舍曲林
| 此條目需要更新。 (2018年8月10日) |
 | |
 | |
| 臨床資料 | |
|---|---|
| 商品名 | 左洛復(Zoloft),彼邁樂,樂復得, Lustral 等等[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697048 |
| 懷孕分級 |
|
| 給藥途徑 | 口服 |
| ATC碼 | |
| 法律規範狀態 | |
| 法律規範 |
|
| 藥物動力學數據 | |
| 生物利用度 | 44% |
| 血漿蛋白結合率 | 98.5% |
| 藥物代謝 | 肝臟(主要由CYP2B6酶進行N-去甲基化)[4] |
| 生物半衰期 | ~23-26小時(低活性的代謝產物去甲基舍曲林則為66小時)[2][3] |
| 排泄途徑 | 尿液 |
| 識別資訊 | |
| |
| CAS號 | 79617-96-2 |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| 化學資訊 | |
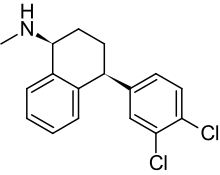
| 化學式 | C17H17Cl2N |
| 摩爾質量 | 306.229 g/mol |
| 3D模型(JSmol) | |
| |
| |
舍曲林與其他新型抗抑鬱藥的差別並不大,並且多隻局限於副作用。與其他SSRI相比,舍曲林的耐受性與其他藥物無明顯差別,通常都會導致一些不良反應如腹瀉、噁心、震顫、性功能障礙和體重增加。舍曲林導致腹瀉的幾率通常比其他SSRI要高。[7]
醫療用途[編輯]
舍曲林適用於多種情況包括:重度抑鬱症(MDD)、強迫症(OCD)、軀體變形障礙(BDD)、創傷後應激障礙(PTSD)、經前煩躁症(PMDD)、恐慌症和焦慮症。舍曲林也用來治療早泄與血管性頭痛,但是還沒有足夠充分的證據證明它的效果。[8]
抑鬱症[編輯]
一份2008年的報告指出只有51%的研究表明SSRI有積極效果。[9] 舍曲林的效果在統計學上與其他SSRI無明顯差別,如帕羅西汀、西酞普蘭、艾司西酞普蘭、文拉法辛(屬於SNRI)等。[10][11][12][13] 證據表明在治療某些抑鬱症亞型上,舍曲林比氟西汀(百優解)效果更明顯。[14]
證據指出舍曲林對兒童抑鬱症的治療沒有好處。[15]
對於伴隨痴呆的抑鬱症,舍曲林並不優於安慰劑或米氮平。[16]
對比其他抗抑鬱藥[編輯]
一般認為三環類抗抑鬱藥(TCA)在治療憂鬱型抑鬱症和住院病人上效果比SSRI更好,但並不一定對更加嚴重的抑鬱症也有更好的效果。[17][18][19] 總的來說,舍曲林在治療住院病人上並不優於安慰劑,在治療重度抑鬱症上與TCA類藥物氯米帕明效果相當。[10] 尚未有針對在治療憂鬱型抑鬱症上舍曲林與TCA的效果對比的研究。1998年有一種觀點認為,由於舍曲林的藥理特性,其在效果上會優於其他SSRI且在治療憂鬱型抑鬱症上與TCA類藥物效果相同。[20]
針對12種新型抗抑鬱藥的數據分析指出,舍曲林與艾司西酞普蘭在治療成人急性單極抑鬱症上有着最好的效果和可接受性,而瑞波西汀的效果明顯較差。[21]
具有比較性的臨床試驗表明,舍曲林治療抑鬱症的效果與嗎氯貝胺、奈法唑酮、艾司西酞普蘭、安非他酮、西酞普蘭、氟伏沙明、帕羅西汀、米氮平相似。有質量較低的證據表明,舍曲林治療抑鬱症的效果優於氟西汀。[22][23][24][25][26]
針對老年患者[編輯]
舍曲林在治療老年患者(大於60歲)的效果上優於安慰劑,與其它SSRI類藥物氟西汀和TCA類藥物阿米替林、去甲替林、丙咪嗪效果相當。除噁心外,舍曲林的不良反應發生率低於這些TCA類藥物。此外,針對大於70歲的患者,舍曲林的效果優於氟西汀和去甲替林。[27]2003年的一項關於舍曲林與安慰劑的對比試驗得出一個具有統計學上顯著(也就是說不只是偶然發生)並且具有臨床意義的結論,老年患者使用舍曲林後抑鬱症狀有適度改善,但是生活質量並沒有得到提高。[28]
強迫症[編輯]
舍曲林對成人及兒童的強迫症治療均有效果。[29]基於意向性治療分析,舍曲林相比強迫症治療金標準氯米帕明有着更好的效果。[30]普遍認為舍曲林用於治療強迫症的劑量比治療抑鬱症的常用劑量高。[31]舍曲林治療強迫症的起效時間比治療抑鬱症長。治療的建議是,以最大推薦劑量的一半最為起始劑量並持續至少兩個月,在此之後如果治療效果不明顯,可將劑量提高至最大。[32]
無論是兒童還是成人,單獨應用行為認知療法的效果優於舍曲林,但是最好的方法當然是結合藥物治療。[33][34]舍曲林可能對伴隨抽動穢語綜合症的強迫症有療效。[35]
恐慌症[編輯]
使用舍曲林治療恐慌症可以減少驚恐發作並提高生活質量。[36] 四個雙盲實驗顯示出舍曲林在治療恐慌症時效果優於安慰劑,效果取決於劑量。舍曲林可以減少80%驚恐發作的幾率(安慰劑為45%),並且可以減少廣泛性焦慮,提升患者的生活質量。使用舍曲林的患者報告生活質量的提高程度優於安慰劑組。[36][37] 性別不會影響舍曲林的效果。[37] 如果粗略地將舍曲林與其他抗恐慌症藥物(如氯米帕明、丙咪嗪、氯硝西泮、阿普唑侖、氟伏沙明、帕羅西汀)進行單獨比較,那麼他們的效果是接近等價。[36]
其他焦慮症[編輯]
舍曲林可有效治療社交恐怖症。[38] Lielowitz社交焦慮量表得分的改善與舍曲林有關,但與安慰劑無關。[39]在兒童中,舍曲林和認知行為療法(CBT)的組合對焦慮症患兒具有優異的反應率;舍曲林和CBT單獨治療也均優於安慰劑,並且彼此之間沒有顯著差異。[40]
有初步證據表明,舍曲林以及其他SSRI / SNRI抗抑鬱藥可以幫助治療一般焦慮症的症狀。[41]
經前焦慮症[編輯]
包括舍曲林在內的SSRI類藥物可以減輕經前症狀。[42]常見的不良反應有噁心等。[42]
舍曲林對緩解經前焦慮症(Premenstrual dysphoric disorder,PMDD),即為重度的經前症狀,效果明顯。經過舍曲林治療的人症狀得到明顯改善,50-60%的人症狀得到改善,而安慰劑只有20-30%。開始治療一個星期內症狀即會有明顯好轉,包括精神狀態,易怒,焦慮等都有明顯改善,這些好轉還能增進家庭的和睦,社交和生活質量的提高。但是像工作能力,身體症狀,如腫脹、腹脹和乳汁不足的症狀並對藥物並沒有明顯的反應。[43][44] 在黃體期,即經前12-14天服用舍曲林達到的治療效果與在臨近經前時才開始服用基本相當。[42]
其他適應症[編輯]
每日口服舍曲林可以治療早發性射精(早泄、PE)。[45] SSRI類藥物治療早泄的缺點是需要長期給藥才會有顯著效果,並且目前還不清楚SSRI會對早泄或無法控制射精的患者造成怎樣的心理困擾。[46][47]
已知可能後遺症[編輯]
PSSD(Post-SSRIs sexual dysfunction):SSRI後的性功能障礙
不良反應[編輯]


自殺傾向[編輯]
FDA要求包括舍曲林在內的所有抗抑鬱藥都要用黑框警告說明抗抑鬱藥會增加25歲以下服用者自殺的風險。此項警告的依據為兩個獨立的FDA專家組的統計分析,結果顯示兒童和青少年產生自殺意向和行為的幾率提高兩倍,18-24歲的人群則提高1.5倍。[48][49][50]
過量服用[編輯]
急性過量服用舍曲林的症狀通常為嘔吐、嗜睡,運動失調,心動過速和癲癇發作。血漿、血清或血液中舍曲林和去甲基舍曲林(舍曲林的活性代謝產物)是診斷是否過量服用的標誌,也可以幫助法醫進行死因調查。[51] 與其他大部分SSRI一樣,舍曲林服用過量的毒性是相對較小的。[52][53]
作用機制[編輯]
舍曲林主要是一種5-羥色胺再攝取抑制劑,對5-羥色胺轉運體的親和力是Ki=2.0μM.[54] 在服用4周治療劑量的舍曲林 (25–200 mg/天) 後,通過正電子發射斷層掃描測量紋狀體得知,舍曲林抑制80–90%的5-羥色胺轉運體。每日9mg劑量時則抑制50%的5-羥色胺轉運體。[55]
藥代動力學[編輯]

舍曲林口服吸收緩慢,在4-6小時時達到最大血藥濃度。舍曲林在血液中的蛋白結合度為98.5%。舍曲林在體內的生物半衰期為13-45小時,並且平均女性(32小時)比男性(22小時)長1.5倍。 [56]體外研究顯示,舍曲林由多種細胞色素P450同工酶代謝,包括:CYP2D6, CYP2C9, CYP2B6, CYP2C19和CYP3A4。但是對上述任意一種同工酶的抑制都不能使舍曲林的藥代動力學數據發生具有臨床意義的改變。[4][57] CYP2D6活性不同的人對舍曲林的代謝無影響,[58] 然而,低活性的CYP2C19會使舍曲林的代謝時間延長1.5倍。[59][4] [4][60]
舍曲林的非胺類代謝產物也具有抗抑鬱作用。脫氨基舍曲林代號為O-2098,儘管它並沒有氮原子,但是體外研究仍表明其具有抑制多巴胺再攝取的作用。[61]
舍曲林的首要代謝產物,諾舍特拉林(norsertraline/N-去甲舍曲林),是一種生物活性比舍曲林低很多的物質。[62]
參見[編輯]
引用[編輯]
- ^ drugs.com drugs.com international Sertraline (頁面存檔備份,存於互聯網檔案館) Page accessed May 11, 2015
- ^ Sertraline FDA Label. http://www.fda.gov/ohrms/dockets/ac/04/briefing/4006b1_06_zoloft-label.pdf (頁面存檔備份,存於互聯網檔案館)
- ^ Brunton L, Chabner B, Knollman B. Goodman and Gilman’s The Pharmacological Basis of Therapeutics, Twelfth Edition. McGraw Hill Professional; 2010.
- ^ 4.0 4.1 4.2 4.3 Obach RS, Cox LM, Tremaine LM. Sertraline is metabolized by multiple cytochrome P450 enzymes, monoamine oxidases, and glucuronyl transferases in human: an in vitro study. Drug Metab. Dispos. 2005, 33 (2): 262–70. PMID 15547048. doi:10.1124/dmd.104.002428.
- ^ 史有為主編. 舍曲林. 商務印書館辭書研究中心 (編). 新华外来词词典. 北京: 商務印書館: 1011. 2019. ISBN 978-7-100-16091-9.
- ^ John M. Grohol. Top 25 Psychiatric Medication Prescriptions for 2013. Psych Central. 2014 [3 April 2015]. (原始內容存檔於2015-03-31).
- ^ Sanchez, C; Reines, E. H.; Montgomery, S. A. A comparative review of escitalopram, paroxetine, and sertraline: are they all alike?. International Clinical Psychopharmacology. 2014, 29 (4): 185–196. PMC 4047306
 . PMID 24424469. doi:10.1097/YIC.0000000000000023.
. PMID 24424469. doi:10.1097/YIC.0000000000000023.
- ^ Sertraline hydrochloride. The American Society of Health-System Pharmacists. [3 April 2011]. (原始內容存檔於2016-03-08).
- ^ Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R; Matthews; Linardatos; Tell; Rosenthal. Selective publication of antidepressant trials and its influence on apparent efficacy. N. Engl. J. Med. 2008, 358 (3): 252–60. PMID 18199864. doi:10.1056/NEJMsa065779.
- ^ 10.0 10.1 Lépine JP, Goger J, Blashko C, Probst C, Moles MF, Kosolowski J, Scharfetter B, Lane RM; Goger; Blashko; Probst; Moles; Kosolowski; Scharfetter; Lane. A double-blind study of the efficacy and safety of sertraline and clomipramine in outpatients with severe major depression. International Clinical Psychopharmacology. 2000, 15 (5): 263–71. PMID 10993128. doi:10.1097/00004850-200015050-00003.
- ^ Aberg-Wistedt A, Agren H, Ekselius L, Bengtsson F, Akerblad AC; Agren; Ekselius; Bengtsson; Akerblad. Sertraline versus paroxetine in major depression: clinical outcome after six months of continuous therapy. J Clin Psychopharmacol. 20 December 2000, 20 (6): 645–52. PMID 11106136. doi:10.1097/00004714-200012000-00010.
- ^ Ventura D, Armstrong EP, Skrepnek GH, Haim Erder M; Armstrong; Skrepnek; Haim Erder. Escitalopram versus sertraline in the treatment of major depressive disorder: a randomized clinical trial. Current Medical Research and Opinion. 2007, 23 (2): 245–50. PMID 17288677. doi:10.1185/030079906X167273.
- ^ Matreja, P. S.; Badyal, D. K.; Khosla, P; Deswal, R. S. Effectiveness and acceptability of sertraline and citalopram in major depressive disorder: pragmatic randomized open-label comparison. Hum Psychopharmacol. 22 October 2007, 22 (7): 477–82. PMID 17647298. doi:10.1002/hup.864.
- ^ Flament MF, Lane RM, Zhu R, Ying Z; Lane; Zhu; Ying. Predictors of an acute antidepressant response to fluoxetine and sertraline. Int Clin Psychopharmacol. 1999, 14 (5): 259–75. PMID 10529069. doi:10.1097/00004850-199914050-00001.
- ^ Cohen D. Should the use of selective serotonin reuptake inhibitors in child and adolescent depression be banned?. Psychotherapy and psychosomatics. 2007, 76 (1): 5–14. PMID 17170559. doi:10.1159/000096360.
- ^ Banerjee S, Hellier J, Romeo R, Dewey M, Knapp M, Ballard C, Baldwin R, Bentham P, Fox C, Holmes C, Katona C, Lawton C, Lindesay J, Livingston G, McCrae N, Moniz-Cook E, Murray J, Nurock S, Orrell M, O'Brien J, Poppe M, Thomas A, Walwyn R, Wilson K, Burns A; Hellier; Romeo; Dewey; Knapp; Ballard; Baldwin; Bentham; Fox; Holmes; Katona; Lawton; Lindesay; Livingston; McCrae; Moniz-Cook; Murray; Nurock; Orrell; O'Brien; Poppe; Thomas; Walwyn; Wilson; Burns. Study of the use of antidepressants for depression in dementia: the HTA-SADD trial – a multicentre, randomised, double-blind, placebo-controlled trial of the clinical effectiveness and cost-effectiveness of sertraline and mirtazapine. Health Technol Assess. 2007, 17 (7): 1–116. PMID 23438937. doi:10.3310/hta17070.
- ^ Parker G, Roy K, Wilhelm K, Mitchell P; Roy; Wilhelm; Mitchell. Assessing the comparative effectiveness of antidepressant therapies: a prospective clinical practice study. J Clin Psychiatry. 2001, 62 (2): 117–25. PMID 11247097. doi:10.4088/JCP.v62n0209.
- ^ Anderson IM. SSRIS versus tricyclic antidepressants in depressed inpatients: a meta-analysis of efficacy and tolerability. Depress Anxiety. 1998, 7 (S1): 11–7. PMID 9597346. doi:10.1002/(SICI)1520-6394(1998)7:1+<11::AID-DA4>3.0.CO;2-I.
- ^ Hirschfeld RM. Efficacy of SSRIs and newer antidepressants in severe depression: comparison with TCAs. J Clin Psychiatry. 1999, 60 (5): 326–35. PMID 10362442. doi:10.4088/JCP.v60n0511.
- ^ Amsterdam JD. Selective serotonin reuptake inhibitor efficacy in severe and melancholic depression. J. Psychopharmacol. (Oxford). 1998, 12 (3 Suppl B): S99–111. PMID 9808081. doi:10.1177/0269881198012003061 (不活躍 2015-05-19).
- ^ Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C; Furukawa; Salanti; Geddes; Higgins; Churchill; Watanabe; Nakagawa; Omori; McGuire; Tansella; Barbui. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. The Lancet. 2009, 373 (9665): 746–758. PMID 19185342. doi:10.1016/S0140-6736(09)60046-5. 簡明摘要 – The Washington Post (29 January 2009).
- ^ Papakostas GI, Fava M; Fava. A metaanalysis of clinical trials comparing moclobemide with selective serotonin reuptake inhibitors for the treatment of major depressive disorder. Canadian Journal of Psychiatry. 2006, 51 (12): 783–90. PMID 17168253.
- ^ Feiger A, Kiev A, Shrivastava RK, Wisselink PG, Wilcox CS; Kiev; Shrivastava; Wisselink; Wilcox. Nefazodone versus sertraline in outpatients with major depression: focus on efficacy, tolerability, and effects on sexual function and satisfaction. The Journal of Clinical Psychiatry. 57. 1996,. Suppl 2: 53–62. PMID 8626364.
- ^ Kavoussi RJ, Segraves RT, Hughes AR, Ascher JA, Johnston JA; Segraves; Hughes; Ascher; Johnston. Double-blind comparison of bupropion sustained release and sertraline in depressed outpatients. The Journal of Clinical Psychiatry. 1997, 58 (12): 532–7. PMID 9448656. doi:10.4088/JCP.v58n1204.
- ^ For the review, see:Hansen RA, Gartlehner G, Lohr KN, Gaynes BN, Carey TS; Gartlehner; Lohr; Gaynes; Carey. Efficacy and safety of second-generation antidepressants in the treatment of major depressive disorder. Ann. Intern. Med. 2005, 143 (6): 415–26. PMID 16172440. doi:10.7326/0003-4819-143-6-200509200-00006.
- ^ Cipriani, A; La Ferla, T; Furukawa, TA; Signoretti, A; Nakagawa, A; Churchill, R; McGuire, H; Barbui, C. Sertraline versus other antidepressive agents for depression. The Cochrane database of systematic reviews. 14 April 2010, (4): CD006117. PMC 4163971
 . PMID 20393946. doi:10.1002/14651858.CD006117.pub4.
. PMID 20393946. doi:10.1002/14651858.CD006117.pub4.
- ^ Muijsers RB, Plosker GL, Noble S; Plosker; Noble. Sertraline: a review of its use in the management of major depressive disorder in elderly patients. Drugs & Aging. 2002, 19 (5): 377–92. PMID 12093324. doi:10.2165/00002512-200219050-00006.
- ^ Schneider LS, Nelson JC, Clary CM, Newhouse P, Krishnan KR, Shiovitz T, Weihs K; Nelson; Clary; Newhouse; Krishnan; Shiovitz; Weihs; Sertraline Elderly Depression Study Group. An 8-week multicenter, parallel-group, double-blind, placebo-controlled study of sertraline in elderly outpatients with major depression. Am J Psychiatry. 2003, 160 (7): 1277–85. PMID 12832242. doi:10.1176/appi.ajp.160.7.1277.
- ^ Geller DA, Biederman J, Stewart SE, Mullin B, Martin A, Spencer T, Faraone SV; Biederman; Stewart; Mullin; Martin; Spencer; Faraone. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. The American Journal of Psychiatry. 2003, 160 (11): 1919–28. PMID 14594734. doi:10.1176/appi.ajp.160.11.1919.
- ^ Flament MF, Bisserbe JC; Bisserbe. Pharmacologic treatment of obsessive-compulsive disorder: comparative studies. The Journal of Clinical Psychiatry. 58. 1997,. Suppl 12: 18–22. PMID 9393392.
- ^ Math SB, Janardhan Reddy YC. Issues In The Pharmacological Treatment of Obsessive-Compulsive Disorder: First-Line Treatment Options for OCD. medscape.com. 19 July 2007 [28 July 2009]. (原始內容存檔於2021-01-25).
- ^ Blier P, Habib R, Flament MF; Habib; Flament. Pharmacotherapies in the management of obsessive-compulsive disorder (PDF). Can J Psychiatry. 2006, 51 (7): 417–30. PMID 16838823. (原始內容 (PDF)存檔於2010-02-04).
- ^ Pediatric OCD Treatment Study (POTS) Team. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004, 292 (16): 1969–76. PMID 15507582. doi:10.1001/jama.292.16.1969.
- ^ Sousa MB, Isolan LR, Oliveira RR, Manfro GG, Cordioli AV; Isolan; Oliveira; Manfro; Cordioli. A randomized clinical trial of cognitive-behavioral group therapy and sertraline in the treatment of obsessive-compulsive disorder. The Journal of Clinical Psychiatry. 2006, 67 (7): 1133–9. PMID 16889458. doi:10.4088/JCP.v67n0717.
- ^ Jiménez-Jiménez FJ, García-Ruiz PJ; García-Ruiz. Pharmacological options for the treatment of Tourette's disorder. Drugs. 2001, 61 (15): 2207–20. PMID 11772131. doi:10.2165/00003495-200161150-00005.
- ^ 36.0 36.1 36.2 Hirschfeld RM. Sertraline in the treatment of anxiety disorders. Depress Anxiety. 2000, 11 (4): 139–57. PMID 10945134. doi:10.1002/1520-6394(2000)11:4<139::AID-DA1>3.0.CO;2-C.
- ^ 37.0 37.1 Clayton AH, Stewart RS, Fayyad R, Clary CM; Stewart; Fayyad; Clary. Sex differences in clinical presentation and response in panic disorder: pooled data from sertraline treatment studies. Arch Womens Ment Health. 2006, 9 (3): 151–7. PMID 16292466. doi:10.1007/s00737-005-0111-y.
- ^ Hansen, Richard A.; Gaynes, Bradley N.; Gartlehner, Gerald; Moore, Charity G.; Tiwari, Ruchi; Lohr, Kathleen N. Efficacy and Tolerability of Second-Generation Antidepressants in Social Anxiety Disorder. International clinical psychopharmacology. 2008-05, 23 (3): 170–179 [2019-03-30]. ISSN 0268-1315. PMC 2657552
 . PMID 18408531. doi:10.1097/YIC.0b013e3282f4224a. (原始內容存檔於2022-05-04).
. PMID 18408531. doi:10.1097/YIC.0b013e3282f4224a. (原始內容存檔於2022-05-04).
- ^ Hansen, Richard A.; Gaynes, Bradley N.; Gartlehner, Gerald; Moore, Charity G.; Tiwari, Ruchi; Lohr, Kathleen N. Efficacy and Tolerability of Second-Generation Antidepressants in Social Anxiety Disorder. International clinical psychopharmacology. 2008-05, 23 (3): 170–179 [2019-03-30]. ISSN 0268-1315. PMC 2657552
 . PMID 18408531. doi:10.1097/YIC.0b013e3282f4224a. (原始內容存檔於2022-05-04).
. PMID 18408531. doi:10.1097/YIC.0b013e3282f4224a. (原始內容存檔於2022-05-04).
- ^ Walkup, John T.; Albano, Anne Marie; Piacentini, John; Birmaher, Boris; Compton, Scott N.; Sherrill, Joel T.; Ginsburg, Golda S.; Rynn, Moira A.; McCracken, James. Cognitive Behavioral Therapy, Sertraline, or a Combination in Childhood Anxiety. The New England journal of medicine. 2008-12-25, 359 (26): 2753–2766 [2019-03-30]. ISSN 0028-4793. PMC 2702984
 . PMID 18974308. doi:10.1056/NEJMoa0804633. (原始內容存檔於2022-06-22).
. PMID 18974308. doi:10.1056/NEJMoa0804633. (原始內容存檔於2022-06-22).
- ^ Gale, Christopher K; Millichamp, Jane. Generalised anxiety disorder. BMJ Clinical Evidence. 2011-10-27, 2011 [2019-03-30]. ISSN 1752-8526. PMC 3275153
 . PMID 22030083. (原始內容存檔於2022-05-09).
. PMID 22030083. (原始內容存檔於2022-05-09).
- ^ 42.0 42.1 42.2 Marjoribanks J, Brown J, O'Brien PM, Wyatt K; Brown; O'Brien; Wyatt. Selective serotonin reuptake inhibitors for premenstrual syndrome. The Cochrane database of systematic reviews. 7 June 2013, 6: CD001396. PMID 23744611. doi:10.1002/14651858.cd001396.pub3.
- ^ Pearlstein T. Selective serotonin reuptake inhibitors for premenstrual dysphoric disorder: the emerging gold standard?. Drugs. 2002, 62 (13): 1869–85. PMID 12215058. doi:10.2165/00003495-200262130-00004.
- ^ Ackermann RT, Williams JW; Williams Jr. Rational treatment choices for non-major depressions in primary care: an evidence-based review. J Gen Intern Med. 2002, 17 (4): 293–301. PMC 1495030
 . PMID 11972726. doi:10.1046/j.1525-1497.2002.10350.x.
. PMID 11972726. doi:10.1046/j.1525-1497.2002.10350.x.
- ^ Abdel-Hamid IA. Pharmacologic treatment of rapid ejaculation: levels of evidence-based review.. Current clinical pharmacology. September 2006, 1 (3): 243–54. PMID 18666749. doi:10.2174/157488406778249352.
- ^ Waldinger MD. Premature ejaculation: state of the art. Urol. Clin. North Am. 2007, 34 (4): 591–9, vii–viii. PMID 17983899. doi:10.1016/j.ucl.2007.08.011.
- ^ McMahon CG, Porst H; Porst. Oral agents for the treatment of premature ejaculation: review of efficacy and safety in the context of the recent International Society for Sexual Medicine criteria for lifelong premature ejaculation. The journal of sexual medicine. October 2011, 8 (10): 2707–25. PMID 21771283. doi:10.1111/j.1743-6109.2011.02386.x.
- ^ Levenson M, Holland C. Antidepressants and Suicidality in Adults: Statistical Evaluation. (Presentation at Psychopharmacologic Drugs Advisory Committee; December 13, 2006). FDA. [11 July 2008]. (原始內容存檔於2017-05-17).
- ^ Stone MB, Jones ML. Clinical review: relationship between antidepressant drugs and suicidality in adults (PDF). Overview for December 13 Meeting of Psychopharmacologic Drugs Advisory Committee (PDAC). FDA: 11–74. 17 November 2006 [11 July 2008]. (原始內容存檔 (PDF)於2007-03-16).
- ^ Levenson M, Holland C. Statistical Evaluation of Suicidality in Adults Treated with Antidepressants (PDF). Overview for December 13 Meeting of Psychopharmacologic Drugs Advisory Committee (PDAC). FDA: 75–140. 17 November 2006 [11 July 2008]. (原始內容存檔 (PDF)於2007-03-16).
- ^ R. Baselt. Disposition of Toxic Drugs and Chemicals in Man 8th. Foster City, California: Biomedical Publications. 2008: 1399–1400.
- ^ Taylor, D; Paton, C; Shitij, K. The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. 2012. ISBN 978-0-470-97948-8.
- ^ White N, Litovitz T, Clancy C; Litovitz; Clancy. Suicidal antidepressant overdoses: a comparative analysis by antidepressant type. Journal of Medical Toxicology. December 2008, 4 (4): 238–250. PMC 3550116
 . PMID 19031375. doi:10.1007/BF03161207/pdf/13181_2009_Article_BF03161207.pdf (不活躍 2015-05-19).
. PMID 19031375. doi:10.1007/BF03161207/pdf/13181_2009_Article_BF03161207.pdf (不活躍 2015-05-19).
- ^ 存档副本 (PDF). [2015-09-03]. (原始內容 (PDF)存檔於2020-09-20).
- ^ Meyer JH, Wilson AA, Sagrati S, Hussey D, Carella A, Potter WZ, Ginovart N, Spencer EP, Cheok A, Houle S; Wilson; Sagrati; Hussey; Carella; Potter; Ginovart; Spencer; Cheok; Houle. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. The American Journal of Psychiatry. 2004, 161 (5): 826–35. PMID 15121647. doi:10.1176/appi.ajp.161.5.826.
- ^ DeVane CL, Liston HL, Markowitz JS; Liston; Markowitz. Clinical pharmacokinetics of sertraline. Clinical Pharmacokinetics. 2002, 41 (15): 1247–66. PMID 12452737. doi:10.2165/00003088-200241150-00002.
- ^ Kobayashi K, Ishizuka T, Shimada N, Yoshimura Y, Kamijima K, Chiba K; Ishizuka; Shimada; Yoshimura; Kamijima; Chiba. Sertraline N-demethylation is catalyzed by multiple isoforms of human cytochrome P-450 in vitro. Drug Metab. Dispos. 1999, 27 (7): 763–6. PMID 10383917.
- ^ Hamelin BA, Turgeon J, Vallée F, Bélanger PM, Paquet F, LeBel M; Turgeon; Vallée; Bélanger; Paquet; Lebel. The disposition of fluoxetine but not sertraline is altered in poor metabolizers of debrisoquin. Clin. Pharmacol. Ther. 1996, 60 (5): 512–21. PMID 8941024. doi:10.1016/S0009-9236(96)90147-2.
- ^ Wang JH, Liu ZQ, Wang W, Chen XP, Shu Y, He N, Zhou HH; Liu; Wang; Chen; Shu; He; Zhou. Pharmacokinetics of sertraline in relation to genetic polymorphism of CYP2C19. Clin. Pharmacol. Ther. 2001, 70 (1): 42–7. PMID 11452243. doi:10.1067/mcp.2001.116513.
- ^ 引用錯誤:沒有為名為
pmid9400006的參考文獻提供內容 - ^ Madras BK, Fahey MA, Miller GM, De La Garza R, Goulet M, Spealman RD, Meltzer PC, George SR, O'Dowd BF, Bonab AA, Livni E, Fischman AJ; Fahey; Miller; de la Garza; Goulet; Spealman; Meltzer; George; O'Dowd; Bonab; Livni; Fischman. Non-amine-based dopamine transporter (reuptake) inhibitors retain properties of amine-based progenitors. Eur. J. Pharmacol. 2003, 479 (1–3): 41–51. PMID 14612136. doi:10.1016/j.ejphar.2003.08.055.
- ^ Ciraulo, DA; Shader, RI (編). Pharmacotherapy of Depression. SpringerLink 2nd (New York, NY: Humana Press). 2011 [2015-10-04]. ISBN 978-1-60327-434-0. doi:10.1007/978-1-60327-435-7. (原始內容存檔於2021-02-25).
外部連結[編輯]
- List of international brand names for sertraline (頁面存檔備份,存於互聯網檔案館)
- U.S. National Library of Medicine: Drug Information Portal – Sertraline (頁面存檔備份,存於互聯網檔案館)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||
