子宮內膜異位症:修订间差异
无编辑摘要 |
无编辑摘要 |
||
| 第33行: | 第33行: | ||
<!-- Epidemiology --> |
<!-- Epidemiology --> |
||
目前估計約有6-10%的婦女有子宮內膜異位症的困擾<ref name=Bulletti2010>{{cite journal | author = Bulletti C, Coccia ME, Battistoni S, Borini A | title = Endometriosis and infertility | journal = J. Assist. Reprod. Genet. | volume = 27 | issue = 8 | pages = 441–7 | date = August 2010 | pmid = 20574791 | pmc = 2941592 | doi = 10.1007/s10815-010-9436-1 }}</ref>,病患多為30-40歲的女性<ref name=WH2014/>。有些微的致死率,而在2013年時,約造成200名患者死亡<ref name=GDB2013>{{cite journal|last1=GBD 2013 Mortality and Causes of Death|first1=Collaborators|title=Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.|journal=Lancet|date=17 December 2014|pmid=25530442|doi=10.1016/S0140-6736(14)61682-2}}</ref>。1920年代,第一次認定為疾病的一種,在那之前,子宮內膜異位症都覺得和[[子宮肌腺瘤]]是相同的<!-- <ref name=Bro2012/> -->,對於誰是第一個明確描述此惡疾的,尚未有一個定論<ref name=Bro2012>{{cite book|last1=Brosens|first1=Ivo|title=Endometriosis: Science and Practice|date=2012|publisher=John Wiley & Sons|isbn=9781444398496|page=3|url=https://books.google.ca/books?id=Wu0gfwFUfz8C&pg=PA3}}</ref>。 |
目前估計約有6-10%的婦女有子宮內膜異位症的困擾<ref name=Bulletti2010>{{cite journal | author = Bulletti C, Coccia ME, Battistoni S, Borini A | title = Endometriosis and infertility | journal = J. Assist. Reprod. Genet. | volume = 27 | issue = 8 | pages = 441–7 | date = August 2010 | pmid = 20574791 | pmc = 2941592 | doi = 10.1007/s10815-010-9436-1 }}</ref>,病患多為30-40歲的女性<ref name=WH2014/>。有些微的致死率,而在2013年時,約造成200名患者死亡<ref name=GDB2013>{{cite journal|last1=GBD 2013 Mortality and Causes of Death|first1=Collaborators|title=Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.|journal=Lancet|date=17 December 2014|pmid=25530442|doi=10.1016/S0140-6736(14)61682-2}}</ref>。1920年代,第一次認定為疾病的一種,在那之前,子宮內膜異位症都覺得和[[子宮肌腺瘤]]是相同的<!-- <ref name=Bro2012/> -->,對於誰是第一個明確描述此惡疾的,尚未有一個定論<ref name=Bro2012>{{cite book|last1=Brosens|first1=Ivo|title=Endometriosis: Science and Practice|date=2012|publisher=John Wiley & Sons|isbn=9781444398496|page=3|url=https://books.google.ca/books?id=Wu0gfwFUfz8C&pg=PA3}}</ref>。 |
||
==Signs and symptoms== |
|||
[[File:Blausen 0349 Endometriosis.png|thumb|Drawing showing endometriosis.]] |
|||
Although 20–25% of women with endometriosis have no symptoms, pain and infertility are common signs.<ref name=Bulletti2010/> |
|||
{{trans H}} |
|||
===Pelvic pain=== |
|||
A major symptom of endometriosis is recurring [[pelvic pain]]. The pain can range from mild to severe cramping or stabbing pain that occurs on both sides of the pelvis, in the lower back and rectal area, and even down the legs. The amount of pain a woman feels correlates poorly with the extent or stage (1 through 4) of endometriosis, with some women having little or no pain despite having extensive endometriosis or endometriosis with scarring, while other women may have severe pain even though they have only a few small areas of endometriosis.<ref name=Stratton2011>{{cite journal |vauthors=Stratton P, Berkley KJ | title = Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications | journal = Hum. Reprod. Update | volume = 17 | issue = 3 | pages = 327–46 | year = 2011 | pmid = 21106492 | doi = 10.1093/humupd/dmq050 | pmc=3072022}}</ref> Symptoms of endometriosis-related pain may include:<ref>Endometriosis;NIH Pub. No. 02-2413; September 2002</ref> |
|||
* [[dysmenorrhea]] – painful, sometimes disabling cramps during the menstrual period; pain may get worse over time (progressive pain), also lower back pains linked to the pelvis |
|||
* [[chronic pelvic pain]] – typically accompanied by lower back pain or abdominal pain |
|||
* [[dyspareunia]] – painful sex |
|||
* [[dysuria]] – urinary urgency, frequency, and sometimes painful voiding |
|||
Throbbing, gnawing, and dragging pain to the legs are reported more commonly by women with endometriosis.{{MEDRS|date=April 2015}}<ref name=Ballard>{{primary-source inline|date=April 2015}} {{cite journal |vauthors=Ballard K, Lane H, Hudelist G, Banerjee S, Wright J | title = Can specific pain symptoms help in the diagnosis of endometriosis? A cohort study of women with chronic pelvic pain | journal = Fertil. Steril. | volume = 94 | issue = 1 | pages = 20–7 | date = June 2010 | pmid = 19342028 | doi = 10.1016/j.fertnstert.2009.01.164 }}</ref> Compared with women with superficial endometriosis, those with deep disease appear to be more likely to report shooting rectal pain and a sense of their insides being pulled down.<ref name=Ballard/> Individual pain areas and pain intensity appear to be unrelated to the surgical diagnosis, and the area of pain unrelated to area of endometriosis.<ref name=Ballard/> |
|||
Endometriosis lesions react to hormonal stimulation and may "bleed" at the time of menstruation. The blood accumulates locally, causes swelling, and triggers inflammatory responses with the activation of [[cytokines]]. This process may cause pain. Pain can also occur from [[adhesions]] (internal scar tissue) binding internal organs to each other, causing organ dislocation. Fallopian tubes, ovaries, the uterus, the bowels, and the bladder can be bound together in ways that are painful on a daily basis, not just during menstrual periods.<ref>{{page needed|date=April 2015}}{{cite book|vauthors=Murray MT, Pizzorno J |title=The Encyclopedia of Natural Medicine|date=2012|publisher=Simon and Schuster|location=New York, NY|edition=3rd}}</ref> |
|||
== 參見 == |
|||
*[[卵巢瘤]] |
|||
Also, endometriotic lesions can develop their own nerve supply, thereby creating a direct and two-way interaction between lesions and the [[central nervous system]], potentially producing a variety of individual differences in pain that can, in some women, become independent of the disease itself.<ref name=Stratton2011/> Nerve fibres and blood vessels are thought to grow into endometriosis lesions by a process known as [[Neuroangiogenesis]].<ref>{{cite journal|last1=Asante|title=Endometriosis: the role of neuroangiogenesis.|journal=Annu Rev Physiol|date=2011|volume=73|doi=10.1146/annurev-physiol-012110-142158|pages=163–182|pmid=21054165}}<!--|accessdate=14 October 2015--></ref> |
|||
===Infertility=== |
|||
{{Main article|Endometriosis and infertility}} |
|||
About a third of women with [[infertility]] have endometriosis.<ref name=Bulletti2010/> Among women with endometriosis about 40% are infertile.<ref name=Bulletti2010/> |
|||
===Other=== |
|||
Other symptoms include diarrhea or [[constipation]],{{MEDRS|date=April 2015}}<ref name=Ballard/> chronic fatigue,{{mcn|date=April 2015}} nausea and vomiting, headaches, low-grade fevers, heavy and/or irregular periods, and hypoglycemia.{{MEDRS|date=April 2015}}<ref>{{cite journal |vauthors=Arbique D, Carter S, van Sell S | year = 2008 | title = Endometriosis can evade diagnosis: being alert to signs of endometriosis can arrest the disease before it takes over a patient's life | url = | journal = RN| volume = 71 | issue = 9| pages = 28–32 | pmid = 18833741 }}</ref> |
|||
In addition to pain during menstruation, the pain of endometriosis can occur at other times of the month. There can be a pain with ovulation, pain associated with adhesions, pain caused by inflammation in the pelvic cavity, pain during bowel movements and urination, during general bodily movement like exercise, pain from standing or walking, and pain with intercourse. The most severe pain is typically associated with menstruation. Pain can also start a week before a menstrual period, during and even a week after a menstrual period, or it can be constant. The pain can be debilitating and the emotional stress can take a toll.<ref>{{cite journal |vauthors=Colette S, Donnez J | title = Are aromatase inhibitors effective in endometriosis treatment? | journal = Expert Opin Investig Drugs | volume = 20 | issue = 7 | pages = 917–31 | date = July 2011 | pmid = 21529311 | doi = 10.1517/13543784.2011.581226 }}</ref> |
|||
There is an association between endometriosis and certain types of cancers, notably some types of [[ovarian cancer]],<ref name="pmid22361336">{{cite journal |vauthors=Pearce CL, Templeman C, Rossing MA, etal | title = Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies | journal = Lancet Oncol. | volume = 13 | issue = 4 | pages = 385–94 | year = 2012 | pmid = 22361336 | pmc = 3664011 | doi = 10.1016/S1470-2045(11)70404-1 }}</ref><ref>Nezhat F. [http://hcp.obgyn.net/endometriosis/content/article/1760982/2066478 Article by Prof. Farr Nezhat, MD, FACOG, FACS, University of Columbia, May 1, 2012]</ref> [[non-Hodgkin's lymphoma]] and [[brain cancer]].<ref>{{cite journal | author = Audebert A | title = La femme endométriosique est-elle différente ? | language = French | journal = Gynécologie, Obstétrique & Fertilité | volume = 33 | issue = 4 | pages = 239–46 | date = April 2005 | pmid = 15894210 | doi = 10.1016/j.gyobfe.2005.03.010 | trans_title = Women with endometriosis: are they different from others? }}</ref> Endometriosis is unrelated to [[endometrial cancer]].<ref>{{cite journal|author=Rowlands IJ, Nagle CM, Spurdle AB, Webb PM; Australian National Endometrial Cancer Study Group and Australian Ovarian Cancer Study Group|title=Gynecological conditions and the risk of endometrial cancer|journal=Gynecol Oncol|date=Dec 2011|volume=3|pages=537–41}}</ref> |
|||
==Risk factors== |
|||
===Genetics=== |
|||
Genetic predisposition plays a role in endometriosis.<ref name=Fauser2011/> Daughters or sisters of women with endometriosis are at higher risk of developing endometriosis themselves; low progesterone levels may be genetic, and may contribute to a hormone imbalance.<ref name=emed>Kapoor D, Davila W (2005). [http://www.emedicine.com/med/topic3419.htm Endometriosis,] ''eMedicine''.</ref> There is an about six-fold increased incidence in women with an affected first-degree relative.<ref>{{cite journal |vauthors=Giudice LC, Kao LC |title=Endometriosis |journal=Lancet |volume=364 |issue=9447 |pages=1789–99 |year=2004 |pmid=15541453 |doi=10.1016/S0140-6736(04)17403-5}}</ref> |
|||
It has been proposed that endometriosis results from a series of multiple hits within target genes, in a mechanism similar to the development of cancer.<ref name=Fauser2011/> In this case, the initial mutation may be either somatic or heritable.<ref name=Fauser2011/> |
|||
Individual genomic changes (found by [[genotyping]] including [[genome-wide association study|genome-wide association studies]]) that have been associated with endometriosis include: |
|||
*Changes on [[chromosome 1]] near [[WNT4]].<ref name="RahmiogluNyholt2014"/> |
|||
*Changes on [[chromosome 2]] near GREB1.<ref name="RahmiogluNyholt2014"/> |
|||
*Changes on [[chromosome 6]] near [[ID4]].<ref name="RahmiogluNyholt2014"/> |
|||
*Changes on [[chromosome 7]] in the 7p15.2 region.<ref name="RahmiogluNyholt2014">{{cite journal |vauthors=Rahmioglu N, Nyholt DR, Morris AP, etal |title=Genetic variants underlying risk of endometriosis: insights from meta-analysis of eight genome-wide association and replication datasets|journal=Human Reproduction Update|volume=20|issue=5|year=2014|pages=702–716|issn=1355-4786|doi=10.1093/humupd/dmu015|pmid=24676469|pmc=4132588}}</ref><ref>{{cite journal |vauthors=Painter JN, Anderson CA, Nyholt DR, etal |title=Genome-wide association study identifies a locus at 7p15.2 associated with endometriosis |journal=Nature Genetics |volume=43 |issue=1 |pages=51–4 |date=January 2011 |pmid=21151130 |pmc=3019124 |doi=10.1038/ng.731}}</ref> |
|||
*Changes on [[chromosome 9]] near [[CDKN2BAS]].<ref name="RahmiogluNyholt2014"/> |
|||
*Changes on [[chromosome 10]] at region 10q26.<ref>{{cite journal |vauthors=Treloar SA, Wicks J, Nyholt DR, etal |title=Genomewide linkage study in 1,176 affected sister pair families identifies a significant susceptibility locus for endometriosis on chromosome 10q26 |journal=American Journal of Human Genetics |volume=77 |issue=3 |pages=365–76 |date=September 2005 |pmid=16080113 |pmc=1226203 |doi=10.1086/432960}}</ref> |
|||
*Changes on [[chromosome 12]] near [[VEZT]].<ref name="RahmiogluNyholt2014"/> |
|||
In addition, there is a weaker association with changes in the [[fibronectin]] gene as well as in the 2p14 region of [[chromosome 2]].<ref name="RahmiogluNyholt2014"/> |
|||
In addition, there are many findings of altered [[gene expression]] and [[epigenetics]], but both of these can also be a secondary result of, for example, environmental factors and altered metabolism. Examples of altered gene expression include that of [[miRNA]]s.<ref name=Fauser2011/> |
|||
===Environmental toxins=== |
|||
Several studies have investigated the potential link between exposure to [[dioxin]]s and endometriosis, but the evidence is equivocal and potential mechanisms are poorly understood.<ref name="pmid17981650">{{cite journal |vauthors=Anger DL, Foster WG |title=The link between environmental toxicant exposure and endometriosis |journal=Frontiers in Bioscience |volume=13 |issue= |pages=1578–93 |year=2008 |pmid=17981650 |doi=10.2741/2782}}</ref> A 2004 review of studies of dioxin and endometriosis concluded that "the human data supporting the dioxin-endometriosis association are scanty and conflicting",<ref>{{cite journal |author=Guo SW |title=The link between exposure to dioxin and endometriosis: a critical reappraisal of primate data |journal=Gynecologic and Obstetric Investigation |volume=57 |issue=3 |pages=157–73 |year=2004 |pmid=14739528 |doi=10.1159/000076374}}</ref> and a 2009 follow-up review also found that there was "insufficient evidence" in support of a link between dioxin exposure and women developing endometriosis.<ref>{{cite journal |vauthors=Guo SW, Simsa P, Kyama CM, etal |title=Reassessing the evidence for the link between dioxin and endometriosis: from molecular biology to clinical epidemiology |journal=Molecular Human Reproduction |volume=15 |issue=10 |pages=609–24 |date=October 2009 |pmid=19744969 |doi=10.1093/molehr/gap075}}</ref> A 2008 review concluded that more work was needed, stating that "although preliminary work suggests a potential involvement of exposure to dioxins in the pathogenesis of endometriosis, much work remains to clearly define cause and effect and to understand the potential mechanism of toxicity".<ref>{{cite journal |vauthors=Rier S, Foster WG |title=Environmental dioxins and endometriosis |journal=Toxicological Sciences |volume=70 |issue=2 |pages=161–70 |date=December 2002 |pmid=12441361 |doi=10.1093/toxsci/70.2.161}}</ref> |
|||
==Pathophysiology== |
|||
[[File:Peritoneal endometriosis.jpg|thumb|[[laparoscopy|Laparoscopic]] image of endometriotic lesions at the [[peritoneum]] of the pelvic wall.]] |
|||
While the exact cause of endometriosis remains unknown, many theories have been presented to better understand and explain its development. These concepts do not necessarily exclude each other. The [[pathophysiology]] of endometriosis is likely to be multifactorial and to involve an interplay between several factors.<ref name=Fauser2011/> |
|||
===Formation=== |
|||
The main theories for the formation of the ectopic endometrium are retrograde menstruation, müllerianosis, coelomic metaplasia and transplantation, each further described below. |
|||
====Retrograde menstruation theory==== |
|||
The theory of retrograde menstruation (also called the ''implantation theory'' or ''transplantation theory'')<ref>{{cite journal | author = van der Linden PJ | title = Theories on the pathogenesis of endometriosis | journal = Human reproduction (Oxford, England) | volume = 11 Suppl 3 | pages = 53–65 | year = 1996 | pmid = 9147102 | doi=10.1093/humrep/11.suppl_3.53}}</ref> is the most widely accepted theory for the formation of ectopic endometrium in endometriosis.<ref name=Fauser2011>{{cite journal |vauthors=Fauser BC, Diedrich K, Bouchard P, Domínguez F, Matzuk M, Franks S, Hamamah S, Simón C, Devroey P, Ezcurra D, Howles CM | title = Contemporary genetic technologies and female reproduction | journal = Hum. Reprod. Update | volume = 17 | issue = 6 | pages = 829–47 | year = 2011 | pmid = 21896560 | pmc = 3191938 | doi = 10.1093/humupd/dmr033 }}</ref> It suggests that during a woman's menstrual flow, some of the endometrial debris exits the uterus through the fallopian tubes and attaches itself to the peritoneal surface (the lining of the abdominal cavity) where it can proceed to invade the tissue as endometriosis.<ref name=Fauser2011/> |
|||
Retrograde menstruation alone is not able to explain all instances of endometriosis, and additional factors such as genetic or immune differences need to be invoked to account for the fact that many women with retrograde menstruation do not have endometriosis. Researchers are investigating the possibility that the [[immune system]] may not be able to cope with the cyclic onslaught of retrograde menstrual fluid. In this context there is interest in studying the relationship of endometriosis to [[autoimmune disease]], [[allergy|allergic]] reactions, and the impact of toxic materials.<ref>{{cite journal |vauthors=Gleicher N, el-Roeiy A, Confino E, Friberg J | title = Is endometriosis an autoimmune disease? | journal = Obstet Gynecol | volume = 70 | issue = 1 | pages = 115–22 | date = July 1987 | pmid = 3110710 }}</ref><ref>{{cite journal |vauthors=Capellino S, Montagna P, Villaggio B, Sulli A, Soldano S, etal | title = Role of estrogens in inflammatory response: expression of estrogen receptors in peritoneal fluid macrophages from endometriosis | journal = Annals of the New York Academy of Sciences | volume = 1069 | pages = 263–7 | date = June 2006 | pmid = 16855153 | doi = 10.1196/annals.1351.024 }}</ref> It is still unclear what, if any, causal relationship exists between toxic materials, autoimmune disease, and endometriosis. There are immune system changes in women with endometriosis, such as an increase macrophage-derived secretion products, but it is unknown if these are contributing to the disorder or are reactions from it.<ref name=Young2013>{{cite journal |vauthors=Young VJ, Brown JK, Saunders PT, Horne AW | title = The role of the peritoneum in the pathogenesis of endometriosis | journal = Human Reproduction Update | volume = 19 | issue = 5 | pages = 558–569 | year = 2013 | pmid = 23720497 | pmc = | doi = 10.1093/humupd/dmt024 }}</ref> |
|||
In addition, at least one study found that endometriotic lesions differ in their biochemistry from artificially transplanted ectopic tissue.<ref name="pmid12372441">{{cite journal | author = Redwine DB | title = Was Sampson wrong? | journal = Fertility and Sterility | volume = 78 | issue = 4 | pages = 686–93 | date = October 2002 | pmid = 12372441 | doi = 10.1016/S0015-0282(02)03329-0 }}</ref> This is likely because the cells that give rise to endometriosis are a side population of cells.<ref name=Fauser2011/> Similarly, there are changes in for example the [[mesothelium]] of the [[peritoneum]] in women with endometriosis, such as loss of [[tight junction]]s, but it is unknown if these are causes or effects of the disorder.<ref name=Young2013/> |
|||
In rare cases where [[imperforate hymen]] does not resolve itself prior to the first menstrual cycle and goes undetected, blood and [[endometrium]] are trapped within the uterus of the woman until such time as the problem is resolved by surgical incision. Many health care practitioners never encounter this defect, and due to the [[flu-like symptoms]] it is often misdiagnosed or overlooked until multiple menstrual cycles have passed. By the time a correct diagnosis has been made, endometrium and other fluids have filled the uterus and fallopian tubes with results similar to retrograde menstruation resulting in endometriosis. The initial stage of endometriosis may vary based on the time elapsed between onset and surgical procedure.{{citation needed|date=March 2016}} |
|||
The theory of retrograde menstruation as a cause of endometriosis was first proposed by [[John A. Sampson]]. |
|||
====Other theories==== |
|||
*Stem cells: Endometriosis may arise from stem cells from bone marrow and potentially other sources. In particular this theory explains endometriosis found in areas remote from the pelvis such as the brain or lungs.<ref>{{cite journal|last1=Hufnagel|first1=D|last2=Li|first2=F|last3=Cosar|first3=E|last4=Krikun|first4=G|last5=Taylor|first5=HS|title=The Role of Stem Cells in the Etiology and Pathophysiology of Endometriosis.|journal=Seminars in reproductive medicine|date=September 2015|volume=33|issue=5|pages=333–40|pmid=26375413|doi=10.1055/s-0035-1564609}}</ref> |
|||
*Environment; Environmental toxins (e.g.; dioxin, nickel) may cause endometriosis.<ref name=Bruner-Tran_2008>{{Cite journal | pmid = 18394613| year = 2008| author1 = Bruner-Tran| first1 = K.L.| title = Dioxin may promote inflammation-related development of endometriosis.| journal = Fertility and Sterility| last2 = Yeaman| first2 = G.R.| last3 = Crispens| first3 = M.A.| last4 = Igarashi| first4 = T.M.| last5 = Osteen| first5 = K.G.| doi = 10.1016/j.fertnstert.2008.02.102| volume=89| pages=1287–98| pmc=2430157}}</ref><ref>{{Cite journal| doi = 10.1371/journal.pone.0139388| issn = 1932-6203| volume = 10| issue = 10| pages = –0139388| last1 = Yuk| first1 = Jin-Sung| last2 = Shin| first2 = Jong Seung| last3 = Shin| first3 = Ji-Yeon| last4 = Oh| first4 = Eunsuk| last5 = Kim| first5 = Hyunmee| last6 = Park| first6 = Won I.| title = Nickel Allergy Is a Risk Factor for Endometriosis: An 11-Year Population-Based Nested Case-Control Study| journal = PloS One| date = 2015| pmid = 26439741}}</ref> |
|||
*Müllerianosis: A theory supported by foetal autopsy is that cells with the potential to become endometrial, which are laid down in tracts during embryonic development called the female reproductive (Mullerian) tract as it migrates downward at 8–10 weeks of embryonic life, could become dislocated from the migrating uterus and act like seeds or [[stem cells]].<ref name=signorile2009>{{cite journal |vauthors=Signorile PG, Baldi F, Bussani R, D'Armiento M, De Falco M, Baldi A | title = Ectopic endometrium in human foetuses is a common event and sustains the theory of müllerianosis in the pathogenesis of endometriosis, a disease that predisposes to cancer | journal = Journal of Experimental & Clinical Cancer Research | volume = 28 | issue = | page = 49 | date = April 2009 | pmid = 19358700 | pmc = 2671494 | doi = 10.1186/1756-9966-28-49 | url = http://www.jeccr.com/content/28//49 }}</ref> |
|||
*Coelomic metaplasia: [[Coelomic]] cells which are the common ancestor of [[endometrial]] and [[peritoneal]] cells may undergo [[metaplasia]] (transformation) from one type of cell to the other, perhaps triggered by inflammation.<ref name=aafp1999>{{cite web|url=http://www.aafp.org/afp/991015ap/1753.html |title=Diagnosis and Treatment of Endometriosis |publisher=American Academy of Family Physicians|date=1999-10-15 |accessdate=2011-07-26}}</ref> |
|||
*Vasculogenesis: Up to 37% of the microvascular [[endothelium]] of ectopic endometrial tissue originates from [[endothelial progenitor cell]]s, which result in ''de novo'' formation of microvessels by the process of [[vasculogenesis]] rather than the conventional process of [[angiogenesis]].<ref>{{cite journal |vauthors=Laschke MW, Giebels C, Menger MD | title = Vasculogenesis: a new piece of the endometriosis puzzle | journal = Hum. Reprod. Update | volume = 17 | issue = 5 | pages = 628–36 | year = 2011 | pmid = 21586449 | doi = 10.1093/humupd/dmr023 | url = }}</ref>{{clarify|reason=what's the theory here? |date=March 2016}} |
|||
*Neural growth: An increased expression of new nerve fibres is found in endometriosis, but does not fully explain the formation of ectopic endometrial tissue, and is not definitely correlated with the amount of perceived pain.<ref name="MorottiVincent2014">{{cite journal|vauthors=Morotti M, Vincent K, Brawn J, Zondervan KT, Becker CM |title=Peripheral changes in endometriosis-associated pain|journal=Human Reproduction Update|volume=20| issue=5| year=2014| pages=717–736| issn=1355-4786|doi=10.1093/humupd/dmu021| pmid=24859987| pmc=4337970}}</ref>{{clarify|reason=what's the theory here? |date=March 2016}} |
|||
*Autoimmune: Graves disease is an autoimmune disease characterized by hyperthyroidism, goiter, ophthalmopathy, and dermopathy. Women with endometriosis had higher rates of Graves disease. One of these potential links between Graves disease and endometriosis is autoimmunity.<ref>{{Cite journal| doi = 10.1097/MD.0000000000002975| issn = 1536-5964| volume = 95| issue = 10| pages = –2975| last1 = Yuk| first1 = Jin-Sung| last2 = Park| first2 = Eun-Ju| last3 = Seo| first3 = Yong-Soo| last4 = Kim| first4 = Hee Jin| last5 = Kwon| first5 = Seon-Young| last6 = Park| first6 = Won I.| title = Graves Disease Is Associated With Endometriosis: A 3-Year Population-Based Cross-Sectional Study| journal = Medicine| date = 2016| pmid = 26962803}}</ref><ref>{{Cite journal| doi = 10.1016/S0140-6736(04)17403-5| issn = 1474-547X| volume = 364| issue = 9447| pages = 1789–1799| last1 = Giudice| first1 = Linda C| last2 = Kao| first2 = Lee C| title = Endometriosis| journal = Lancet| date = 2004| pmid = 15541453}}</ref> |
|||
===Localization=== |
|||
[[File:Endometriosis loc en.svg|thumb|possible locations of endometriosis]] |
|||
Most endometriosis is found on these structures in the [[pelvic cavity]]:<ref>{{cite journal|vauthors=Jenkins S, Olive DL, Haney AF |title=Endometriosis: pathogenetic implications of the anatomic distribution|journal=Obstetrics and gynecology|date=March 1986|volume=67|issue=3|pages=335–8|pmid=3945444}}</ref> |
|||
* [[Ovary|Ovaries]] (the most common site) |
|||
* [[Fallopian tube]]s |
|||
* The back of the [[uterus]] and the posterior [[Rectouterine pouch|cul-de-sac]] |
|||
* The front of the uterus and the anterior cul-de-sac |
|||
* Uterine [[ligament]]s such as the broad or round ligament of the uterus |
|||
* Pelvic and back wall |
|||
* [[Intestine]]s, most commonly the rectosigmoid |
|||
* [[Urinary bladder]] and [[ureter]]s |
|||
Rectovaginal or bowel endometriosis affects approximately 5-12% of women with endometriosis, and can cause severe pain with bowel movements.<ref>{{cite journal|vauthors=Weed JC, Ray JE |title=Endometriosis of the bowel|journal=Obstetrics and gynecology|date=May 1987|volume=69|issue=5|pages=727–30|pmid=3574800}}</ref> |
|||
Endometriosis may spread to the [[cervix]] and [[vagina]] or to sites of a surgical abdominal incision, known as "scar endometriosis."<ref>{{cite journal|vauthors=Uzunçakmak C, Güldaş A, Ozçam H, Dinç K |title=Scar endometriosis: a case report of this uncommon entity and review of the literature|journal=Case reports in obstetrics and gynecology|date=2013|volume=2013|pages=386783|pmid=23762683|doi=10.1155/2013/386783|pmc=3665185}}</ref> Risk factors for scar endometriosis include previous abdominal surgeries, such as a hysterotomy or cesarean section, or ectopic pregnancies, salpingostomy puerperal sterilization, laparoscopy, amniocentesis, appendectomy, episiotomy, vaginal hysterectomies, and hernia repair.<ref>{{cite journal|vauthors=Dwivedi AJ, Agrawal SN, Silva YJ |title=Abdominal wall endometriomas|journal=Digestive diseases and sciences|date=February 2002|volume=47|issue=2|pages=456–61|pmid=11855568}}</ref><ref>{{cite journal|vauthors=Kaunitz A, Di Sant'Agnese PA |title=Needle tract endometriosis: an unusual complication of amniocentesis|journal=Obstetrics and gynecology|date=December 1979|volume=54|issue=6|pages=753–5|pmid=160025}}</ref><ref>{{cite journal|vauthors=Koger KE, Shatney CH, Hodge K, McClenathan JH |title=Surgical scar endometrioma.|journal=Surgery, gynecology & obstetrics|date=September 1993|volume=177|issue=3|pages=243–6|pmid=8356497}}</ref> |
|||
Endometriosis may also present with skin lesions in [[cutaneous endometriosis]]. |
|||
Less commonly lesions can be found on the diaphragm. Diaphragmatic endometriosis is rare, almost always on the right hemidiaphragm, and may inflict the cyclic pain of the right shoulder just before and during a menstrual period. Rarely, endometriosis can be extraperitoneal and is found in the lungs and CNS.<ref name=WebMD >{{cite web| author = Daly S | title =Endometrioma/Endometriosis| work = | url=http://www.emedicine.com/radio/topic250.htm | date= October 18, 2004 | publisher=WebMD | accessdate=2006-12-19}}</ref> |
|||
==Diagnosis== |
|||
[[File:Endometrioma.jpg|thumb|[[Transvaginal ultrasonography]] showing a 67 x 40 mm [[endometrioma]] as distinguished from other types of [[ovarian cyst]]s by a somewhat grainy and not completely [[anechoic]] content.]] |
|||
A health history and a physical examination can lead the health care practitioner to suspect endometriosis. Although doctors can often feel the endometrial growths during a pelvic exam, and these symptoms may be signs of endometriosis, diagnosis cannot be confirmed by exam only. Use of pelvic ultrasound may identify large endometriotic cysts (called [[endometrioma]]s). However, smaller endometriosis implants cannot be visualized with ultrasound technique.{{citation needed||date=March 2016}} |
|||
===Laparoscopy=== |
|||
[[File:Douglas endometriose.jpg|thumb|[[laparoscopy|Laparoscopic]] image of endometriotic lesions in the [[Pouch of Douglas]] and on the right [[sacrouterine ligament]].]] |
|||
[[Laparoscopy]], a surgical procedure where a camera is used to look inside the abdominal cavity, is the only way to officially diagnose endometriosis as it permits lesion visualization unless the lesion is visible externally, e.g. an endometriotic nodule in the vagina. If the growths are not visible, a [[biopsy]] may be taken to determine the diagnosis.<ref>Office on Women’s Health, U.S. Department of Health and Human Services. (16 July 2012). Endometriosis Fact Sheet. Retrieved from Womenshealth.gov http://www.womenshealth.gov/publications/our-publications/fact-sheet/endometriosis.html</ref> Surgery for diagnoses also allows for surgical treatment of endometriosis at the same time. |
|||
To the eye, lesions can appear dark blue, powder-burn black, red, white, yellow, brown or non-pigmented. Lesions vary in size. Some within the pelvis walls may not be visible, as normal-appearing peritoneum of infertile women reveals endometriosis on biopsy in 6–13% of cases.<ref>{{cite journal |vauthors=Nisolle M, Paindaveine B, Bourdon A, Berlière M, Casanas-Roux F, Donnez J | title = Histologic study of peritoneal endometriosis in infertile women | journal = Fertility and Sterility | volume = 53 | issue = 6 | pages = 984–8 | date = June 1990 | pmid = 2351237 }}</ref> Early endometriosis typically occurs on the surfaces of organs in the pelvic and intra-abdominal areas. Health care providers may call areas of endometriosis by different names, such as implants, lesions, or nodules. Larger lesions may be seen within the ovaries as endometriomas or "chocolate cysts", "chocolate" because they contain a thick brownish fluid, mostly old blood.{{citation needed||date=March 2016}} |
|||
Frequently during diagnostic [[laparoscopy]], no lesions are found in women with chronic pelvic pain, a symptom common to other disorders including adenomyosis, pelvic adhesions, pelvic inflammatory disease, congenital anomalies of the reproductive tract, and ovarian or tubal masses.<ref name="committee">{{cite journal|last1=Practice Committee of the American Society for Reproductive|first1=Medicine|title=Treatment of pelvic pain associated with endometriosis: a committee opinion. |journal=Fertility and Sterility|date=April 2014|volume=101|issue=4| pages=927–35| pmid=24630080| doi= 10.1016/j.fertnstert.2014.02.012 }}</ref> |
|||
===Staging=== |
|||
Surgically, endometriosis can be staged I–IV by the revised classification of the [[American Society of Reproductive Medicine]] from 1997.<ref name="pmid9130884">{{cite journal | author = American Society For Reproductive M, | title = Revised American Society for Reproductive Medicine classification of endometriosis: 1996 | journal = Fertility and Sterility | volume = 67 | issue = 5 | pages = 817–21 | date = May 1997 | pmid = 9130884 | doi = 10.1016/S0015-0282(97)81391-X }}</ref> The process is a complex point system that assesses lesions and adhesions in the pelvic organs, but it is important to note staging assesses physical disease only, not the level of pain or infertility. A person with Stage I endometriosis may have a little disease and severe pain, while a person with Stage IV endometriosis may have severe disease and no pain or vice versa. In principle the various stages show these findings:{{citation needed||date=March 2016}} |
|||
;Stage I (Minimal) |
|||
: Findings restricted to only superficial lesions and possibly a few filmy [[adhesions]] |
|||
;Stage II (Mild) |
|||
: In addition, some deep lesions are present in the [[Rectouterine pouch|cul-de-sac]] |
|||
;Stage III (Moderate) |
|||
: As above, plus the presence of endometriomas on the ovary and more adhesions. |
|||
;Stage IV (Severe) |
|||
: As above, plus large endometriomas, extensive adhesions. |
|||
===Markers=== |
|||
An area of research is the search for endometriosis [[biomarker|markers]].<ref name=May2010/> |
|||
In 2010 essentially all proposed biomarkers for endometriosis were of unclear medical use, although some appear to be promising.<ref name=May2010>{{cite journal |vauthors=May KE, Conduit-Hulbert SA, Villar J, Kirtley S, Kennedy SH, Becker CM | title = Peripheral biomarkers of endometriosis: a systematic review | journal = Hum. Reprod. Update | volume = 16 | issue = 6 | pages = 651–74 | year = 2010 | pmid = 20462942 | pmc = 2953938 | doi = 10.1093/humupd/dmq009 }}</ref> The one biomarker that has been in use over the last 20 years is [[CA-125]].<ref name=May2010/> A 2016 review found that in those with symptoms of endometriosis and once [[ovarian cancer]] has been ruled out, a positive CA-125 may confirm the diagnosis.<ref name=Hir2016>{{cite journal|last1=Hirsch|first1=M|last2=Duffy|first2=J|last3=Davis|first3=CJ|last4=Nieves Plana|first4=M|last5=Khan|first5=KS|last6=International Collaboration to Harmonise Outcomes and Measures for|first6=Endometriosis.|title=Diagnostic accuracy of cancer antigen 125 for endometriosis: a systematic review and meta-analysis.|journal=BJOG : an international journal of obstetrics and gynaecology|date=October 2016|volume=123|issue=11|pages=1761–8|pmid=27173590|doi=10.1111/1471-0528.14055}}</ref> Its performance in ruling out endometriosis; however, is low.<ref name=Hir2016/> CA-125 levels appear to fall during endometriosis treatment, but has not shown a correlation with disease response.<ref name=May2010/> |
|||
Another review in 2011 identified several putative biomarkers upon biopsy, including findings of small sensory nerve fibers or defectively expressed [[Beta-3 integrin|β3 integrin]] subunit.<ref>{{cite journal |vauthors=May KE, Villar J, Kirtley S, Kennedy SH, Becker CM | title = Endometrial alterations in endometriosis: a systematic review of putative biomarkers | journal = Hum. Reprod. Update | volume = 17 | issue = 5 | pages = 637–53 | year = 2011 | pmid = 21672902 | doi = 10.1093/humupd/dmr013 }}</ref> It has been postulated a future diagnostic tool for endometriosis will consist of a panel of several specific and sensitive biomarkers, including both substance concentrations and genetic predisposition.<ref name=May2010/> |
|||
===Histopathology=== |
|||
[[Image:Endometriosis, abdominal wall.jpg|thumb|Endometriosis, abdominal wall]] |
|||
[[Image:Endometriosis of the ovary.jpg|thumb|right|[[Micrograph]] showing endometriosis (right) and ovarian stroma (left). [[H&E stain]].]] |
|||
[[Image:Endometrioma1.jpg|thumb|right|[[Micrograph]] of the wall of an endometrioma. All features of endometriosis are present (endometrial [[gland]]s, endometrial [[stroma (animal tissue)|stroma]] and [[hemosiderin]]-laden [[macrophage]]s). [[H&E stain]].]] |
|||
Typical endometriotic lesions show [[histopathology|histopathologic]] features similar to [[endometrium]], namely endometrial [[stroma (animal tissue)|stroma]], endometrial [[epithelium]], and glands that respond to hormonal stimuli. Older lesions may display no glands but [[hemosiderin]] deposits (see photomicrograph on right) as residual.{{citation needed||date=March 2016}} |
|||
Immunohistochemistry has been found to be useful in diagnosing endometriosis as stromal cells have a peculiar surface antigen, CD10, thus allowing the pathologist go straight to a staining area and hence confirm the presence of stromal cells and sometimes glandular tissue is thus identified that was missed on routine H&E staining.<ref>http://www.rfay.com.au/docs/cd10poster.pdf</ref>{{better source||date=March 2016}} |
|||
===Pain quantification=== |
|||
The most common [[pain scale]] for quantification of endometriosis-related pain is the [[visual analogue scale]] (VAS); VAS and [[numerical rating scale]] (NRS) were the best adapted pain scales for pain measurement in endometriosis. For research purposes, and for more detailed pain measurement in clinical practice, VAS or NRS for each type of typical pain related to endometriosis ([[dysmenorrhea]], deep [[dyspareunia]] and non-menstrual [[chronic pelvic pain]]), combined with the [[clinical global impression]] (CGI) and a [[quality of life]] scale, are used.<ref name="BourdelAlves2014">{{cite journal |vauthors=Bourdel N, Alves J, Pickering G, etal |title=Systematic review of endometriosis pain assessment: how to choose a scale?|journal=Human Reproduction Update|volume=21|issue=1|year=2014|pages=136–152|issn=1355-4786|doi=10.1093/humupd/dmu046|pmid=25180023}}</ref> |
|||
==Prevention== |
|||
Limited evidence indicates that the use of [[combined oral contraceptive pill|combined oral contraceptives]] is associated with a reduced risk of endometriosis.<ref name=Ver2011/> |
|||
==Management== |
|||
While there is no cure for endometriosis, there are two types of interventions; treatment of pain and treatment of [[endometriosis-associated infertility]].<ref name="TreatmentEKSNI">{{cite web | title =What are the treatments for endometriosis | work = | publisher =Eunice Kennedy Shriver National Institute of Child Health and Human Development | url = http://www.nichd.nih.gov/health/topics/endometri/conditioninfo/Pages/treatment.aspx | accessdate =20 August 2013 }}</ref> In many women menopause (natural or surgical) will abate the process.<ref name="pmid20627430">{{cite journal |vauthors=Moen MH, Rees M, Brincat M, etal | title = EMAS position statement: Managing the menopause in women with a past history of endometriosis | journal = Maturitas | volume = 67 | issue = 1 | pages = 94–7 | year = 2010 | pmid = 20627430 | doi = 10.1016/j.maturitas.2010.04.018 }}</ref> In women in the reproductive years, endometriosis is merely managed: the goal is to provide pain relief, to restrict progression of the process, and to restore or preserve fertility where needed. In younger women, surgical treatment attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue.<ref name="AFFDiagnosisandTreat">{{cite journal | author = Wellbery C | title = Diagnosis and treatment of endometriosis | journal = Am Fam Physician | volume = 60 | issue = 6 | pages = 1753–62, 1767–8 | year = 1999 | pmid = 10537390 | doi = | url = http://www.aafp.org/afp/1999/1015/p1753.html }}</ref> |
|||
In general, the diagnosis of endometriosis is confirmed during surgery, at which time ablative steps can be taken. Further steps depend on circumstances: a woman without infertility can be managed with hormonal medication that suppresses the natural cycle and pain medication, while an infertile woman may be treated expectantly after surgery, with fertility medication, or with [[IVF]]. As to the surgical procedure, [[ablation]] (or [[fulguration]]) of endometriosis (burning and vaporizing the lesions with an electric device) has shown a high rate of short-term recurrence after the procedure. The best surgical procedure with much lower rate of short-term recurrence is to excise (cut and remove) the lesions completely.{{mcn|date=April 2015}} |
|||
===Surgery=== |
|||
Conservative treatment consists of the excision of the [[endometrium]], [[adhesions]], resection of endometriomas, and restoration of normal pelvic anatomy as much as is possible.<ref name=speroff>{{Cite book|vauthors=Speroff L, Glass RH, Kase NG |title=Clinical Gynecologic Endocrinology and Infertility |publisher=Lippincott Willimas Wilkins |edition=6th |page=1057 |isbn=0-683-30379-1 |year=1999}}</ref> Endometrioma on the ovary of any significant size (Approx. 2 cm +) -sometimes misdiagnosed as ovarian cysts- must be removed surgically because hormonal treatment alone will not remove the full endometrioma cyst, which can progress to acute pain from the rupturing of the cyst and internal bleeding.{{mcn|date=March 2016}} [[Laparoscopy]], besides being used for diagnosis, can also be used to perform surgery. It's considered a "minimally invasive" surgery because the surgeon makes very small openings (incisions) at (or around) the belly button and lower portion of the belly. A thin telescope-like instrument (the laparoscope) is placed through one incision, which allows the doctor to look for endometriosis using a small camera attached to the laparoscope. Small instruments are inserted through the incisions to remove the endometriosis tissue and adhesions. Because the incisions are very small, there will only be small scars on the skin after the procedure, and all endometriosis can be removed, and women recover from surgery quicker and have a lower risk of adhesions.<ref>{{cite web |url=http://www.asrm.org/uploadedFiles/ASRM_Content/Resources/Patient_Resources/Fact_Sheets_and_Info_Booklets/endometriosis_infertility.pdf |title=Endometriosis and Infertility: Can Surgery Help? |year=2008 |publisher=American Society for Reproductive Medicine |accessdate=31 Oct 2010}}</ref> |
|||
55% to 100% of women develop adhesions following pelvic surgery,<ref name="LiakokosPAE">{{cite journal |vauthors=Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL | title = Peritoneal Adhesions: Etiology, Pathophysiology, and Clinical Significance | language = | journal = Dig Surgery | volume = 18 | issue = 4 | pages = 260–273 | year = 2001 | pmid = 11528133 | doi = 10.1159/000050149 }}</ref> which can result in infertility, chronic abdominal and pelvic pain, and difficult reoperative surgery. Trehan's temporary ovarian suspension, a technique in which the ovaries are suspended for a week after surgery may be used to reduce the incidence of adhesions after endometriosis surgery.<ref>{{cite journal | author = Trehan AK | title = Temporary ovarian suspension | journal = Gynaecological Endoscopy | volume = 11 | pages = 309–314 | year = 2002 | doi=10.1046/j.1365-2508.2002.00520.x | issue=1}}</ref><ref name="pmid11821616">{{cite journal |vauthors=Abuzeid MI, Ashraf M, Shamma FN | title = Temporary ovarian suspension at laparoscopy for prevention of adhesions | journal = J Am Assoc Gynecol Laparosc | volume = 9 | issue = 1 | pages = 98–102 | year = 2002 | pmid = 11821616 }}</ref> |
|||
Conservative treatment involves excision of endometriosis while preserving the ovaries and uterus, very important for women wishing to conceive, but may increase the risk of recurrence.<ref>{{cite journal |vauthors=Namnoum AB, Hickman TN, Goodman SB, Gehlbach DL, Rock JA | title = Incidence of symptom recurrence after hysterectomy for endometriosis | journal = Fertility and Sterility | volume = 64 | issue = 5 | pages = 898–902 | date = November 1995 | pmid = 7589631 }}</ref> |
|||
Endometriosis recurrence following conservative surgery is estimated as 21.5% at 2 years and 40-50% at 5 years.<ref>{{cite journal | author = Guo SW | title = Recurrence of endometriosis and its control | journal = Hum. Reprod. Update | year = 2009 | pmid = 19279046 | doi=10.1093/humupd/dmp007 | volume=15 | issue=4 | pages=441–61}}</ref> |
|||
A [[hysterectomy]] (removal of the uterus) can be used to treat endometriosis in women who do not wish to conceive. However, this should only be done when combined with removal of the endometriosis by excision, as if endometriosis is not also removed at the time of hysterectomy, pain may persist.<ref name="Johnson NP, Hummelshoj L; World Endometriosis Society Montpellier Consortium 2013">{{cite journal |vauthors=Johnson NP, Hummelshoj L | title = Consensus on current management of endometriosis. | journal = Human Reproduction | date = June 2013 | pmid = 23528916 | doi=10.1093/humrep/det050 | volume=28 | issue=6 | pages=1552–68}}</ref> |
|||
For women with extreme pain, a presacral neurectomy may be very rarely performed where the nerves to the uterus are cut. However, this technique is almost never used due to the high incidence of associated complications including presacral hematoma and irreversible problems with urination and constipation.<ref name="Johnson NP, Hummelshoj L; World Endometriosis Society Montpellier Consortium 2013"/> |
|||
===Hormones=== |
|||
* [[Progesterone]] or [[progestins]]: Progesterone counteracts estrogen and inhibits the growth of the endometrium.<ref name="PatelElguero2014">{{cite journal |vauthors=Patel B, Elguero S, Thakore S, etal |title=Role of nuclear progesterone receptor isoforms in uterine pathophysiology|journal=Human Reproduction Update|volume=21|issue=2|year=2014|pages=155–173|issn=1355-4786|doi=10.1093/humupd/dmu056|pmid=25406186|pmc=4366574}}</ref> Such therapy can reduce or eliminate menstruation in a controlled and reversible fashion. Progestins are chemical variants of natural progesterone. An example of a progestin is [[dienogest]] (Visanne). |
|||
* Avoiding products with [[xenoestrogen]]s, which have a similar effect to naturally produced estrogen and can increase growth of the endometrium.{{mcn|date=April 2015}} |
|||
* Hormone contraception therapy: [[Combined oral contraceptive pill|Oral contraceptive]]s reduce the menstrual pain associated with endometriosis.{{MEDRS|date=April 2015}}<ref>{{primary-source inline|date=April 2015}} {{cite journal |vauthors=Harada T, Momoeda M, Taketani Y, Hoshiai H, Terakawa N | title = Low-dose oral contraceptive pill for dysmenorrhea associated with endometriosis: a placebo-controlled, double-blind, randomized trial | journal = Fertility and Sterility | volume = 90 | issue = 5 | pages = 1583–8 | date = November 2008 | pmid = 18164001 | doi = 10.1016/j.fertnstert.2007.08.051 }}</ref> They may function by reducing or eliminating menstrual flow and providing estrogen support. Typically, it is a long-term approach. |
|||
* [[Danazol]] (danocrine) and [[gestrinone]] are suppressive steroids with some androgenic activity.<ref name="AFFDiagnosisandTreat"/> Both agents inhibit the growth of endometriosis but their use remains limited as they may cause [[hirsutism]] and voice changes.{{mcn|date=April 2015}} |
|||
* [[GnRH agonist|Gonadotropin-releasing hormone (GnRH) agonist]]s: These drugs are thought to work by decreasing hormone levels.<ref name="brown2010" /> A 2010 Cochrane review found that GnRH agonists were more effective for pain relief in endometriosis than no treatment or [[placebo]], but were no more effective than danazol or intrauterine progestagen, and had more side effects than danazol.<ref name="brown2010">{{cite journal |authors=Brown J, Pan A, Hart RJ |title=Gonadotrophin-releasing hormone analogues for pain associated with endometriosis |journal=Cochrane Database Syst Rev |issue=12 |pages=CD008475 |year=2010 |pmid=21154398 |doi=10.1002/14651858.CD008475.pub2}}</ref> |
|||
*[[Aromatase inhibitor]]s are medications that block the formation of estrogen and have become of interest for researchers who are treating endometriosis.<ref>{{cite journal |vauthors=Attar E, Bulun SE | title = Aromatase inhibitors: the next generation of therapeutics for endometriosis? | journal = Fertility and Sterility | volume = 85 | issue = 5 | pages = 1307–18 | date = May 2006 | pmid = 16647373 | doi = 10.1016/j.fertnstert.2005.09.064 }}</ref> |
|||
===Other medication=== |
|||
* [[NSAID]]s: Anti-inflammatory. They are commonly used in conjunction with other therapy. For more severe cases narcotic prescription drugs may be used. NSAID injections can be helpful for severe pain or if stomach pain prevents oral NSAID use. |
|||
* [[Opioid]]s: [[Morphine]] sulphate tablets and other opioid painkillers work by mimicking the action of naturally occurring pain-reducing chemicals called "[[endorphins]]". There are different long acting and short acting medications that can be used alone or in combination to provide appropriate pain control. |
|||
* Following laparoscopic surgery women who were given Chinese herbs were reported to have comparable benefits to women with conventional drug treatments, though the journal article that reviewed this study also noted that "the two trials included in this review are of poor methodological quality so these findings must be interpreted cautiously. Better quality randomised controlled trials are needed to investigate a possible role for CHM [Chinese Herbal Medicine] in the treatment of endometriosis."<ref>{{Cite journal|last=Flower|first=Andrew|last2=Liu|first2=Jian Ping|last3=Lewith|first3=George|last4=Little|first4=Paul|last5=Li|first5=Qing|date=2012-05-16|title=Chinese herbal medicine for endometriosis|journal=The Cochrane Database of Systematic Reviews|issue=5|pages=CD006568|doi=10.1002/14651858.CD006568.pub3|issn=1469-493X|pmid=22592712}}</ref> |
|||
* [[Pentoxifylline]], an immunomodulating agent, has been theorized to improve pain as well as improve pregnancy rates in women with endometriosis. A 2012 Cochrane review, however, found that there was not enough evidence to support the effectiveness or safety of either of these uses.<ref>{{cite journal |vauthors=Lu D, Song H, Li Y, Clarke J, Shi G | title = Pentoxifylline for endometriosis. | journal = Cochrane database of systematic reviews (Online) | volume = 1 | pages = CD007677 | date = Jan 18, 2012 | pmid = 22258970 | doi = 10.1002/14651858.CD007677.pub3 }}</ref> Current [[American Congress of Obstetricians and Gynecologists]] (ACOG) guidelines do not include immune-modulators, such as pentoxifylline, in standard treatment protocols.<ref>{{cite journal | title = Practice bulletin no. 114 management of endometriosis | journal = Obstet Gynecol | volume = 116 | issue = 1 | pages = 223–36 | date = July 2010 | pmid = 20567196 | doi = 10.1097/AOG.0b013e3181e8b073 }}</ref> |
|||
*[[Angiogenesis inhibitor]]s lack clinical evidence of efficacy in endometriosis therapy.<ref name="Laschke2012">{{cite journal |vauthors=Laschke MW, Menger MD | title = Anti-angiogenic treatment strategies for the therapy of endometriosis | journal = Human Reproduction Update | volume = 18 | issue = 6 | pages = 682–702 | year = 2012 | pmid = 22718320 | pmc = | doi = 10.1093/humupd/dms026 }}</ref> Under experimental ''[[in vitro]]'' and ''[[in vivo]]'' conditions, compounds that have been shown to exert inhibitory effects on endometriotic lesions include growth factor inhibitors, endogenous angiogenesis inhibitors, fumagillin analogues, [[statin]]s, [[cyclo-oxygenase-2 inhibitor]]s, [[phytochemical]] compounds, [[immunomodulator]]s, [[dopamine agonist]]s, [[peroxisome proliferator-activated receptor agonist]]s, [[progestin]]s, [[danazol]] and [[gonadotropin-releasing hormone agonist]]s.<ref name=Laschke2012/> However, many of these agents are associated with undesirable side effects and more research is necessary. An ideal therapy would diminish inflammation and underlying symptoms without being contraceptive.<ref name="pmid23485944">{{cite journal |vauthors=Canny GO, Lessey BA | title = The role of lipoxin A4 in endometrial biology and endometriosis | journal = Mucosal Immunol | volume = 6 | issue = 3 | pages = 439–50 | year = 2013 | pmid = 23485944 | doi = 10.1038/mi.2013.9 | pmc=4062302}}</ref><ref name="pmid23356536">{{cite journal |vauthors=Streuli I, de Ziegler D, Santulli P, etal | title = An update on the pharmacological management of endometriosis | journal = Expert Opin Pharmacother | volume = 14 | issue = 3 | pages = 291–305 | year = 2013 | pmid = 23356536 | doi = 10.1517/14656566.2013.767334 }}</ref> |
|||
The overall effectiveness of manual physical therapy to treat endometriosis has not yet been identified.<ref name="pmid21589790">{{cite journal |vauthors=Valiani M, Ghasemi N, Bahadoran P, Heshmat R | title = The effects of massage therapy on dysmenorrhea caused by endometriosis | journal = Iran J Nurs Midwifery Res | volume = 15 | issue = 4 | pages = 167–71 | year = 2010 | pmid = 21589790 | pmc = 3093183 | doi = }}</ref> There is no evidence to support nutritional therapy as effective. |
|||
===Comparison of interventions=== |
|||
Medicinal and surgical interventions produce roughly equivalent pain-relief benefits. Recurrence of pain was found to be 44 and 53 percent with medicinal and surgical interventions, respectively.<ref name= emed/> Each approach has advantages and disadvantages.<ref name=aafp1999/> Manual therapy showed a decrease in pain for 84 percent of study participants, and a 93 percent improvement in sexual function.{{MEDRS|date=April 2015}}<ref name="JOEPPD">{{primary-source inline|date=April 2015}} {{cite journal |vauthors=Wurn BF, Wurn LJ, Patterson K, King CR, Scharf ES | title =Decreasing dyspareunia and dysmenorrhea in women with endometriosis via a manual physical therapy: Results from two independent studies | journal =Journal of Endometriosis and Pelvic Pain Disorders | volume = 3| issue = | pages = 188–196| year =2011 | url = http://www.j-endometriosis.com/article/decreasing-dyspareunia-and-dysmenorrhea-in-women-with-endometriosis-via-a-manual-physical-therapy--results-from-two-independent-studies-je-11-0029 | doi =10.5301/JE.2012.9088 }}</ref> |
|||
Evidence on how effective medication is for relieving pain associated with endometriosis is limited.<ref name="TreatmentEKSNI"/> |
|||
The advantages of surgery are demonstrated efficacy for pain control,<ref>{{cite journal |vauthors=Kaiser A, Kopf A, Gericke C, Bartley J, Mechsner S | title = The influence of peritoneal endometriotic lesions on the generation of endometriosis-related pain and pain reduction after surgical excision | journal = Arch Gynecol Obstet. | volume = 280 | issue = 3 | pages = 369–73 | date = 16 January 2009 | pmid = 19148660 | doi = 10.1007/s00404-008-0921-z }}</ref> it is more effective for infertility than medicinal intervention,<ref name="AFFDiagnosisandTreat"/> it provides a definitive diagnosis,<ref name="AFFDiagnosisandTreat"/> and surgery can often be performed as a minimally invasive (laparoscopic) procedure to reduce morbidity and minimize the risk of post-operative adhesions.<ref>{{cite journal |vauthors=Radosa MP, Bernardi TS, Georgiev I, Diebolder H, Camara O, Runnebaum IB | title = Coagulation versus excision of primary superficial endometriosis: a 2-year follow-up | journal = Eur. J. Obstet. Gynecol. Reprod. Biol. | volume = 150 | issue = 2 | pages = 195–8 | date = June 2010 | pmid = 20303642 | doi = 10.1016/j.ejogrb.2010.02.022 | url = http://linkinghub.elsevier.com/retrieve/pii/S0301-2115(10)00087-4 }}</ref> Efforts to develop effective strategies to reduce or prevent adhesions have been undertaken, but their formation remain a frequent side effect of abdominal surgery.<ref name="LiakokosPAE"/> |
|||
The advantages of physical therapy techniques are decreased cost, absence of major side-effects, it does not interfere with fertility, and near-universal increase of sexual function.<ref name="JOEPPD"/> Disadvantages are that there are no large or long-term studies of its use for treating pain or infertility related to endometriosis.<ref name="JOEPPD"/> |
|||
===Treatment of infertility=== |
|||
{{Main article|Endometriosis and infertility}} |
|||
Surgery is more effective than medicinal intervention for addressing infertility associated with endometriosis.<ref name="AFFDiagnosisandTreat"/> Surgery attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue.<ref name="AFFDiagnosisandTreat"/> [[In-vitro fertilization]] (IVF) procedures are effective in improving fertility in many women with endometriosis.{{mcn|date=April 2015}} |
|||
==Prognosis== |
|||
Proper counseling of women with endometriosis requires attention to several aspects of the disorder. Of primary importance is the initial operative staging of the disease to obtain adequate information on which to base future decisions about therapy. The woman's symptoms and desire for childbearing dictate appropriate therapy. Not all therapy works for all women. Some women have recurrences after surgery or pseudo-menopause. In most cases, treatment will give women significant relief from pelvic pain and assist them in achieving pregnancy.<ref name=AMN>{{cite web| authors = Memarzadeh S, Muse KN, Fox, MD | title =Endometriosis| work =Differential Diagnosis and Treatment of endometriosis. | url=http://www.health.am/gyneco/endometriosis/ | date= September 21, 2006 | publisher=Armenian Health Network, Health.am | accessdate=2006-12-19}}</ref> |
|||
The underlying process that causes endometriosis may not cease after a surgical or medical intervention. Studies have shown that endometriosis recurs at a rate of 20 to 40 percent within five years following conservative surgery,{{MEDRS|date=April 2015}}<ref>{{MEDRS|date=April 2015}} {{cite web |url=http://my.clevelandclinic.org/disorders/Endometriosis/hic_Recurrent_Endometriosis_Surgical_Management.aspx |title=Recurrent Endometriosis: Surgical Management |date=7 Jan 2010 |work=Endometriosis |publisher=The Cleveland Clinic |accessdate=31 Oct 2010}}</ref> |
|||
unless hysterectomy is performed or menopause reached. Monitoring of women consists of periodic clinical examinations and [[sonography]]. |
|||
Vaginal [[childbirth]] decreases recurrence of endometriosis. In contrast, endometriosis recurrence rates have been shown to be higher in women who have not given birth vaginally, such as in [[cesarean section]].{{MEDRS|date=April 2015}}<ref>{{primary-source inline |date=April 2015}}{{cite journal |vauthors=Bulletti C, Montini A, Setti PL, etal | title = Vaginal parturition decreases recurrence of endometriosis | journal = Fertil. Steril. | volume = 94 | issue = 3 | pages = 850–5 | date = June 2009 | pmid = 19524893 | doi = 10.1016/j.fertnstert.2009.04.012 }}</ref> |
|||
===Complications=== |
|||
Complications of endometriosis include internal scarring, [[adhesions]], pelvic cysts, [[Chocolate cyst of ovary|chocolate cyst of ovaries]], ruptured cysts, and bowel and ureteral obstruction resulting from pelvic adhesions.<ref>{{cite journal |vauthors=Acosta S, Leandersson U, Svensson SE, Johnsen J |title=Fallbeskrivning. Endometrios orsakade kolonileus, uretärobstruktion och hypertoni |trans_title=A case report. Endometriosis caused colonic ileus, ureteral obstruction and hypertension |language=Swedish |journal=Läkartidningen |volume=98 |issue=18 |pages=2208–12 |date=May 2001 |pmid=11402601 |url=http://lup.lub.lu.se/record/1121619}}</ref> [[Endometriosis-associated infertility]] can be related to scar formation and anatomical distortions due to the endometriosis.{{mcn|date=April 2015}} |
|||
Ovarian endometriosis may complicate pregnancy by decidualization,{{clarify|date=April 2015}} abscess and/or rupture.<ref name=Ueda>{{cite journal |vauthors=Ueda Y, Enomoto T, Miyatake T, etal |title=A retrospective analysis of ovarian endometriosis during pregnancy |journal=Fertility and Sterility |volume=94 |issue=1 |pages=78–84 |date=June 2010 |pmid=19356751 |doi=10.1016/j.fertnstert.2009.02.092}}</ref> |
|||
[[Thoracic endometriosis]] is associated with recurrent pneumothoraces at times of a menstrual period, termed [[catamenial pneumothorax]].<ref>{{cite journal |vauthors=Visouli AN, Zarogoulidis K, Kougioumtzi I, etal |title=Catamenial pneumothorax.|journal=Journal of thoracic disease|date=October 2014|volume=6|issue=Suppl 4|pages=S448-60|pmid=25337402|doi=10.3978/j.issn.2072-1439.2014.08.49|pmc=4203986}}</ref> |
|||
==Epidemiology== |
|||
Endometriosis can affect any female, from [[menarche|premenarche]] to [[menopause|postmenopause]], regardless of race or ethnicity or whether or not they have had children. It is primarily a disease of the reproductive years.<ref name=Nothnick>{{cite journal | author = Nothnick WB | title = The emerging use of aromatase inhibitors for endometriosis treatment | journal = Reprod. Biol. Endocrinol. | volume = 9 | issue = | pages = 87 | year = 2011 | pmid = 21693036 | pmc = 3135533 | doi = 10.1186/1477-7827-9-87 }}</ref> The number of women affected is between 6–10%.<ref name=Bulletti2010/> It is more common in women with infertility and chronic pelvic pain (35–50%).<ref name=Bulletti2010/> |
|||
Incidences of endometriosis have occurred in postmenopausal women,<ref name=Medscape>{{cite journal |vauthors=Bulun SE, Zeitoun K, Sasano H, Simpson ER |title=Aromatase in aging women |journal=Seminars in Reproductive Endocrinology |volume=17 |issue=4 |pages=349–58 |year=1999 |pmid=10851574 |doi=10.1055/s-2007-1016244}}</ref> and in less common cases, girls may have endometriosis symptoms before they even reach menarche.<ref>{{cite journal |vauthors=Batt RE, Mitwally MF |title=Endometriosis from thelarche to midteens: pathogenesis and prognosis, prevention and pedagogy |journal=Journal of Pediatric and Adolescent Gynecology |volume=16 |issue=6 |pages=337–47 |date=December 2003 |pmid=14642954 |doi=10.1016/j.jpag.2003.09.008}}</ref><ref>{{cite journal |vauthors=Marsh EE, Laufer MR |title=Endometriosis in premenarcheal girls who do not have an associated obstructive anomaly |journal=Fertility and Sterility |volume=83 |issue=3 |pages=758–60 |date=March 2005 |pmid=15749511 |doi=10.1016/j.fertnstert.2004.08.025}}</ref> |
|||
==History== |
|||
Endometriosis was first discovered microscopically by [[Carl von Rokitansky|Karl von Rokitansky]] in 1860,<ref name=batt>{{cite book|last=Batt|first=Ronald E.|title=A history of endometriosis|year=2011|publisher=Springer|location=London|isbn=978-0-85729-585-9|pages=13–38|url=http://link.springer.com/book/10.1007/978-0-85729-585-9}}</ref> although it was documented in medical texts more than 4,000 years ago.<ref name=nezhat>{{cite journal|vauthors=Nezhat C, Nezhat F, Nezhat C |title=Endometriosis: ancient disease, ancient treatments.|journal=Fertility and Sterility|date=December 2012|volume=98|issue=6 Suppl|pages=S1-62|pmid=23084567|doi=10.1016/j.fertnstert.2012.08.001}}</ref> The [[Hippocratic Corpus]] outlines symptoms similar to endometriosis, including uterine ulcers, adhesions, and infertility.<ref name=nezhat/> Historically, women with these symptoms were treated with [[leech]]es, [[straitjacket]]s, [[bloodletting]], chemical [[douche]]s, [[Female genital mutilation|genital mutilation]], [[pregnancy]] (as a form of treatment), hanging upside down, surgical intervention, and even killing due to suspicion of [[demonic possession]].<ref name=nezhat/> Hippocratic doctors recognized and treated chronic pelvic pain as a true organic disorder 2,500 years ago, but during the Middle Ages, there was a shift into believing that women with pelvic pain were mad, immoral, imagining the pain, or simply misbehaving.<ref name=nezhat/> The symptoms of inexplicable chronic pelvic pain were often attributed to imagined madness, female weakness, promiscuity, or hysteria.<ref name=nezhat/> The historical diagnosis of hysteria, which was thought to be a psychological disease, may have indeed been endometriosis.<ref name=nezhat/> The idea that chronic pelvic pain was related to mental illness influenced modern attitudes regarding women with endometriosis, leading to delays in correct diagnosis and indifference to the patients' true pain during the 20th century.<ref name=nezhat/> |
|||
Hippocratic doctors believed that delaying childbearing could trigger diseases of the uterus, which caused endometriosis-like symptoms. Women with dysmenorrhea were encouraged to marry and have children at a young age.<ref name=nezhat/> The fact that Hippocratics were recommending changes in marriage practices due to an endometriosis-like illness implies that this disease was likely common, with rates higher than the 5-15% prevalence that is often cited today.<ref name=nezhat/> If indeed this disorder was so common historically, this may point away from modern theories that suggest links between endometriosis and dioxins, PCBs, and chemicals.<ref name=nezhat/> |
|||
==Society and culture== |
|||
As recently as 1995, reports found that over 50% of women with chronic pelvic pain had no organic cause, with women still often being considered mentally unstable.<ref name=Gomel>{{page needed|date=April 2015}}{{cite book|vauthors=Gomel V, Taylor PJ |title=Diagnostic and operative gynecologic laparoscopy|date=1995|publisher=Mosby|location=St. Louis, MO}}</ref> Self-help groups say practitioners delay making the diagnosis, often because they don't consider it a possibility. In the US, as of 2007, about 27% of women with endometriosis had had the symptoms for at least six years before it is diagnosed.{{update after|2015|5|20}}<ref name=Atlas>{{cite book|vauthors=Overton C, Davis C, McMillan L, Shaw RW |title=An atlas of endometriosis|date=2007|publisher=Informa Healthcare|location=London|edition=3rd|pages=9–10}}</ref> |
|||
The economic effects associated with endometriosis are substantial and are similar to that of other chronic diseases such as Crohn's disease, diabetes, or rheumatoid arthritis.<ref name=Endoburden>{{cite journal |vauthors=Simoens S, Dunselman G, Dirksen C, etal |title=The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres|journal=Human Reproduction|date=14 March 2012|volume=27|issue=5|pages=1292–1299|doi=10.1093/humrep/des073|pmid=22422778}}</ref> This economic burden is attributed mostly to the inability to consistently work and predicted by decreased quality of life.<ref name=Endoburden/> |
|||
{{trans F}} |
|||
==參考文獻== |
==參考文獻== |
||
{{ |
{{Reflist|30em}} |
||
== 參見 == |
|||
*[[卵巢瘤]] |
|||
== 外部链接 == |
== 外部链接 == |
||
* [http://www.eataiwan.org.tw/ 中華民國子宮內膜異位症婦女協會] |
* [http://www.eataiwan.org.tw/ 中華民國子宮內膜異位症婦女協會] |
||
{{Medical condition classification and resources |
|||
| DiseasesDB = 4269 |
|||
| ICD10 = {{ICD10|N|80||n|80}} |
|||
| ICD9 = {{ICD9|617.0}} |
|||
| ICDO = |
|||
| OMIM = 131200 |
|||
| MedlinePlus = 000915 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 3419 |
|||
| eMedicine_mult = {{eMedicine2|ped|677}} {{eMedicine2|emerg|165}} |
|||
| MeshID = D004715 |
|||
}} |
|||
{{commons category|Endometriosis}} |
|||
*{{dmoz|Health/Women's_Health/Conditions_and_Diseases/Uterus/Endometriosis}} |
|||
* [http://womenshealth.gov/publications/our-publications/fact-sheet/endometriosis.cfm Endometriosis fact sheet] from womenshealth.gov |
|||
{{-}} |
{{-}} |
||
{{女性盆腔和生殖器疾病}} |
{{女性盆腔和生殖器疾病}} |
||
{{Diseases of the pelvis, genitals and breasts}} |
|||
{{Authority control}} |
|||
{{Authority control}} |
{{Authority control}} |
||
[[Category:子宫内膜疾病]] |
[[Category:子宫内膜疾病]] |
||
[[Category:Noninflammatory disorders of female genital tract]] |
|||
[[Category:Menstrual cycle]] |
|||
[[Category:RTT]] |
|||
2017年7月28日 (五) 03:59的版本
| 子宮內膜異位症 Endometriosis | |
|---|---|
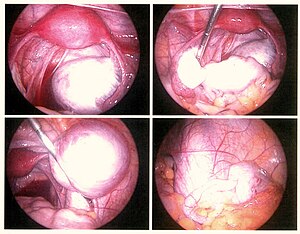 | |
| 利用腹腔鏡手術過程觀察到的巧克力囊腫 | |
| 症状 | 骨盆痛、不孕[1] |
| 起病年龄 | 30–40 歲[2][3] |
| 病程 | 長期[1] |
| 类型 | 女性生殖器畸形[*]、endometrial disease[*]、疾病 |
| 病因 | 未知[1] |
| 风险因素 | 家族病史[2] |
| 診斷方法 | 根據症狀、醫學影像、活體組織切片[2] |
| 鑑別診斷 | 骨盆腔發炎、大腸激躁症、間質性膀胱炎、纤维肌痛[1] |
| 預防 | 复合口服避孕药、運動[2][4] |
| 治療 | NSAIDs、持續服用避孕藥、intrauterine device with progestogen、手術[2] |
| 患病率 | 2000萬 (2015)[5] |
| 死亡數 | ~100 (2015)[6] |
| 分类和外部资源 | |
| 醫學專科 | 婦科學 |
| ICD-11 | GA10 |
| ICD-9-CM | 617、617.9、617.8 |
| OMIM | 131200 |
| DiseasesDB | 4269 |
| MedlinePlus | 000915 |
| eMedicine | 271899、795771 |
| Orphanet | 137820 |
子宮內膜異位症、巧克力囊腫(Endometriosis)為一種婦科疾病,指的是本當存在於子宮內的組織卻在子宮外的其他地方生長[7],主要的症狀有骨盆疼痛以及不孕。有近一半的患者有慢性骨盆疼痛的困擾,更有七成的疼痛感發生在經期,性交時會產生疼痛感的主訴更是常見,有五成的病人更罹患了不孕症[1]。子宮內膜異位症會對病人的社交生活與心靈造成影響[8]。有極少數的病患有排尿或腸部分的病徵。約25%的患者沒有任何症狀[1]。
造成子宮內膜異位症的原因尚未有定論[1],但危險因子包括有家族病史等[9]。大多數的病患在患病後在卵巢、輸卵管和子宮周圍的組織會有感染與影響,而且,甚至有極少數的患者在身體的其他部位也會產生感染[2]。因子宮內膜異位症而每月造成出血的部位會有發炎與留疤的疑慮[1][2],此疾病而促使的細胞生長並不是癌症。診斷常是依據症狀並結合醫學影像技術。活體組織切片是所有檢驗當中最精確的方法[2]。會引起相同症狀的疾病包括有:大腸激躁症、間質性膀胱炎,和纖維肌痛[1]。
一些實驗證據顯示,服用複合口服避孕藥能降低罹患子宮內膜異位症的機率[4],大量的運動以及避免飲用大量酒精飲料也同樣有預防效果[2]。目前沒有針對此症而開發的特效藥,但有多項醫療方法可改善症狀[1] 。上述提到的方法包括有使用止痛藥、賀爾蒙藥物或透過手術來達到幫助病人的目的。推薦患者服用的止痛藥通常為例如萘普生類的非類固醇類抗發炎藥。連續使用避孕藥中的活性成分或裝設子宮內避孕器都視為對抗子宮內膜異位症的有效方法。促性腺刺激素拮抗劑能多少協助因罹患此疾病而不孕的婦女懷孕。對於症狀無法藉由藥物來控制的病患,只能考慮進行手術了[2]。
目前估計約有6-10%的婦女有子宮內膜異位症的困擾[1],病患多為30-40歲的女性[2]。有些微的致死率,而在2013年時,約造成200名患者死亡[10]。1920年代,第一次認定為疾病的一種,在那之前,子宮內膜異位症都覺得和子宮肌腺瘤是相同的,對於誰是第一個明確描述此惡疾的,尚未有一個定論[11]。
Signs and symptoms

Although 20–25% of women with endometriosis have no symptoms, pain and infertility are common signs.[1]
Pelvic pain
A major symptom of endometriosis is recurring pelvic pain. The pain can range from mild to severe cramping or stabbing pain that occurs on both sides of the pelvis, in the lower back and rectal area, and even down the legs. The amount of pain a woman feels correlates poorly with the extent or stage (1 through 4) of endometriosis, with some women having little or no pain despite having extensive endometriosis or endometriosis with scarring, while other women may have severe pain even though they have only a few small areas of endometriosis.[12] Symptoms of endometriosis-related pain may include:[13]
- dysmenorrhea – painful, sometimes disabling cramps during the menstrual period; pain may get worse over time (progressive pain), also lower back pains linked to the pelvis
- chronic pelvic pain – typically accompanied by lower back pain or abdominal pain
- dyspareunia – painful sex
- dysuria – urinary urgency, frequency, and sometimes painful voiding
Throbbing, gnawing, and dragging pain to the legs are reported more commonly by women with endometriosis.[不可靠的醫學來源?][14] Compared with women with superficial endometriosis, those with deep disease appear to be more likely to report shooting rectal pain and a sense of their insides being pulled down.[14] Individual pain areas and pain intensity appear to be unrelated to the surgical diagnosis, and the area of pain unrelated to area of endometriosis.[14]
Endometriosis lesions react to hormonal stimulation and may "bleed" at the time of menstruation. The blood accumulates locally, causes swelling, and triggers inflammatory responses with the activation of cytokines. This process may cause pain. Pain can also occur from adhesions (internal scar tissue) binding internal organs to each other, causing organ dislocation. Fallopian tubes, ovaries, the uterus, the bowels, and the bladder can be bound together in ways that are painful on a daily basis, not just during menstrual periods.[15]
Also, endometriotic lesions can develop their own nerve supply, thereby creating a direct and two-way interaction between lesions and the central nervous system, potentially producing a variety of individual differences in pain that can, in some women, become independent of the disease itself.[12] Nerve fibres and blood vessels are thought to grow into endometriosis lesions by a process known as Neuroangiogenesis.[16]
Infertility
About a third of women with infertility have endometriosis.[1] Among women with endometriosis about 40% are infertile.[1]
Other
Other symptoms include diarrhea or constipation,[不可靠的醫學來源?][14] chronic fatigue,[需要可靠醫學來源] nausea and vomiting, headaches, low-grade fevers, heavy and/or irregular periods, and hypoglycemia.[不可靠的醫學來源?][17]
In addition to pain during menstruation, the pain of endometriosis can occur at other times of the month. There can be a pain with ovulation, pain associated with adhesions, pain caused by inflammation in the pelvic cavity, pain during bowel movements and urination, during general bodily movement like exercise, pain from standing or walking, and pain with intercourse. The most severe pain is typically associated with menstruation. Pain can also start a week before a menstrual period, during and even a week after a menstrual period, or it can be constant. The pain can be debilitating and the emotional stress can take a toll.[18]
There is an association between endometriosis and certain types of cancers, notably some types of ovarian cancer,[19][20] non-Hodgkin's lymphoma and brain cancer.[21] Endometriosis is unrelated to endometrial cancer.[22]
Risk factors
Genetics
Genetic predisposition plays a role in endometriosis.[23] Daughters or sisters of women with endometriosis are at higher risk of developing endometriosis themselves; low progesterone levels may be genetic, and may contribute to a hormone imbalance.[24] There is an about six-fold increased incidence in women with an affected first-degree relative.[25]
It has been proposed that endometriosis results from a series of multiple hits within target genes, in a mechanism similar to the development of cancer.[23] In this case, the initial mutation may be either somatic or heritable.[23]
Individual genomic changes (found by genotyping including genome-wide association studies) that have been associated with endometriosis include:
- Changes on chromosome 1 near WNT4.[26]
- Changes on chromosome 2 near GREB1.[26]
- Changes on chromosome 6 near ID4.[26]
- Changes on chromosome 7 in the 7p15.2 region.[26][27]
- Changes on chromosome 9 near CDKN2BAS.[26]
- Changes on chromosome 10 at region 10q26.[28]
- Changes on chromosome 12 near VEZT.[26]
In addition, there is a weaker association with changes in the fibronectin gene as well as in the 2p14 region of chromosome 2.[26]
In addition, there are many findings of altered gene expression and epigenetics, but both of these can also be a secondary result of, for example, environmental factors and altered metabolism. Examples of altered gene expression include that of miRNAs.[23]
Environmental toxins
Several studies have investigated the potential link between exposure to dioxins and endometriosis, but the evidence is equivocal and potential mechanisms are poorly understood.[29] A 2004 review of studies of dioxin and endometriosis concluded that "the human data supporting the dioxin-endometriosis association are scanty and conflicting",[30] and a 2009 follow-up review also found that there was "insufficient evidence" in support of a link between dioxin exposure and women developing endometriosis.[31] A 2008 review concluded that more work was needed, stating that "although preliminary work suggests a potential involvement of exposure to dioxins in the pathogenesis of endometriosis, much work remains to clearly define cause and effect and to understand the potential mechanism of toxicity".[32]
Pathophysiology

While the exact cause of endometriosis remains unknown, many theories have been presented to better understand and explain its development. These concepts do not necessarily exclude each other. The pathophysiology of endometriosis is likely to be multifactorial and to involve an interplay between several factors.[23]
Formation
The main theories for the formation of the ectopic endometrium are retrograde menstruation, müllerianosis, coelomic metaplasia and transplantation, each further described below.
Retrograde menstruation theory
The theory of retrograde menstruation (also called the implantation theory or transplantation theory)[33] is the most widely accepted theory for the formation of ectopic endometrium in endometriosis.[23] It suggests that during a woman's menstrual flow, some of the endometrial debris exits the uterus through the fallopian tubes and attaches itself to the peritoneal surface (the lining of the abdominal cavity) where it can proceed to invade the tissue as endometriosis.[23]
Retrograde menstruation alone is not able to explain all instances of endometriosis, and additional factors such as genetic or immune differences need to be invoked to account for the fact that many women with retrograde menstruation do not have endometriosis. Researchers are investigating the possibility that the immune system may not be able to cope with the cyclic onslaught of retrograde menstrual fluid. In this context there is interest in studying the relationship of endometriosis to autoimmune disease, allergic reactions, and the impact of toxic materials.[34][35] It is still unclear what, if any, causal relationship exists between toxic materials, autoimmune disease, and endometriosis. There are immune system changes in women with endometriosis, such as an increase macrophage-derived secretion products, but it is unknown if these are contributing to the disorder or are reactions from it.[36]
In addition, at least one study found that endometriotic lesions differ in their biochemistry from artificially transplanted ectopic tissue.[37] This is likely because the cells that give rise to endometriosis are a side population of cells.[23] Similarly, there are changes in for example the mesothelium of the peritoneum in women with endometriosis, such as loss of tight junctions, but it is unknown if these are causes or effects of the disorder.[36]
In rare cases where imperforate hymen does not resolve itself prior to the first menstrual cycle and goes undetected, blood and endometrium are trapped within the uterus of the woman until such time as the problem is resolved by surgical incision. Many health care practitioners never encounter this defect, and due to the flu-like symptoms it is often misdiagnosed or overlooked until multiple menstrual cycles have passed. By the time a correct diagnosis has been made, endometrium and other fluids have filled the uterus and fallopian tubes with results similar to retrograde menstruation resulting in endometriosis. The initial stage of endometriosis may vary based on the time elapsed between onset and surgical procedure.[來源請求]
The theory of retrograde menstruation as a cause of endometriosis was first proposed by John A. Sampson.
Other theories
- Stem cells: Endometriosis may arise from stem cells from bone marrow and potentially other sources. In particular this theory explains endometriosis found in areas remote from the pelvis such as the brain or lungs.[38]
- Environment; Environmental toxins (e.g.; dioxin, nickel) may cause endometriosis.[39][40]
- Müllerianosis: A theory supported by foetal autopsy is that cells with the potential to become endometrial, which are laid down in tracts during embryonic development called the female reproductive (Mullerian) tract as it migrates downward at 8–10 weeks of embryonic life, could become dislocated from the migrating uterus and act like seeds or stem cells.[41]
- Coelomic metaplasia: Coelomic cells which are the common ancestor of endometrial and peritoneal cells may undergo metaplasia (transformation) from one type of cell to the other, perhaps triggered by inflammation.[42]
- Vasculogenesis: Up to 37% of the microvascular endothelium of ectopic endometrial tissue originates from endothelial progenitor cells, which result in de novo formation of microvessels by the process of vasculogenesis rather than the conventional process of angiogenesis.[43][需要解释]
- Neural growth: An increased expression of new nerve fibres is found in endometriosis, but does not fully explain the formation of ectopic endometrial tissue, and is not definitely correlated with the amount of perceived pain.[44][需要解释]
- Autoimmune: Graves disease is an autoimmune disease characterized by hyperthyroidism, goiter, ophthalmopathy, and dermopathy. Women with endometriosis had higher rates of Graves disease. One of these potential links between Graves disease and endometriosis is autoimmunity.[45][46]
Localization
Most endometriosis is found on these structures in the pelvic cavity:[47]
- Ovaries (the most common site)
- Fallopian tubes
- The back of the uterus and the posterior cul-de-sac
- The front of the uterus and the anterior cul-de-sac
- Uterine ligaments such as the broad or round ligament of the uterus
- Pelvic and back wall
- Intestines, most commonly the rectosigmoid
- Urinary bladder and ureters
Rectovaginal or bowel endometriosis affects approximately 5-12% of women with endometriosis, and can cause severe pain with bowel movements.[48]
Endometriosis may spread to the cervix and vagina or to sites of a surgical abdominal incision, known as "scar endometriosis."[49] Risk factors for scar endometriosis include previous abdominal surgeries, such as a hysterotomy or cesarean section, or ectopic pregnancies, salpingostomy puerperal sterilization, laparoscopy, amniocentesis, appendectomy, episiotomy, vaginal hysterectomies, and hernia repair.[50][51][52]
Endometriosis may also present with skin lesions in cutaneous endometriosis.
Less commonly lesions can be found on the diaphragm. Diaphragmatic endometriosis is rare, almost always on the right hemidiaphragm, and may inflict the cyclic pain of the right shoulder just before and during a menstrual period. Rarely, endometriosis can be extraperitoneal and is found in the lungs and CNS.[53]
Diagnosis

A health history and a physical examination can lead the health care practitioner to suspect endometriosis. Although doctors can often feel the endometrial growths during a pelvic exam, and these symptoms may be signs of endometriosis, diagnosis cannot be confirmed by exam only. Use of pelvic ultrasound may identify large endometriotic cysts (called endometriomas). However, smaller endometriosis implants cannot be visualized with ultrasound technique.[來源請求]
Laparoscopy

Laparoscopy, a surgical procedure where a camera is used to look inside the abdominal cavity, is the only way to officially diagnose endometriosis as it permits lesion visualization unless the lesion is visible externally, e.g. an endometriotic nodule in the vagina. If the growths are not visible, a biopsy may be taken to determine the diagnosis.[54] Surgery for diagnoses also allows for surgical treatment of endometriosis at the same time.
To the eye, lesions can appear dark blue, powder-burn black, red, white, yellow, brown or non-pigmented. Lesions vary in size. Some within the pelvis walls may not be visible, as normal-appearing peritoneum of infertile women reveals endometriosis on biopsy in 6–13% of cases.[55] Early endometriosis typically occurs on the surfaces of organs in the pelvic and intra-abdominal areas. Health care providers may call areas of endometriosis by different names, such as implants, lesions, or nodules. Larger lesions may be seen within the ovaries as endometriomas or "chocolate cysts", "chocolate" because they contain a thick brownish fluid, mostly old blood.[來源請求]
Frequently during diagnostic laparoscopy, no lesions are found in women with chronic pelvic pain, a symptom common to other disorders including adenomyosis, pelvic adhesions, pelvic inflammatory disease, congenital anomalies of the reproductive tract, and ovarian or tubal masses.[56]
Staging
Surgically, endometriosis can be staged I–IV by the revised classification of the American Society of Reproductive Medicine from 1997.[57] The process is a complex point system that assesses lesions and adhesions in the pelvic organs, but it is important to note staging assesses physical disease only, not the level of pain or infertility. A person with Stage I endometriosis may have a little disease and severe pain, while a person with Stage IV endometriosis may have severe disease and no pain or vice versa. In principle the various stages show these findings:[來源請求]
- Stage I (Minimal)
- Findings restricted to only superficial lesions and possibly a few filmy adhesions
- Stage II (Mild)
- In addition, some deep lesions are present in the cul-de-sac
- Stage III (Moderate)
- As above, plus the presence of endometriomas on the ovary and more adhesions.
- Stage IV (Severe)
- As above, plus large endometriomas, extensive adhesions.
Markers
An area of research is the search for endometriosis markers.[58]
In 2010 essentially all proposed biomarkers for endometriosis were of unclear medical use, although some appear to be promising.[58] The one biomarker that has been in use over the last 20 years is CA-125.[58] A 2016 review found that in those with symptoms of endometriosis and once ovarian cancer has been ruled out, a positive CA-125 may confirm the diagnosis.[59] Its performance in ruling out endometriosis; however, is low.[59] CA-125 levels appear to fall during endometriosis treatment, but has not shown a correlation with disease response.[58]
Another review in 2011 identified several putative biomarkers upon biopsy, including findings of small sensory nerve fibers or defectively expressed β3 integrin subunit.[60] It has been postulated a future diagnostic tool for endometriosis will consist of a panel of several specific and sensitive biomarkers, including both substance concentrations and genetic predisposition.[58]
Histopathology



Typical endometriotic lesions show histopathologic features similar to endometrium, namely endometrial stroma, endometrial epithelium, and glands that respond to hormonal stimuli. Older lesions may display no glands but hemosiderin deposits (see photomicrograph on right) as residual.[來源請求]
Immunohistochemistry has been found to be useful in diagnosing endometriosis as stromal cells have a peculiar surface antigen, CD10, thus allowing the pathologist go straight to a staining area and hence confirm the presence of stromal cells and sometimes glandular tissue is thus identified that was missed on routine H&E staining.[61][需要較佳来源]
Pain quantification
The most common pain scale for quantification of endometriosis-related pain is the visual analogue scale (VAS); VAS and numerical rating scale (NRS) were the best adapted pain scales for pain measurement in endometriosis. For research purposes, and for more detailed pain measurement in clinical practice, VAS or NRS for each type of typical pain related to endometriosis (dysmenorrhea, deep dyspareunia and non-menstrual chronic pelvic pain), combined with the clinical global impression (CGI) and a quality of life scale, are used.[62]
Prevention
Limited evidence indicates that the use of combined oral contraceptives is associated with a reduced risk of endometriosis.[4]
Management
While there is no cure for endometriosis, there are two types of interventions; treatment of pain and treatment of endometriosis-associated infertility.[63] In many women menopause (natural or surgical) will abate the process.[64] In women in the reproductive years, endometriosis is merely managed: the goal is to provide pain relief, to restrict progression of the process, and to restore or preserve fertility where needed. In younger women, surgical treatment attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue.[65]
In general, the diagnosis of endometriosis is confirmed during surgery, at which time ablative steps can be taken. Further steps depend on circumstances: a woman without infertility can be managed with hormonal medication that suppresses the natural cycle and pain medication, while an infertile woman may be treated expectantly after surgery, with fertility medication, or with IVF. As to the surgical procedure, ablation (or fulguration) of endometriosis (burning and vaporizing the lesions with an electric device) has shown a high rate of short-term recurrence after the procedure. The best surgical procedure with much lower rate of short-term recurrence is to excise (cut and remove) the lesions completely.[需要可靠醫學來源]
Surgery
Conservative treatment consists of the excision of the endometrium, adhesions, resection of endometriomas, and restoration of normal pelvic anatomy as much as is possible.[66] Endometrioma on the ovary of any significant size (Approx. 2 cm +) -sometimes misdiagnosed as ovarian cysts- must be removed surgically because hormonal treatment alone will not remove the full endometrioma cyst, which can progress to acute pain from the rupturing of the cyst and internal bleeding.[需要可靠醫學來源] Laparoscopy, besides being used for diagnosis, can also be used to perform surgery. It's considered a "minimally invasive" surgery because the surgeon makes very small openings (incisions) at (or around) the belly button and lower portion of the belly. A thin telescope-like instrument (the laparoscope) is placed through one incision, which allows the doctor to look for endometriosis using a small camera attached to the laparoscope. Small instruments are inserted through the incisions to remove the endometriosis tissue and adhesions. Because the incisions are very small, there will only be small scars on the skin after the procedure, and all endometriosis can be removed, and women recover from surgery quicker and have a lower risk of adhesions.[67]
55% to 100% of women develop adhesions following pelvic surgery,[68] which can result in infertility, chronic abdominal and pelvic pain, and difficult reoperative surgery. Trehan's temporary ovarian suspension, a technique in which the ovaries are suspended for a week after surgery may be used to reduce the incidence of adhesions after endometriosis surgery.[69][70]
Conservative treatment involves excision of endometriosis while preserving the ovaries and uterus, very important for women wishing to conceive, but may increase the risk of recurrence.[71]
Endometriosis recurrence following conservative surgery is estimated as 21.5% at 2 years and 40-50% at 5 years.[72]
A hysterectomy (removal of the uterus) can be used to treat endometriosis in women who do not wish to conceive. However, this should only be done when combined with removal of the endometriosis by excision, as if endometriosis is not also removed at the time of hysterectomy, pain may persist.[73]
For women with extreme pain, a presacral neurectomy may be very rarely performed where the nerves to the uterus are cut. However, this technique is almost never used due to the high incidence of associated complications including presacral hematoma and irreversible problems with urination and constipation.[73]
Hormones
- Progesterone or progestins: Progesterone counteracts estrogen and inhibits the growth of the endometrium.[74] Such therapy can reduce or eliminate menstruation in a controlled and reversible fashion. Progestins are chemical variants of natural progesterone. An example of a progestin is dienogest (Visanne).
- Avoiding products with xenoestrogens, which have a similar effect to naturally produced estrogen and can increase growth of the endometrium.[需要可靠醫學來源]
- Hormone contraception therapy: Oral contraceptives reduce the menstrual pain associated with endometriosis.[不可靠的醫學來源?][75] They may function by reducing or eliminating menstrual flow and providing estrogen support. Typically, it is a long-term approach.
- Danazol (danocrine) and gestrinone are suppressive steroids with some androgenic activity.[65] Both agents inhibit the growth of endometriosis but their use remains limited as they may cause hirsutism and voice changes.[需要可靠醫學來源]
- Gonadotropin-releasing hormone (GnRH) agonists: These drugs are thought to work by decreasing hormone levels.[76] A 2010 Cochrane review found that GnRH agonists were more effective for pain relief in endometriosis than no treatment or placebo, but were no more effective than danazol or intrauterine progestagen, and had more side effects than danazol.[76]
- Aromatase inhibitors are medications that block the formation of estrogen and have become of interest for researchers who are treating endometriosis.[77]
Other medication
- NSAIDs: Anti-inflammatory. They are commonly used in conjunction with other therapy. For more severe cases narcotic prescription drugs may be used. NSAID injections can be helpful for severe pain or if stomach pain prevents oral NSAID use.
- Opioids: Morphine sulphate tablets and other opioid painkillers work by mimicking the action of naturally occurring pain-reducing chemicals called "endorphins". There are different long acting and short acting medications that can be used alone or in combination to provide appropriate pain control.
- Following laparoscopic surgery women who were given Chinese herbs were reported to have comparable benefits to women with conventional drug treatments, though the journal article that reviewed this study also noted that "the two trials included in this review are of poor methodological quality so these findings must be interpreted cautiously. Better quality randomised controlled trials are needed to investigate a possible role for CHM [Chinese Herbal Medicine] in the treatment of endometriosis."[78]
- Pentoxifylline, an immunomodulating agent, has been theorized to improve pain as well as improve pregnancy rates in women with endometriosis. A 2012 Cochrane review, however, found that there was not enough evidence to support the effectiveness or safety of either of these uses.[79] Current American Congress of Obstetricians and Gynecologists (ACOG) guidelines do not include immune-modulators, such as pentoxifylline, in standard treatment protocols.[80]
- Angiogenesis inhibitors lack clinical evidence of efficacy in endometriosis therapy.[81] Under experimental in vitro and in vivo conditions, compounds that have been shown to exert inhibitory effects on endometriotic lesions include growth factor inhibitors, endogenous angiogenesis inhibitors, fumagillin analogues, statins, cyclo-oxygenase-2 inhibitors, phytochemical compounds, immunomodulators, dopamine agonists, peroxisome proliferator-activated receptor agonists, progestins, danazol and gonadotropin-releasing hormone agonists.[81] However, many of these agents are associated with undesirable side effects and more research is necessary. An ideal therapy would diminish inflammation and underlying symptoms without being contraceptive.[82][83]
The overall effectiveness of manual physical therapy to treat endometriosis has not yet been identified.[84] There is no evidence to support nutritional therapy as effective.
Comparison of interventions
Medicinal and surgical interventions produce roughly equivalent pain-relief benefits. Recurrence of pain was found to be 44 and 53 percent with medicinal and surgical interventions, respectively.[24] Each approach has advantages and disadvantages.[42] Manual therapy showed a decrease in pain for 84 percent of study participants, and a 93 percent improvement in sexual function.[不可靠的醫學來源?][85]
Evidence on how effective medication is for relieving pain associated with endometriosis is limited.[63]
The advantages of surgery are demonstrated efficacy for pain control,[86] it is more effective for infertility than medicinal intervention,[65] it provides a definitive diagnosis,[65] and surgery can often be performed as a minimally invasive (laparoscopic) procedure to reduce morbidity and minimize the risk of post-operative adhesions.[87] Efforts to develop effective strategies to reduce or prevent adhesions have been undertaken, but their formation remain a frequent side effect of abdominal surgery.[68]
The advantages of physical therapy techniques are decreased cost, absence of major side-effects, it does not interfere with fertility, and near-universal increase of sexual function.[85] Disadvantages are that there are no large or long-term studies of its use for treating pain or infertility related to endometriosis.[85]
Treatment of infertility
Surgery is more effective than medicinal intervention for addressing infertility associated with endometriosis.[65] Surgery attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue.[65] In-vitro fertilization (IVF) procedures are effective in improving fertility in many women with endometriosis.[需要可靠醫學來源]
Prognosis
Proper counseling of women with endometriosis requires attention to several aspects of the disorder. Of primary importance is the initial operative staging of the disease to obtain adequate information on which to base future decisions about therapy. The woman's symptoms and desire for childbearing dictate appropriate therapy. Not all therapy works for all women. Some women have recurrences after surgery or pseudo-menopause. In most cases, treatment will give women significant relief from pelvic pain and assist them in achieving pregnancy.[88]
The underlying process that causes endometriosis may not cease after a surgical or medical intervention. Studies have shown that endometriosis recurs at a rate of 20 to 40 percent within five years following conservative surgery,[不可靠的醫學來源?][89] unless hysterectomy is performed or menopause reached. Monitoring of women consists of periodic clinical examinations and sonography.
Vaginal childbirth decreases recurrence of endometriosis. In contrast, endometriosis recurrence rates have been shown to be higher in women who have not given birth vaginally, such as in cesarean section.[不可靠的醫學來源?][90]
Complications
Complications of endometriosis include internal scarring, adhesions, pelvic cysts, chocolate cyst of ovaries, ruptured cysts, and bowel and ureteral obstruction resulting from pelvic adhesions.[91] Endometriosis-associated infertility can be related to scar formation and anatomical distortions due to the endometriosis.[需要可靠醫學來源]
Ovarian endometriosis may complicate pregnancy by decidualization,[需要解释] abscess and/or rupture.[92]
Thoracic endometriosis is associated with recurrent pneumothoraces at times of a menstrual period, termed catamenial pneumothorax.[93]
Epidemiology
Endometriosis can affect any female, from premenarche to postmenopause, regardless of race or ethnicity or whether or not they have had children. It is primarily a disease of the reproductive years.[94] The number of women affected is between 6–10%.[1] It is more common in women with infertility and chronic pelvic pain (35–50%).[1]
Incidences of endometriosis have occurred in postmenopausal women,[95] and in less common cases, girls may have endometriosis symptoms before they even reach menarche.[96][97]
History
Endometriosis was first discovered microscopically by Karl von Rokitansky in 1860,[98] although it was documented in medical texts more than 4,000 years ago.[99] The Hippocratic Corpus outlines symptoms similar to endometriosis, including uterine ulcers, adhesions, and infertility.[99] Historically, women with these symptoms were treated with leeches, straitjackets, bloodletting, chemical douches, genital mutilation, pregnancy (as a form of treatment), hanging upside down, surgical intervention, and even killing due to suspicion of demonic possession.[99] Hippocratic doctors recognized and treated chronic pelvic pain as a true organic disorder 2,500 years ago, but during the Middle Ages, there was a shift into believing that women with pelvic pain were mad, immoral, imagining the pain, or simply misbehaving.[99] The symptoms of inexplicable chronic pelvic pain were often attributed to imagined madness, female weakness, promiscuity, or hysteria.[99] The historical diagnosis of hysteria, which was thought to be a psychological disease, may have indeed been endometriosis.[99] The idea that chronic pelvic pain was related to mental illness influenced modern attitudes regarding women with endometriosis, leading to delays in correct diagnosis and indifference to the patients' true pain during the 20th century.[99]
Hippocratic doctors believed that delaying childbearing could trigger diseases of the uterus, which caused endometriosis-like symptoms. Women with dysmenorrhea were encouraged to marry and have children at a young age.[99] The fact that Hippocratics were recommending changes in marriage practices due to an endometriosis-like illness implies that this disease was likely common, with rates higher than the 5-15% prevalence that is often cited today.[99] If indeed this disorder was so common historically, this may point away from modern theories that suggest links between endometriosis and dioxins, PCBs, and chemicals.[99]
Society and culture
As recently as 1995, reports found that over 50% of women with chronic pelvic pain had no organic cause, with women still often being considered mentally unstable.[100] Self-help groups say practitioners delay making the diagnosis, often because they don't consider it a possibility. In the US, as of 2007, about 27% of women with endometriosis had had the symptoms for at least six years before it is diagnosed.[需要更新][101]
The economic effects associated with endometriosis are substantial and are similar to that of other chronic diseases such as Crohn's disease, diabetes, or rheumatoid arthritis.[102] This economic burden is attributed mostly to the inability to consistently work and predicted by decreased quality of life.[102]
參考文獻
- ^ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J. Assist. Reprod. Genet. August 2010, 27 (8): 441–7. PMC 2941592
 . PMID 20574791. doi:10.1007/s10815-010-9436-1.
. PMID 20574791. doi:10.1007/s10815-010-9436-1.
- ^ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Endometriosis. http://www.womenshealth.gov/. December 5, 2014 [4 March 2015].
- ^ 引用错误:没有为名为
Mc2013的参考文献提供内容 - ^ 4.0 4.1 4.2 Vercellini P, Eskenazi B, Consonni D, Somigliana E, Parazzini F, Abbiati A, Fedele L. Oral contraceptives and risk of endometriosis: a systematic review and meta-analysis. Hum. Reprod. Update. 2011, 17 (2): 159–70. PMID 20833638. doi:10.1093/humupd/dmq042.
- ^ GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England). 8 October 2016, 388 (10053): 1545–1602. ISSN 0140-6736. PMC 5055577
 . PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
- ^ Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England). 8 October 2016, 388 (10053): 1459–1544. ISSN 0140-6736. PMC 5388903
 . PMID 27733281. doi:10.1016/S0140-6736(16)31012-1.
. PMID 27733281. doi:10.1016/S0140-6736(16)31012-1.
- ^ Endometriosis: Overview. 2013-06-24 [4 March 2015].
- ^ Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, Raine-Fenning N. The social and psychological impact of endometriosis on women's lives: A critical narrative review. Human Reproduction Update. 2013, 19 (6): 625–639. PMID 23884896. doi:10.1093/humupd/dmt027.
- ^ Painter, Jodie N.; Anderson, Carl A.; Nyholt, Dale R.; Macgregor, Stuart; Lin, Jianghai; Lee, Sang Hong; Lambert, Ann; Zhao, Zhen Z.; Roseman, Fenella. Genome-wide association study identifies a locus at 7p15.2 associated with endometriosis. Nature Genetics. 2011-01-01, 43 (1): 51–54. ISSN 1546-1718. PMC 3019124
 . PMID 21151130. doi:10.1038/ng.731.
. PMID 21151130. doi:10.1038/ng.731.
- ^ GBD 2013 Mortality and Causes of Death, Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.. Lancet. 17 December 2014. PMID 25530442. doi:10.1016/S0140-6736(14)61682-2.
- ^ Brosens, Ivo. Endometriosis: Science and Practice. John Wiley & Sons. 2012: 3. ISBN 9781444398496.
- ^ 12.0 12.1 Stratton P, Berkley KJ. Chronic pelvic pain and endometriosis: translational evidence of the relationship and implications. Hum. Reprod. Update. 2011, 17 (3): 327–46. PMC 3072022
 . PMID 21106492. doi:10.1093/humupd/dmq050.
. PMID 21106492. doi:10.1093/humupd/dmq050.
- ^ Endometriosis;NIH Pub. No. 02-2413; September 2002
- ^ 14.0 14.1 14.2 14.3 Template:Primary-source inline Ballard K, Lane H, Hudelist G, Banerjee S, Wright J. Can specific pain symptoms help in the diagnosis of endometriosis? A cohort study of women with chronic pelvic pain. Fertil. Steril. June 2010, 94 (1): 20–7. PMID 19342028. doi:10.1016/j.fertnstert.2009.01.164.
- ^ [页码请求]Murray MT, Pizzorno J. The Encyclopedia of Natural Medicine 3rd. New York, NY: Simon and Schuster. 2012.
- ^ Asante. Endometriosis: the role of neuroangiogenesis.. Annu Rev Physiol. 2011, 73: 163–182. PMID 21054165. doi:10.1146/annurev-physiol-012110-142158.
- ^ Arbique D, Carter S, van Sell S. Endometriosis can evade diagnosis: being alert to signs of endometriosis can arrest the disease before it takes over a patient's life. RN. 2008, 71 (9): 28–32. PMID 18833741.
- ^ Colette S, Donnez J. Are aromatase inhibitors effective in endometriosis treatment?. Expert Opin Investig Drugs. July 2011, 20 (7): 917–31. PMID 21529311. doi:10.1517/13543784.2011.581226.
- ^ Pearce CL, Templeman C, Rossing MA, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012, 13 (4): 385–94. PMC 3664011
 . PMID 22361336. doi:10.1016/S1470-2045(11)70404-1.
. PMID 22361336. doi:10.1016/S1470-2045(11)70404-1.
- ^ Nezhat F. Article by Prof. Farr Nezhat, MD, FACOG, FACS, University of Columbia, May 1, 2012
- ^ Audebert A. La femme endométriosique est-elle différente ? [Women with endometriosis: are they different from others?]. Gynécologie, Obstétrique & Fertilité. April 2005, 33 (4): 239–46. PMID 15894210. doi:10.1016/j.gyobfe.2005.03.010 (French).
- ^ Rowlands IJ, Nagle CM, Spurdle AB, Webb PM; Australian National Endometrial Cancer Study Group and Australian Ovarian Cancer Study Group. Gynecological conditions and the risk of endometrial cancer. Gynecol Oncol. Dec 2011, 3: 537–41.
- ^ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 23.7 Fauser BC, Diedrich K, Bouchard P, Domínguez F, Matzuk M, Franks S, Hamamah S, Simón C, Devroey P, Ezcurra D, Howles CM. Contemporary genetic technologies and female reproduction. Hum. Reprod. Update. 2011, 17 (6): 829–47. PMC 3191938
 . PMID 21896560. doi:10.1093/humupd/dmr033.
. PMID 21896560. doi:10.1093/humupd/dmr033.
- ^ 24.0 24.1 Kapoor D, Davila W (2005). Endometriosis, eMedicine.
- ^ Giudice LC, Kao LC. Endometriosis. Lancet. 2004, 364 (9447): 1789–99. PMID 15541453. doi:10.1016/S0140-6736(04)17403-5.
- ^ 26.0 26.1 26.2 26.3 26.4 26.5 26.6 Rahmioglu N, Nyholt DR, Morris AP, et al. Genetic variants underlying risk of endometriosis: insights from meta-analysis of eight genome-wide association and replication datasets. Human Reproduction Update. 2014, 20 (5): 702–716. ISSN 1355-4786. PMC 4132588
 . PMID 24676469. doi:10.1093/humupd/dmu015.
. PMID 24676469. doi:10.1093/humupd/dmu015.
- ^ Painter JN, Anderson CA, Nyholt DR, et al. Genome-wide association study identifies a locus at 7p15.2 associated with endometriosis. Nature Genetics. January 2011, 43 (1): 51–4. PMC 3019124
 . PMID 21151130. doi:10.1038/ng.731.
. PMID 21151130. doi:10.1038/ng.731.
- ^ Treloar SA, Wicks J, Nyholt DR, et al. Genomewide linkage study in 1,176 affected sister pair families identifies a significant susceptibility locus for endometriosis on chromosome 10q26. American Journal of Human Genetics. September 2005, 77 (3): 365–76. PMC 1226203
 . PMID 16080113. doi:10.1086/432960.
. PMID 16080113. doi:10.1086/432960.
- ^ Anger DL, Foster WG. The link between environmental toxicant exposure and endometriosis. Frontiers in Bioscience. 2008, 13: 1578–93. PMID 17981650. doi:10.2741/2782.
- ^ Guo SW. The link between exposure to dioxin and endometriosis: a critical reappraisal of primate data. Gynecologic and Obstetric Investigation. 2004, 57 (3): 157–73. PMID 14739528. doi:10.1159/000076374.
- ^ Guo SW, Simsa P, Kyama CM, et al. Reassessing the evidence for the link between dioxin and endometriosis: from molecular biology to clinical epidemiology. Molecular Human Reproduction. October 2009, 15 (10): 609–24. PMID 19744969. doi:10.1093/molehr/gap075.
- ^ Rier S, Foster WG. Environmental dioxins and endometriosis. Toxicological Sciences. December 2002, 70 (2): 161–70. PMID 12441361. doi:10.1093/toxsci/70.2.161.
- ^ van der Linden PJ. Theories on the pathogenesis of endometriosis. Human reproduction (Oxford, England). 1996,. 11 Suppl 3: 53–65. PMID 9147102. doi:10.1093/humrep/11.suppl_3.53.
- ^ Gleicher N, el-Roeiy A, Confino E, Friberg J. Is endometriosis an autoimmune disease?. Obstet Gynecol. July 1987, 70 (1): 115–22. PMID 3110710.
- ^ Capellino S, Montagna P, Villaggio B, Sulli A, Soldano S, et al. Role of estrogens in inflammatory response: expression of estrogen receptors in peritoneal fluid macrophages from endometriosis. Annals of the New York Academy of Sciences. June 2006, 1069: 263–7. PMID 16855153. doi:10.1196/annals.1351.024.
- ^ 36.0 36.1 Young VJ, Brown JK, Saunders PT, Horne AW. The role of the peritoneum in the pathogenesis of endometriosis. Human Reproduction Update. 2013, 19 (5): 558–569. PMID 23720497. doi:10.1093/humupd/dmt024.
- ^ Redwine DB. Was Sampson wrong?. Fertility and Sterility. October 2002, 78 (4): 686–93. PMID 12372441. doi:10.1016/S0015-0282(02)03329-0.
- ^ Hufnagel, D; Li, F; Cosar, E; Krikun, G; Taylor, HS. The Role of Stem Cells in the Etiology and Pathophysiology of Endometriosis.. Seminars in reproductive medicine. September 2015, 33 (5): 333–40. PMID 26375413. doi:10.1055/s-0035-1564609.
- ^ Bruner-Tran, K.L.; Yeaman, G.R.; Crispens, M.A.; Igarashi, T.M.; Osteen, K.G. Dioxin may promote inflammation-related development of endometriosis.. Fertility and Sterility. 2008, 89: 1287–98. PMC 2430157
 . PMID 18394613. doi:10.1016/j.fertnstert.2008.02.102.
. PMID 18394613. doi:10.1016/j.fertnstert.2008.02.102.
- ^ Yuk, Jin-Sung; Shin, Jong Seung; Shin, Ji-Yeon; Oh, Eunsuk; Kim, Hyunmee; Park, Won I. Nickel Allergy Is a Risk Factor for Endometriosis: An 11-Year Population-Based Nested Case-Control Study. PloS One. 2015, 10 (10): –0139388. ISSN 1932-6203. PMID 26439741. doi:10.1371/journal.pone.0139388.
- ^ Signorile PG, Baldi F, Bussani R, D'Armiento M, De Falco M, Baldi A. Ectopic endometrium in human foetuses is a common event and sustains the theory of müllerianosis in the pathogenesis of endometriosis, a disease that predisposes to cancer. Journal of Experimental & Clinical Cancer Research. April 2009, 28: 49. PMC 2671494
 . PMID 19358700. doi:10.1186/1756-9966-28-49.
. PMID 19358700. doi:10.1186/1756-9966-28-49.
- ^ 42.0 42.1 Diagnosis and Treatment of Endometriosis. American Academy of Family Physicians. 1999-10-15 [2011-07-26].
- ^ Laschke MW, Giebels C, Menger MD. Vasculogenesis: a new piece of the endometriosis puzzle. Hum. Reprod. Update. 2011, 17 (5): 628–36. PMID 21586449. doi:10.1093/humupd/dmr023.
- ^ Morotti M, Vincent K, Brawn J, Zondervan KT, Becker CM. Peripheral changes in endometriosis-associated pain. Human Reproduction Update. 2014, 20 (5): 717–736. ISSN 1355-4786. PMC 4337970
 . PMID 24859987. doi:10.1093/humupd/dmu021.
. PMID 24859987. doi:10.1093/humupd/dmu021.
- ^ Yuk, Jin-Sung; Park, Eun-Ju; Seo, Yong-Soo; Kim, Hee Jin; Kwon, Seon-Young; Park, Won I. Graves Disease Is Associated With Endometriosis: A 3-Year Population-Based Cross-Sectional Study. Medicine. 2016, 95 (10): –2975. ISSN 1536-5964. PMID 26962803. doi:10.1097/MD.0000000000002975.
- ^ Giudice, Linda C; Kao, Lee C. Endometriosis. Lancet. 2004, 364 (9447): 1789–1799. ISSN 1474-547X. PMID 15541453. doi:10.1016/S0140-6736(04)17403-5.
- ^ Jenkins S, Olive DL, Haney AF. Endometriosis: pathogenetic implications of the anatomic distribution. Obstetrics and gynecology. March 1986, 67 (3): 335–8. PMID 3945444.
- ^ Weed JC, Ray JE. Endometriosis of the bowel. Obstetrics and gynecology. May 1987, 69 (5): 727–30. PMID 3574800.
- ^ Uzunçakmak C, Güldaş A, Ozçam H, Dinç K. Scar endometriosis: a case report of this uncommon entity and review of the literature. Case reports in obstetrics and gynecology. 2013, 2013: 386783. PMC 3665185
 . PMID 23762683. doi:10.1155/2013/386783.
. PMID 23762683. doi:10.1155/2013/386783.
- ^ Dwivedi AJ, Agrawal SN, Silva YJ. Abdominal wall endometriomas. Digestive diseases and sciences. February 2002, 47 (2): 456–61. PMID 11855568.
- ^ Kaunitz A, Di Sant'Agnese PA. Needle tract endometriosis: an unusual complication of amniocentesis. Obstetrics and gynecology. December 1979, 54 (6): 753–5. PMID 160025.
- ^ Koger KE, Shatney CH, Hodge K, McClenathan JH. Surgical scar endometrioma.. Surgery, gynecology & obstetrics. September 1993, 177 (3): 243–6. PMID 8356497.
- ^ Daly S. Endometrioma/Endometriosis. WebMD. October 18, 2004 [2006-12-19].
- ^ Office on Women’s Health, U.S. Department of Health and Human Services. (16 July 2012). Endometriosis Fact Sheet. Retrieved from Womenshealth.gov http://www.womenshealth.gov/publications/our-publications/fact-sheet/endometriosis.html
- ^ Nisolle M, Paindaveine B, Bourdon A, Berlière M, Casanas-Roux F, Donnez J. Histologic study of peritoneal endometriosis in infertile women. Fertility and Sterility. June 1990, 53 (6): 984–8. PMID 2351237.
- ^ Practice Committee of the American Society for Reproductive, Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion.. Fertility and Sterility. April 2014, 101 (4): 927–35. PMID 24630080. doi:10.1016/j.fertnstert.2014.02.012.
- ^ American Society For Reproductive M,. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertility and Sterility. May 1997, 67 (5): 817–21. PMID 9130884. doi:10.1016/S0015-0282(97)81391-X.
- ^ 58.0 58.1 58.2 58.3 58.4 May KE, Conduit-Hulbert SA, Villar J, Kirtley S, Kennedy SH, Becker CM. Peripheral biomarkers of endometriosis: a systematic review. Hum. Reprod. Update. 2010, 16 (6): 651–74. PMC 2953938
 . PMID 20462942. doi:10.1093/humupd/dmq009.
. PMID 20462942. doi:10.1093/humupd/dmq009.
- ^ 59.0 59.1 Hirsch, M; Duffy, J; Davis, CJ; Nieves Plana, M; Khan, KS; International Collaboration to Harmonise Outcomes and Measures for, Endometriosis. Diagnostic accuracy of cancer antigen 125 for endometriosis: a systematic review and meta-analysis.. BJOG : an international journal of obstetrics and gynaecology. October 2016, 123 (11): 1761–8. PMID 27173590. doi:10.1111/1471-0528.14055.
- ^ May KE, Villar J, Kirtley S, Kennedy SH, Becker CM. Endometrial alterations in endometriosis: a systematic review of putative biomarkers. Hum. Reprod. Update. 2011, 17 (5): 637–53. PMID 21672902. doi:10.1093/humupd/dmr013.
- ^ http://www.rfay.com.au/docs/cd10poster.pdf
- ^ Bourdel N, Alves J, Pickering G, et al. Systematic review of endometriosis pain assessment: how to choose a scale?. Human Reproduction Update. 2014, 21 (1): 136–152. ISSN 1355-4786. PMID 25180023. doi:10.1093/humupd/dmu046.
- ^ 63.0 63.1 What are the treatments for endometriosis. Eunice Kennedy Shriver National Institute of Child Health and Human Development. [20 August 2013].
- ^ Moen MH, Rees M, Brincat M, et al. EMAS position statement: Managing the menopause in women with a past history of endometriosis. Maturitas. 2010, 67 (1): 94–7. PMID 20627430. doi:10.1016/j.maturitas.2010.04.018.
- ^ 65.0 65.1 65.2 65.3 65.4 65.5 Wellbery C. Diagnosis and treatment of endometriosis. Am Fam Physician. 1999, 60 (6): 1753–62, 1767–8. PMID 10537390.
- ^ Speroff L, Glass RH, Kase NG. Clinical Gynecologic Endocrinology and Infertility 6th. Lippincott Willimas Wilkins. 1999: 1057. ISBN 0-683-30379-1.
- ^ Endometriosis and Infertility: Can Surgery Help? (PDF). American Society for Reproductive Medicine. 2008 [31 Oct 2010].
- ^ 68.0 68.1 Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal Adhesions: Etiology, Pathophysiology, and Clinical Significance. Dig Surgery. 2001, 18 (4): 260–273. PMID 11528133. doi:10.1159/000050149.
- ^ Trehan AK. Temporary ovarian suspension. Gynaecological Endoscopy. 2002, 11 (1): 309–314. doi:10.1046/j.1365-2508.2002.00520.x.
- ^ Abuzeid MI, Ashraf M, Shamma FN. Temporary ovarian suspension at laparoscopy for prevention of adhesions. J Am Assoc Gynecol Laparosc. 2002, 9 (1): 98–102. PMID 11821616.
- ^ Namnoum AB, Hickman TN, Goodman SB, Gehlbach DL, Rock JA. Incidence of symptom recurrence after hysterectomy for endometriosis. Fertility and Sterility. November 1995, 64 (5): 898–902. PMID 7589631.
- ^ Guo SW. Recurrence of endometriosis and its control. Hum. Reprod. Update. 2009, 15 (4): 441–61. PMID 19279046. doi:10.1093/humupd/dmp007.
- ^ 73.0 73.1 Johnson NP, Hummelshoj L. Consensus on current management of endometriosis.. Human Reproduction. June 2013, 28 (6): 1552–68. PMID 23528916. doi:10.1093/humrep/det050.
- ^ Patel B, Elguero S, Thakore S, et al. Role of nuclear progesterone receptor isoforms in uterine pathophysiology. Human Reproduction Update. 2014, 21 (2): 155–173. ISSN 1355-4786. PMC 4366574
 . PMID 25406186. doi:10.1093/humupd/dmu056.
. PMID 25406186. doi:10.1093/humupd/dmu056.
- ^ Template:Primary-source inline Harada T, Momoeda M, Taketani Y, Hoshiai H, Terakawa N. Low-dose oral contraceptive pill for dysmenorrhea associated with endometriosis: a placebo-controlled, double-blind, randomized trial. Fertility and Sterility. November 2008, 90 (5): 1583–8. PMID 18164001. doi:10.1016/j.fertnstert.2007.08.051.
- ^ 76.0 76.1 Brown J, Pan A, Hart RJ. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev. 2010, (12): CD008475. PMID 21154398. doi:10.1002/14651858.CD008475.pub2.
- ^ Attar E, Bulun SE. Aromatase inhibitors: the next generation of therapeutics for endometriosis?. Fertility and Sterility. May 2006, 85 (5): 1307–18. PMID 16647373. doi:10.1016/j.fertnstert.2005.09.064.
- ^ Flower, Andrew; Liu, Jian Ping; Lewith, George; Little, Paul; Li, Qing. Chinese herbal medicine for endometriosis. The Cochrane Database of Systematic Reviews. 2012-05-16, (5): CD006568. ISSN 1469-493X. PMID 22592712. doi:10.1002/14651858.CD006568.pub3.
- ^ Lu D, Song H, Li Y, Clarke J, Shi G. Pentoxifylline for endometriosis.. Cochrane database of systematic reviews (Online). Jan 18, 2012, 1: CD007677. PMID 22258970. doi:10.1002/14651858.CD007677.pub3.
- ^ Practice bulletin no. 114 management of endometriosis. Obstet Gynecol. July 2010, 116 (1): 223–36. PMID 20567196. doi:10.1097/AOG.0b013e3181e8b073.
- ^ 81.0 81.1 Laschke MW, Menger MD. Anti-angiogenic treatment strategies for the therapy of endometriosis. Human Reproduction Update. 2012, 18 (6): 682–702. PMID 22718320. doi:10.1093/humupd/dms026.
- ^ Canny GO, Lessey BA. The role of lipoxin A4 in endometrial biology and endometriosis. Mucosal Immunol. 2013, 6 (3): 439–50. PMC 4062302
 . PMID 23485944. doi:10.1038/mi.2013.9.
. PMID 23485944. doi:10.1038/mi.2013.9.
- ^ Streuli I, de Ziegler D, Santulli P, et al. An update on the pharmacological management of endometriosis. Expert Opin Pharmacother. 2013, 14 (3): 291–305. PMID 23356536. doi:10.1517/14656566.2013.767334.
- ^ Valiani M, Ghasemi N, Bahadoran P, Heshmat R. The effects of massage therapy on dysmenorrhea caused by endometriosis. Iran J Nurs Midwifery Res. 2010, 15 (4): 167–71. PMC 3093183
 . PMID 21589790.
. PMID 21589790.
- ^ 85.0 85.1 85.2 Template:Primary-source inline Wurn BF, Wurn LJ, Patterson K, King CR, Scharf ES. Decreasing dyspareunia and dysmenorrhea in women with endometriosis via a manual physical therapy: Results from two independent studies. Journal of Endometriosis and Pelvic Pain Disorders. 2011, 3: 188–196. doi:10.5301/JE.2012.9088.
- ^ Kaiser A, Kopf A, Gericke C, Bartley J, Mechsner S. The influence of peritoneal endometriotic lesions on the generation of endometriosis-related pain and pain reduction after surgical excision. Arch Gynecol Obstet. 16 January 2009, 280 (3): 369–73. PMID 19148660. doi:10.1007/s00404-008-0921-z.
- ^ Radosa MP, Bernardi TS, Georgiev I, Diebolder H, Camara O, Runnebaum IB. Coagulation versus excision of primary superficial endometriosis: a 2-year follow-up. Eur. J. Obstet. Gynecol. Reprod. Biol. June 2010, 150 (2): 195–8. PMID 20303642. doi:10.1016/j.ejogrb.2010.02.022.
- ^ Memarzadeh S, Muse KN, Fox, MD. Endometriosis. Differential Diagnosis and Treatment of endometriosis. Armenian Health Network, Health.am. September 21, 2006 [2006-12-19].
- ^ [不可靠的醫學來源?] Recurrent Endometriosis: Surgical Management. Endometriosis. The Cleveland Clinic. 7 Jan 2010 [31 Oct 2010].
- ^ Template:Primary-source inlineBulletti C, Montini A, Setti PL, et al. Vaginal parturition decreases recurrence of endometriosis. Fertil. Steril. June 2009, 94 (3): 850–5. PMID 19524893. doi:10.1016/j.fertnstert.2009.04.012.
- ^ Acosta S, Leandersson U, Svensson SE, Johnsen J. Fallbeskrivning. Endometrios orsakade kolonileus, uretärobstruktion och hypertoni [A case report. Endometriosis caused colonic ileus, ureteral obstruction and hypertension]. Läkartidningen. May 2001, 98 (18): 2208–12. PMID 11402601 (Swedish).
- ^ Ueda Y, Enomoto T, Miyatake T, et al. A retrospective analysis of ovarian endometriosis during pregnancy. Fertility and Sterility. June 2010, 94 (1): 78–84. PMID 19356751. doi:10.1016/j.fertnstert.2009.02.092.
- ^ Visouli AN, Zarogoulidis K, Kougioumtzi I, et al. Catamenial pneumothorax.. Journal of thoracic disease. October 2014, 6 (Suppl 4): S448–60. PMC 4203986
 . PMID 25337402. doi:10.3978/j.issn.2072-1439.2014.08.49.
. PMID 25337402. doi:10.3978/j.issn.2072-1439.2014.08.49.
- ^ Nothnick WB. The emerging use of aromatase inhibitors for endometriosis treatment. Reprod. Biol. Endocrinol. 2011, 9: 87. PMC 3135533
 . PMID 21693036. doi:10.1186/1477-7827-9-87.
. PMID 21693036. doi:10.1186/1477-7827-9-87.
- ^ Bulun SE, Zeitoun K, Sasano H, Simpson ER. Aromatase in aging women. Seminars in Reproductive Endocrinology. 1999, 17 (4): 349–58. PMID 10851574. doi:10.1055/s-2007-1016244.
- ^ Batt RE, Mitwally MF. Endometriosis from thelarche to midteens: pathogenesis and prognosis, prevention and pedagogy. Journal of Pediatric and Adolescent Gynecology. December 2003, 16 (6): 337–47. PMID 14642954. doi:10.1016/j.jpag.2003.09.008.
- ^ Marsh EE, Laufer MR. Endometriosis in premenarcheal girls who do not have an associated obstructive anomaly. Fertility and Sterility. March 2005, 83 (3): 758–60. PMID 15749511. doi:10.1016/j.fertnstert.2004.08.025.
- ^ Batt, Ronald E. A history of endometriosis. London: Springer. 2011: 13–38. ISBN 978-0-85729-585-9.
- ^ 99.00 99.01 99.02 99.03 99.04 99.05 99.06 99.07 99.08 99.09 Nezhat C, Nezhat F, Nezhat C. Endometriosis: ancient disease, ancient treatments.. Fertility and Sterility. December 2012, 98 (6 Suppl): S1–62. PMID 23084567. doi:10.1016/j.fertnstert.2012.08.001.
- ^ [页码请求]Gomel V, Taylor PJ. Diagnostic and operative gynecologic laparoscopy. St. Louis, MO: Mosby. 1995.
- ^ Overton C, Davis C, McMillan L, Shaw RW. An atlas of endometriosis 3rd. London: Informa Healthcare. 2007: 9–10.
- ^ 102.0 102.1 Simoens S, Dunselman G, Dirksen C, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Human Reproduction. 14 March 2012, 27 (5): 1292–1299. PMID 22422778. doi:10.1093/humrep/des073.
參見
外部链接
| |||||||
- 开放目录项目中的“子宮內膜異位症”
- Endometriosis fact sheet from womenshealth.gov
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||
| |||||||||||||||||
