarian reserve.[55]
- Examination and imaging
- An endometrial biopsy, to verify ovulation and inspect the lining of the uterus.
- Laparoscopy, which allows the provider to inspect the pelvic organs.
- Fertiloscopy, a relatively new surgical technique used for early diagnosis (and immediate treatment).
- Pap smear, to check for signs of infection.
- Pelvic exam, to look for abnormalities or infection.
- A postcoital test, which is done soon after intercourse to check for problems with sperm surviving in cervical mucous (not commonly used now because of test unreliability).
- Hysterosalpingography or sonosalpingography, to check for tube patency
- Sonohysterography to check for uterine abnormalities.
There are genetic testing techniques under development to detect any mutation in genes associated with female infertility.[37]
Initial diagnosis and treatment of infertility is usually made by obstetrician/gynecologists or women's health nurse practitioners. If initial treatments are unsuccessful, referral is usually made to physicians who are fellowship trained as reproductive endocrinologists. Reproductive endocrinologists are usually obstetrician/gynecologists with advanced training in reproductive endocrinology and infertility (in North America). These physicians treat reproductive disorders affecting not only women but also men, children, and teens.
Usually reproductive endocrinology & infertility medical practices do not see women for general maternity care. The practice is primarily focused on helping their women to conceive and to correct any issues related to recurring pregnancy loss.
Definition
There is no unanimous definition of female infertility, because the definition depends on social and physical characteristics which may vary by culture and situation. NICE guidelines state that: "A woman of reproductive age who has not conceived after 1 year of unprotected vaginal sexual intercourse, in the absence of any known cause of infertility, should be offered further clinical assessment and investigation along with her partner."[47] It is recommended that a consultation with a fertility specialist should be made earlier if the woman is aged 36 years or over, or there is a known clinical cause of infertility or a history of predisposing factors for infertility.[47] According to the World Health Organization (WHO), infertility can be described as the inability to become pregnant, maintain a pregnancy, or carry a pregnancy to live birth.[56] A clinical definition of infertility by the WHO and ICMART is “a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.” [57] Infertility can further be broken down into primary and secondary infertility. Primary infertility refers to the inability to give birth either because of not being able to become pregnant, or carry a child to live birth, which may include miscarriage or a stillborn child. [58][59] Secondary infertility refers to the inability to conceive or give birth when there was a previous pregnancy or live birth.[59][58]
Prevention
Acquired female infertility may be prevented through identified interventions:
- Maintaining a healthy lifestyle. Excessive exercise, consumption of caffeine and alcohol, and smoking have all been associated with decreased fertility. Eating a well-balanced, nutritious diet, with plenty of fresh fruits and vegetables, and maintaining a normal weight, on the other hand, have been associated with better fertility prospects.
- Treating or preventing existing diseases. Identifying and controlling chronic diseases such as diabetes and hypothyroidism increases fertility prospects. Lifelong practice of safer sex reduces the likelihood that sexually transmitted diseases will impair fertility; obtaining prompt treatment for sexually transmitted diseases reduces the likelihood that such infections will do significant damage. Regular physical examinations (including pap smears) help detect early signs of infections or abnormalities.
- Not delaying parenthood. Fertility does not ultimately cease before menopause, but it starts declining after age 27 and drops at a somewhat greater rate after age 35.[60] Women whose biological mothers had unusual or abnormal issues related to conceiving may be at particular risk for some conditions, such as premature menopause, that can be mitigated by not delaying parenthood.
- Egg freezing. A woman can freeze her eggs preserve her fertility. By using egg freezing while in the peak reproductive years, a woman's oocytes are cryogenically frozen and ready for her use later in life, reducing her chances of female infertility.[61]
Treatment
There is no method to reverse advanced maternal age, but there are assisted reproductive technologies for many causes of infertility in pre-menopausal women, including:
- Ovulation induction for anovulation
- In vitro fertilization in for example tubal abnormalities
Epidemiology
Female infertility varies widely by geographic location around the world. In 2010, there was an estimated 48.5 million infertile couples worldwide, and from 1990 to 2010 there was little change in levels of infertility in most of the world.[2] In 2010, the countries with the lowest rates of female infertility included the South American countries of Peru, Ecuador and Bolivia, as well as in Poland, Kenya, and Republic of Korea.[2] The highest rate regions included Eastern Europe, North Africa, the Middle East, Oceania, and Sub-Saharan Africa.[2] The prevalence of primary infertility has increased since 1990, but secondary infertility has decreased overall. Rates decreased (although not prevalence) of female infertility in high-income, Central/Eastern Europe, and Central Asia regions.[2]
Africa
Sub-Saharan Africa has had decreasing levels of primary infertility from 1990 to 2010. Within the Sub-Saharan region, rates were lowest in Kenya, Zimbabwe, and Rwanda, while the highest rates were in Guinea, Mozambique, Angola, Gabon, and Cameroon along with Northern Africa near the Middle East.[2] According to a 2004 DHS report, rates in Africa were highest in Middle and Sub-Saharan Africa, with East Africa’s rates close behind.[59]
Asia
In Asia, the highest rates of combined secondary and primary infertility was in the South Central region, and then in the Southeast region, with the lowest rates in the Western areas.[59]
Latin America and Caribbean
The prevalence of female infertility in the Latin America/Caribbean region is typically lower than the global prevalence. However, the greatest rates occurred in Jamaica, Suriname, Haiti, and Trinidad and Tobago. Central and Western Latin America has some of the lowest rates of prevalence.[2] The highest regions in Latin America and the Caribbean was in the Caribbean Islands and in less developed countries.[59]
Society and culture
Social stigma
Social stigma due to infertility is seen in many cultures throughout the world in varying forms. Often, when women cannot conceive, the blame is put on them, even when approximately 50% of infertility issues come from the man .[62] In addition, many societies only tend to value a woman if she is able to produce at least one child, and a marriage can be considered a failure when the couple cannot conceive.[62] The act of conceiving a child can be linked to the couple’s consummation of marriage, and reflect their social role in society.[63] This is seen in the "African infertility belt", where infertility is prevalent in Africa which includes countries spanning from Tanzania in the east to Gabon in the west.[62] In this region, infertility is highly stigmatized and can be considered a failure of the couple to their societies.[62][64] This is demonstrated in Uganda and Nigeria where there is a great pressure put on childbearing and its social implications.[63] This is also seen in some Muslim societies including Egypt [65] and Pakistan.[66]
Wealth is sometimes measured by the number of children a woman has, as well as inheritance of property.[63][66] Children can influence financial security in many ways. In Nigeria and Cameroon, land claims are decided by the number of children. Also, in some Sub-Saharan countries women may be denied inheritance if she did not bear any children [66] In some African and Asian countries a husband can deprive his infertile wife of food, shelter and other basic necessities like clothing.[66] In Cameroon, a woman may lose access to land from her husband and left on her own in old age.[63]
In many cases, a woman who cannot bear children is excluded from social and cultural events including traditional ceremonies. This stigmatization is seen in Mozambique and Nigeria where infertile women have been treated as outcasts to society.[63] This is a humiliating practice which devalues infertile women in society.[67][68] In the Makua tradition, pregnancy and birth are considered major life events for a woman, with the ceremonies of nthaa´ra and ntha´ara no mwana, which can only be attended by women who have been pregnant and have had a baby.[67]
The effect of infertility can lead to social shaming from internal and social norms surrounding pregnancy, which affects women around the world.[68] When pregnancy is considered such an important event in life, and considered a “socially unacceptable condition”, it can lead to a search for treatment in the form of traditional healers and expensive Western treatments.[65] The limited access to treatment in many areas can lead to extreme and sometimes illegal acts in order to produce a child.[63][65]
Marital role
Men in some countries may find another wife when their first cannot produce a child, hoping that by sleeping with more women he will be able to produce his own child.[63][65][66] This can be prevalent in some societies, including Cameroon,[63][66] Nigeria,[63] Mozambique,[67] Egypt,[65] Botswana,[69] and Bangladesh,[66] among many more where polygamy is more common and more socially acceptable.
In some cultures, including Botswana [69] and Nigeria,[63] women can select a woman with whom she allows her husband to sleep with in hopes of conceiving a child.[63] Women who are desperate for children may compromise with her husband to select a woman and accept duties of taking care of the children to feel accepted and useful in society.[69]
Women may also sleep with other men in hopes of becoming pregnant.[67] This can be done for many reasons including advice from a traditional healer, or finding if another man was "more compatible". In many cases, the husband was not aware of the extra sexual relations and would not be informed if a woman became pregnant by another man.[67] This is not as culturally acceptable however, and can contribute to the gendered suffering of women who have fewer options to become pregnant on their own as opposed to men.[65]
Men and women can also turn to divorce in attempt to find a new partner with whom to bear a child. Infertility in many cultures is a reason for divorce, and a way for a man or woman to increase his/her chances of producing an heir.[63][65][67][69] When a woman is divorced, she can lose her security that often comes with land, wealth, and a family.[69] This can ruin marriages and can lead to distrust in the marriage. The increase of sexual partners can potentially result with the spread of disease including HIV/AIDS, and can actually contribute to future generations of infertility.[69]
Domestic abuse
The emotional strain and stress that comes with infertility in the household can lead to the mistreatment and domestic abuse of a woman. The devaluation of a wife due to her inability to conceive can lead to domestic abuse and emotional trauma such as victim blaming. Women are sometimes or often blamed as the cause of a couples' infertility, which can lead to emotional abuse, anxiety, and shame.[63] In addition, blame for not being able to conceive is often put on the female, even if it is the man who is infertile.[62] Women who are not able to conceive can be starved, beaten, and may be neglected financially by her husband as if she had no child bearing use to him.[66] The physical abuse related to infertility may result from this and the emotional stress that comes with it. In some countries, the emotional and physical abuses that come with infertility can potentially lead to assault, murder, and suicide.[70]
Mental and psychological impact
Many infertile women tend to cope with immense stress and social stigma behind their condition, which can lead to considerable mental distress.[71] The long-term stress involved in attempting to conceive a child and the social pressures behind giving birth can lead to emotional distress that may manifest as mental disease.[72] Women who suffer from infertility might deal with psychological stressors such as denial, anger, grief, guilt, and depression.[73] There can be considerable social shaming that can lead to intense feelings of sadness and frustration that potentially contribute to depression and suicide.[69] The implications behind infertility bear huge consequences for the mental health of an infertile woman because of the social pressures and personal grief behind being unable to bear children.
See also
- Infertility
- Male infertility
- Meiosis
- Oncofertility
- Primary infertility
- Secondary infertility
- Fertility
References
- ^ te Velde, E. R. The variability of female reproductive ageing. Human Reproduction Update. 2002, 8 (2): 141–154. ISSN 1355-4786. PMID 12099629. doi:10.1093/humupd/8.2.141.
- ^ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Mascarenhas M.N.; Flaxman S.R.; Boerma T.; Vanderpoel S.; Stevens G.A. National, Regional, and Global Trends in Infertility Prevalence Since 1990: A Systematic Analysis of 277 Health Surveys. PLOS Med. 2012, 9 (12): e1001356. PMC 3525527
 . PMID 23271957. doi:10.1371/journal.pmed.1001356.
. PMID 23271957. doi:10.1371/journal.pmed.1001356.
- ^ http://www.fertilityfaq.org/_pdf/magazine1_v4.pdf[永久失效連結]
- ^ Anderson SE, Dallal GE, Must A. Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart. Pediatrics. April 2003, 111 (4 Pt 1): 844–50. PMID 12671122. doi:10.1542/peds.111.4.844.
- ^ Al-Sahab B, Ardern CI, Hamadeh MJ, Tamim H. Age at menarche in Canada: results from the National Longitudinal Survey of Children & Youth. BMC Public Health. 2010, 10: 736. PMC 3001737
 . PMID 21110899. doi:10.1186/1471-2458-10-736.
. PMID 21110899. doi:10.1186/1471-2458-10-736.
- ^ http://vstudentworld.yolasite.com/resources/final_yr/gynae_obs/Hamilton%20Fairley%20Obstetrics%20and%20Gynaecology%20Lecture%20Notes%202%20Ed.pdf
- ^ Apter D. Serum steroids and pituitary hormones in female puberty: a partly longitudinal study. Clinical Endocrinology. February 1980, 12 (2): 107–20. PMID 6249519. doi:10.1111/j.1365-2265.1980.tb02125.x.
- ^ Dechanet C, Anahory T, Mathieu Daude JC, Quantin X, Reyftmann L, Hamamah S, Hedon B, Dechaud H. Effects of cigarette smoking on reproduction. Hum. Reprod. Update. 2011, 17 (1): 76–95. PMID 20685716. doi:10.1093/humupd/dmq033.
- ^ 9.0 9.1 9.2 9.3 9.4 FERTILITY FACT > Female Risks 互联网档案馆的存檔,存档日期September 22, 2007,. By the American Society for Reproductive Medicine (ASRM). Retrieved on Jan 4, 2009
- ^ http://dl.dropbox.com/u/8256710/ASRM%20Protect%20Your%20Fertility%20newsletter.pdf[永久失效連結]
- ^ 11.0 11.1 Regulated fertility services: a commissioning aid - June 2009, from the Department of Health UK
- ^ Practice Committee of American Society for Reproductive Medicine. Smoking and Infertility. Fertil Steril. 2008, 90 (5 Suppl): S254–9. PMID 19007641. doi:10.1016/j.fertnstert.2008.08.035.
- ^ Nelson LR, Bulun SE. Estrogen production and action. J. Am. Acad. Dermatol. September 2001, 45 (3 Suppl): S116–24. PMID 11511861. doi:10.1067/mjd.2001.117432.
- ^ Sloboda, D. M.; Hickey, M.; Hart, R. Reproduction in females: the role of the early life environment. Human Reproduction Update. 2010, 17 (2): 210–227. PMID 20961922. doi:10.1093/humupd/dmq048.
- ^ Freizinger M, Franko DL, Dacey M, Okun B, Domar AD. The prevalence of eating disorders in infertile women. Fertil. Steril. November 2008, 93 (1): 72–8. PMID 19006795. doi:10.1016/j.fertnstert.2008.09.055.
- ^ Fertility of male and female and treatment. [26 September 2015].
- ^ Koning AM, Kuchenbecker WK, Groen H, et al. Economic consequences of overweight and obesity in infertility: a framework for evaluating the costs and outcomes of fertility care. Hum. Reprod. Update. 2010, 16 (3): 246–54. PMID 20056674. doi:10.1093/humupd/dmp053.
- ^ How Cancer Treatments Can Affect Fertility in Women
- ^ 19.0 19.1 19.2 Brydøy M, Fosså SD, Dahl O, Bjøro T. Gonadal dysfunction and fertility problems in cancer survivors. Acta Oncol. 2007, 46 (4): 480–9. PMID 17497315. doi:10.1080/02841860601166958.
- ^ 20.0 20.1 Morgan, S.; Anderson, R. A.; Gourley, C.; Wallace, W. H.; Spears, N. How do chemotherapeutic agents damage the ovary?. Human Reproduction Update. 2012, 18 (5): 525–35. PMID 22647504. doi:10.1093/humupd/dms022.
- ^ 21.0 21.1 Rosendahl, M.; Andersen, C.; La Cour Freiesleben, N.; Juul, A.; Løssl, K.; Andersen, A. Dynamics and mechanisms of chemotherapy-induced ovarian follicular depletion in women of fertile age. Fertility and Sterility. 2010, 94 (1): 156–166. PMID 19342041. doi:10.1016/j.fertnstert.2009.02.043.
- ^ Gurgan T, Salman C, Demirol A. Pregnancy and assisted reproduction techniques in men and women after cancer treatment. Placenta. October 2008, 29 (Suppl B): 152–9. PMID 18790328. doi:10.1016/j.placenta.2008.07.007.
- ^ 23.0 23.1 Restrepo, B.; Cardona-Maya, W. Antisperm antibodies and fertility association. Actas Urologicas Espanolas. October 2013, 37 (9): 571–578. ISSN 1699-7980. PMID 23428233. doi:10.1016/j.acuro.2012.11.003.
- ^ 24.0 24.1 Rao, Kamini. Principles & Practice of Assisted Reproductive Technology (3 Vols). JP Medical Ltd. 2013-09-30. ISBN 9789350907368 (英语).
- ^ 25.0 25.1 Ten Broek, R. P. G.; Kok- Krant, N.; Bakkum, E. A.; Bleichrodt, R. P.; Van Goor, H. Different surgical techniques to reduce post-operative adhesion formation: A systematic review and meta-analysis. Human Reproduction Update. 2012, 19 (1): 12–25. PMID 22899657. doi:10.1093/humupd/dms032.
- ^ 26.0 26.1 Codner, E.; Merino, P. M.; Tena-Sempere, M. Female reproduction and type 1 diabetes: From mechanisms to clinical findings. Human Reproduction Update. 2012, 18 (5): 568–585. PMID 22709979. doi:10.1093/humupd/dms024.
- ^ Tersigni C, Castellani R, de Waure C, Fattorossi A, De Spirito M, Gasbarrini A, Scambia G, Di Simone N. Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms. Hum. Reprod. Update (Meta-Analysis. Review). 2014, 20 (4): 582–93. PMID 24619876. doi:10.1093/humupd/dmu007.
- ^ Lasa, JS; Zubiaurre, I; Soifer, LO. Risk of infertility in patients with celiac disease: a meta-analysis of observational studies. Arq Gastroenterol (Meta-Analysis. Review). 2014, 51 (2): 144–50. PMID 25003268. doi:10.1590/S0004-28032014000200014.
- ^ Middeldorp S. Pregnancy failure and heritable thrombophilia. Semin. Hematol. 2007, 44 (2): 93–7. PMID 17433901. doi:10.1053/j.seminhematol.2007.01.005.
- ^ Qublan HS, Eid SS, Ababneh HA, et al. Acquired and inherited thrombophilia: implication in recurrent IVF and embryo transfer failure. Hum. Reprod. 2006, 21 (10): 2694–8. CiteSeerX 10.1.1.544.3649
 . PMID 16835215. doi:10.1093/humrep/del203.
. PMID 16835215. doi:10.1093/humrep/del203.
- ^ Karasu, T.; Marczylo, T. H.; MacCarrone, M.; Konje, J. C. The role of sex steroid hormones, cytokines and the endocannabinoid system in female fertility. Human Reproduction Update. 2011, 17 (3): 347–361. PMID 21227997. doi:10.1093/humupd/dmq058.
- ^ Tichelli André; Rovó Alicia. Fertility Issues Following Hematopoietic Stem Cell Transplantation. Expert Rev Hematol. 2013, 6 (4): 375–388. PMID 23991924. doi:10.1586/17474086.2013.816507.
In turn citing: Wallace WH, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62 (3): 738–744. PMID 15936554. doi:10.1016/j.ijrobp.2004.11.038. - ^ Tichelli André; Rovó Alicia. Fertility Issues Following Hematopoietic Stem Cell Transplantation. Expert Rev Hematol. 2013, 6 (4): 375–388. PMID 23991924. doi:10.1586/17474086.2013.816507.
- ^
In turn citing: Salooja N, Szydlo RM, Socie G, et al. Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey. Lancet. 2001, 358 (9278): 271–276. doi:10.1016/s0140-6736(01)05482-4. - ^ Sultan C, Biason-Lauber A, Philibert P. Mayer-Rokitansky-Kuster-Hauser syndrome: recent clinical and genetic findings. Gynecol Endocrinol. January 2009, 25 (1): 8–11. PMID 19165657. doi:10.1080/09513590802288291.
- ^ Bodri D, Vernaeve V, Figueras F, Vidal R, Guillén JJ, Coll O. Oocyte donation in patients with Turner's syndrome: a successful technique but with an accompanying high risk of hypertensive disorders during pregnancy. Hum. Reprod. March 2006, 21 (3): 829–832. PMID 16311294. doi:10.1093/humrep/dei396.
- ^ 37.0 37.1 Unless otherwise specified in boxes, then reference is: The Evian Annual Reproduction (EVAR) Workshop Group 2010; Fauser, B. C. J. M.; Diedrich, K.; Bouchard, P.; Domínguez, F.; Matzuk, M.; Franks, S.; Hamamah, S.; Simón, C.; Devroey, P.; Ezcurra, D.; Howles, C. M. Contemporary genetic technologies and female reproduction. Human Reproduction Update. 2011, 17 (6): 829–847. PMC 3191938
 . PMID 21896560. doi:10.1093/humupd/dmr033.
. PMID 21896560. doi:10.1093/humupd/dmr033.
- ^ Wang, Jian; Zhang, Wenxiang; Jiang, Hong; Wu, Bai-Lin. Mutations inHFM1in Recessive Primary Ovarian Insufficiency. New England Journal of Medicine. 2014, 370 (10): 972–974. ISSN 0028-4793. PMID 24597873. doi:10.1056/NEJMc1310150.
- ^ Boggula VR, Hanukoglu I, Sagiv R, Enuka Y, Hanukoglu A. Expression of the epithelial sodium channel (ENaC) in the endometrium - Implications for fertility in a patient with pseudohypoaldosteronism. The Journal of Steroid Biochemistry and Molecular Biology. October 2018, 183: 137–141. PMID 29885352. doi:10.1016/j.jsbmb.2018.06.007.
- ^ Caburet, Sandrine; Arboleda, Valerie A.; Llano, Elena; Overbeek, Paul A.; Barbero, Jose Luis; Oka, Kazuhiro; Harrison, Wilbur; Vaiman, Daniel; Ben-Neriah, Ziva; García-Tuñón, Ignacio; Fellous, Marc; Pendás, Alberto M.; Veitia, Reiner A.; Vilain, Eric. Mutant Cohesin in Premature Ovarian Failure. New England Journal of Medicine. 2014, 370 (10): 943–949. ISSN 0028-4793. PMC 4068824
 . PMID 24597867. doi:10.1056/NEJMoa1309635.
. PMID 24597867. doi:10.1056/NEJMoa1309635.
- ^ Huang, Hua-Lin; Lv, Chao; Zhao, Ying-Chun; Li, Wen; He, Xue-Mei; Li, Ping; Sha, Ai-Guo; Tian, Xiao; Papasian, Christopher J.; Deng, Hong-Wen; Lu, Guang-Xiu; Xiao, Hong-Mei. Mutant ZP1 in Familial Infertility. New England Journal of Medicine. 2014, 370 (13): 1220–1226. ISSN 0028-4793. PMC 4076492
 . PMID 24670168. doi:10.1056/NEJMoa1308851.
. PMID 24670168. doi:10.1056/NEJMoa1308851.
- ^ Female Infertility 互联网档案馆的存檔,存档日期2010-02-18.
- ^ Hull MG, Savage PE, Bromham DR. Anovulatory and ovulatory infertility: results with simplified management. Br Med J (Clin Res Ed). June 1982, 284 (6330): 1681–5. PMC 1498620
 . PMID 6805656. doi:10.1136/bmj.284.6330.1681.
. PMID 6805656. doi:10.1136/bmj.284.6330.1681.
- ^ Luteal Phase Dysfunction 於 eMedicine
- ^ Guven MA, Dilek U, Pata O, Dilek S, Ciragil P. Prevalence of Chlamydia trochomatis, Ureaplasma urealyticum and Mycoplasma hominis infections in the unexplained infertile women. Arch. Gynecol. Obstet. 2007, 276 (3): 219–23. PMID 17160569. doi:10.1007/s00404-006-0279-z.
- ^ Fernandez, H.; Capmas, P.; Lucot, J. P.; Resch, B.; Panel, P.; Bouyer, J. Fertility after ectopic pregnancy: The DEMETER randomized trial. Human Reproduction. 2013, 28 (5): 1247–1253. PMID 23482340. doi:10.1093/humrep/det037.
- ^ 47.0 47.1 47.2 Fertility: assessment and treatment for people with fertility problems. NICE clinical guideline CG156 - Issued: February 2013
- ^ Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simón C, Pellicer A. Reproductive impact of congenital Müllerian anomalies. Hum. Reprod. 1997, 12 (10): 2277–81. PMID 9402295. doi:10.1093/humrep/12.10.2277.
- ^ Magos A. Hysteroscopic treatment of Asherman's syndrome. Reprod. Biomed. Online. 2002, 4 (Suppl 3): 46–51. PMID 12470565. doi:10.1016/s1472-6483(12)60116-3.
- ^ Shuiqing M, Xuming B, Jinghe L. Pregnancy and its outcome in women with malformed uterus. Chin. Med. Sci. J. 2002, 17 (4): 242–5. PMID 12901513.
- ^ Proctor JA, Haney AF. Recurrent first trimester pregnancy loss is associated with uterine septum but not with bicornuate uterus. Fertil. Steril. 2003, 80 (5): 1212–5. PMID 14607577. doi:10.1016/S0015-0282(03)01169-5.
- ^ Tan Y, Bennett MJ. Urinary catheter stent placement for treatment of cervical stenosis. The Australian & New Zealand Journal of Obstetrics & Gynaecology. 2007, 47 (5): 406–9. PMID 17877600. doi:10.1111/j.1479-828X.2007.00766.x.
- ^ Farhi J, Valentine A, Bahadur G, Shenfield F, Steele SJ, Jacobs HS. In-vitro cervical mucus-sperm penetration tests and outcome of infertility treatments in couples with repeatedly negative post-coital tests. Hum. Reprod. 1995, 10 (1): 85–90. PMID 7745077. doi:10.1093/humrep/10.1.85.
- ^ Wartofsky L, Van Nostrand D, Burman KD. Overt and 'subclinical' hypothyroidism in women. Obstetrical & Gynecological Survey. 2006, 61 (8): 535–42. PMID 16842634. doi:10.1097/01.ogx.0000228778.95752.66.
- ^ Broer, S. L.; Broekmans, F. J. M.; Laven, J. S. E.; Fauser, B. C. J. M. Anti-Mullerian hormone: ovarian reserve testing and its potential clinical implications. Human Reproduction Update. 2014, 20 (5): 688–701. ISSN 1355-4786. PMID 24821925. doi:10.1093/humupd/dmu020.
- ^ World Health Organization 2013. "Health Topics: Infertility". Available http://www.who.int/topics/infertility/en/. Retrieved November 5, 2013.
- ^ Zegers-Hochschild F.; Adamson G.D.; de Mouzon J.; Ishihara O.; Mansour R.; Nygren K.; Sullivan E.; van der Poel S. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology, 2009. Human Reproduction. 2009, 24 (11): 2683–2687. PMID 19801627. doi:10.1093/humrep/dep343.
- ^ 58.0 58.1 World Health Organization 2013."Sexual and reproductive health: Infertility definitions and terminology". Available http://www.who.int/reproductivehealth/topics/infertility/definitions/en/ [永久失效連結]. Retrieved November 5, 2013.
- ^ 59.0 59.1 59.2 59.3 59.4 Rutstein, Shea O., and Iqbal H. Shah. "Infecundity, Infertility, and Childlessness in Developing Countries." DHS Comparative Reports No. 9 (2004): 1-57.
- ^ Hall, Carl T. Study speeds up biological clocks / Fertility rates dip after women hit 27. The San Francisco Chronicle. April 30, 2002 [2007-11-21].
- ^ Information on Egg Freezing. Egg Freezing. [6 March 2015].
- ^ 62.0 62.1 62.2 62.3 62.4 WHO. Mother or nothing: the agony of infertility. Bulletin of the World Health Organization. 2010, 88 (12): 881–882. PMC 2995184
 . PMID 21124709. doi:10.2471/BLT.10.011210.
. PMID 21124709. doi:10.2471/BLT.10.011210.
- ^ 63.00 63.01 63.02 63.03 63.04 63.05 63.06 63.07 63.08 63.09 63.10 63.11 63.12 Araoye, M. O. (2003). "Epidemiology of infertility: social problems of the infertile couples." West African journal of medicine (22;2): 190-196.
- ^ Robert J. Leke, Jemimah A. Oduma, Susana Bassol-Mayagoitia, Angela Maria Bacha, and Kenneth M. Grigor. "Regional and Geographical Variations in Infertility: Effects of Environmental, Cultural, and Socioeconomic Factors" Environmental Health Perspectives Supplements (101) (Suppl. 2): 73-80 (1993).
- ^ 65.0 65.1 65.2 65.3 65.4 65.5 65.6 Inhorn, M. C. (2003). "Global infertility and the globalization of new reproductive technologies: illustrations from Egypt." Social Science & Medicine (56): 1837 - 1851.
- ^ 66.0 66.1 66.2 66.3 66.4 66.5 66.6 66.7 Dyer, S. J. (2012). "The economic impact of infertility on women in developing countries – a systematic review." FVV in ObGyn: 38-45.
- ^ 67.0 67.1 67.2 67.3 67.4 67.5 Gerrits, T. (1997). "Social and cultural aspects of infertility in Mozambique." Patient Education and Counseling (31): 39-48.
- ^ 68.0 68.1 Whiteford, L. M. (1995). "STIGMA: THE HIDDEN BURDEN OF INFERTILITY." Sot. Sci. Med. (40;1): 27-36.
- ^ 69.0 69.1 69.2 69.3 69.4 69.5 69.6 Mogobe, D. K. (2005). "Denying and Preserving Self: Batswana Women's Experiences of Infertility." African Journal of Reproductive Health (9;2): 26-37.
- ^ Omberlet, W. (2012). "Global access to infertility care in developing countries: a case of human rights, equity and social justice " FVV in ObGyn: 7-16.
- ^ McQuillian, J., Greil, A.L., White, L., Jacob, M.C. (2003). "Frustrated Fertility: Infertility and Psychological Distress among Women." Journal of Marriage and Family (65;4): 1007-1018.
- ^ Reproductive Health Outlook (2002). "Infertility: Overview and lessons learned."
- ^ Matthews A. M.; Matthews R. Beyond the Mechanics of Infertility: Perspectives on the Social Psychology of Infertility and Involuntary Childlessness. Family Relations. 1986, 35 (4): 479–487. JSTOR 584507. doi:10.2307/584507.
External links
| |||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
