化学疗法:修订间差异
許多醫學條目需要大幅擴充。建議活化醫學專題小組及開動員令。 =) |
|||
| 第21行: | 第21行: | ||
File:Chemotherapy_with_acral_cooling.jpg|一位女性[[乳癌]]病患正在接受[[歐洲紫杉醇]]化療。手腳各別套上冷手套(手)及{{tsl|en|Wine accessory#Wine coolers|酒類冷卻裝置}}(腳)以減低對[[指甲]]的傷害。 |
File:Chemotherapy_with_acral_cooling.jpg|一位女性[[乳癌]]病患正在接受[[歐洲紫杉醇]]化療。手腳各別套上冷手套(手)及{{tsl|en|Wine accessory#Wine coolers|酒類冷卻裝置}}(腳)以減低對[[指甲]]的傷害。 |
||
</gallery> |
</gallery> |
||
== 治療策略(Treatment strategies) == |
|||
{| border="1" class="wikitable" align="right" |
|||
|+ Common combination [[chemotherapy regimen]]s<ref name=Corrie /> |
|||
! Cancer type |
|||
! Drugs |
|||
! Acronym |
|||
|- |
|||
! rowspan=2 |[[Breast cancer]] |
|||
| [[Cyclophosphamide]], [[methotrexate]], [[5-fluorouracil]] || CMF |
|||
|- |
|||
| [[Doxorubicin]], cyclophosphamide || AC |
|||
|- |
|||
! rowspan=2|[[Hodgkin's disease]] |
|||
| Mustine, [[vincristine]], [[procarbazine]], [[prednisolone]] || MOPP |
|||
|- |
|||
| Doxorubicin, [[bleomycin]], [[vinblastine]], [[dacarbazine]] || ABVD |
|||
|- |
|||
! [[Non-Hodgkin's lymphoma]] |
|||
| Cyclophosphamide, doxorubicin, vincristine, prednisolone || CHOP |
|||
|- |
|||
! [[Germ cell tumor]] |
|||
| Bleomycin, [[etoposide]], [[cisplatin]] || BEP |
|||
|- |
|||
! rowspan=2|[[Stomach cancer]] |
|||
| [[Epirubicin]], cisplatin, 5-fluorouracil || ECF |
|||
|- |
|||
| Epirubicin, cisplatin, [[capecitabine]] || ECX |
|||
|- |
|||
! [[Bladder cancer]] |
|||
| [[Methotrexate]], vincristine, doxorubicin, cisplatin || MVAC |
|||
|- |
|||
! [[Lung cancer]] |
|||
| [[Cyclophosphamide]], [[doxorubicin]], [[vincristine]], || CAV |
|||
|- |
|||
! [[Colorectal cancer]] |
|||
| [[5-fluorouracil]], [[folinic acid]], [[oxaliplatin]] || FOLFOX |
|||
|- |
|||
|} |
|||
There are a number of strategies in the administration of chemotherapeutic drugs used today. Chemotherapy may be given with a [[cure|curative]] intent or it may aim to prolong life or to [[Palliative care|palliate symptoms]]. |
|||
* Induction chemotherapy is the first line treatment of cancer with a chemotherapeutic drug. This type of chemotherapy is used for curative intent.<ref name="isbn0-470-09254-8">Airley, pp. 55-59</ref> |
|||
* Combined modality chemotherapy is the use of drugs with other [[Cancer#Treatments|cancer treatments]], such as [[surgery]], [[radiation therapy]], and/or [[hyperthermia therapy]]. |
|||
* Consolidation chemotherapy is given after remission in order to prolong the overall disease-free time and improve overall survival. The drug that is administered is the same as the drug that achieved remission.<ref name="isbn0-470-09254-8" /> |
|||
* Intensification chemotherapy is identical to consolidation chemotherapy but a different drug than the induction chemotherapy is used.<ref name="isbn0-470-09254-8" /> |
|||
* [[Combination chemotherapy]] involves treating a patient with a number of different drugs simultaneously. The drugs differ in their mechanism and side-effects. The biggest advantage is minimising the chances of resistance developing to any one agent. Also, the drugs can often be used at lower doses, reducing toxicity.<ref name="isbn0-470-09254-8" /><ref name="isbn0-443-07101-2 6">Wood, pp. 17-18</ref> |
|||
* [[Neoadjuvant]] chemotherapy is given prior to a local treatment such as surgery, and is designed to shrink the primary tumor.<ref name="isbn0-470-09254-8" /> It is also given to cancers with a high risk of micrometastatic disease.<ref name="isbn0-7817-7328-8">Perry, p. 42</ref> |
|||
* [[Adjuvant chemotherapy]] is given after a local treatment (radiotherapy or surgery). It can be used when there is little evidence of cancer present, but there is risk of recurrence.<ref name="isbn0-470-09254-8" /> It is also useful in killing any cancerous cells that have spread to other parts of the body. These [[micrometastases]] can be treated with adjuvant chemotherapy and can reduce relapse rates caused by these disseminated cells.<ref name="pmid16061845">{{cite journal | author = Epstein RJ | title = Maintenance therapy to suppress micrometastasis: the new challenge for adjuvant cancer treatment | journal = Clinical Cancer Research | volume = 11 | issue = 15 | pages = 5337–41 | date = Aug 2005 | pmid = 16061845 | doi = 10.1158/1078-0432.CCR-05-0437 }}</ref> |
|||
* Maintenance chemotherapy is a repeated low-dose treatment to prolong remission.<ref name="isbn0-470-09254-8" /> |
|||
* Salvage chemotherapy or palliative chemotherapy is given without curative intent, but simply to decrease tumor load and increase life expectancy. For these regimens, in general, a better toxicity profile is expected.<ref name="isbn0-470-09254-8" /> |
|||
All [[chemotherapy regimen]]s require that the patient be capable of undergoing the treatment. [[Performance status]] is often used as a measure to determine whether a patient can receive chemotherapy, or whether dose reduction is required. Because only a fraction of the cells in a tumor die with each treatment ([[fractional kill]]), repeated doses must be administered to continue to reduce the size of the tumor.<ref name=skeel>{{cite book | name-list-format = vanc |last1=Skeel |first1= R. T. |year=2003 |title= Handbook of Cancer Chemotherapy (paperback) |publisher=Lippincott Williams & Wilkins |edition=6th |isbn=0-7817-3629-3}}</ref> Current chemotherapy regimens apply drug treatment in cycles, with the frequency and duration of treatments limited by toxicity to the patient.<ref name=chabner>{{cite book | name-list-format = vanc |last1=Chabner|first1= B. |last2= Longo | first2=D. L. |year=2005 | edition=4th |title= Cancer Chemotherapy and Biotherapy: Principles and Practice|location= Philadelphia |publisher= Lippincott Willians & Wilkins |isbn= 0-7817-5628-6}}</ref> |
|||
=== 治療效果(Efficacy) === |
|||
The efficacy of chemotherapy depends on the type of cancer and the stage. The overall effectiveness ranges from being curative for some cancers, such as some [[leukemias]],<ref>{{cite journal |vauthors=Nastoupil LJ, Rose AC, Flowers CR | title = Diffuse large B-cell lymphoma: current treatment approaches | journal = Oncology | volume = 26 | issue = 5 | pages = 488–95 | date = May 2012 | pmid = 22730604 }}</ref><ref>{{cite journal | author = Freedman A | title = Follicular lymphoma: 2012 update on diagnosis and management | journal = American Journal of Hematology | volume = 87 | issue = 10 | pages = 988–95 | date = Oct 2012 | pmid = 23001911 | doi = 10.1002/ajh.23313 }}</ref> to being ineffective, such as in some [[brain tumors]],<ref>{{cite journal |vauthors=Rampling R, James A, Papanastassiou V | title = The present and future management of malignant brain tumours: surgery, radiotherapy, chemotherapy | journal = Journal of Neurology, Neurosurgery, and Psychiatry | volume = 75 Suppl 2 | issue = Suppl 2 | pages = ii24–30 | date = Jun 2004 | pmid = 15146036 | pmc = 1765659 | doi = 10.1136/jnnp.2004.040535 }}</ref> to being needless in others, like most [[non-melanoma skin cancer]]s.<ref>{{cite journal |vauthors=Madan V, Lear JT, Szeimies RM | title = Non-melanoma skin cancer | journal = Lancet | volume = 375 | issue = 9715 | pages = 673–85 | date = Feb 2010 | pmid = 20171403 | doi = 10.1016/S0140-6736(09)61196-X }}</ref> |
|||
=== 劑量(Dosage) === |
|||
[[File:Screenshot at 2013-08-16 14 52 30.png|thumb|left|Dose response relationship of cell killing by chemotherapeutic drugs on normal and cancer cells. At high doses the percentage of normal and cancer cells killed is very similar. For this reason, doses are chosen where anti-tumour activity exceeds normal cell death.<ref name=Corrie />]] |
|||
Dosage of chemotherapy can be difficult: If the dose is too low, it will be ineffective against the tumor, whereas, at excessive doses, the toxicity ([[adverse effect|side-effects]]) will be intolerable to the patient.<ref name=Corrie /> The standard method of determining chemotherapy dosage is based on calculated [[body surface area]] (BSA). The BSA is usually calculated with a mathematical formula or a [[nomogram]], using a patient's weight and height, rather than by direct measurement of body mass. This formula was originally derived in a 1916 study and attempted to translate medicinal doses established with laboratory animals to equivalent doses for humans.<ref>{{cite journal|author1=Du Bois D|author2=Du Bois EF|title=A formula to estimate the approximate surface area if height and weight be known. 1916.|journal=Archives Internal Medicine|volume=5|issue=5|pages=303–11}}</ref> The study only included 9 human subjects.<ref name="dosing strategies">{{cite journal|author1=Felici A.|author2=J. Verweij|author3=A. Sparreboom|title=Dosing strategies for anticancer drugs: the good, the bad and body-surface area|journal=Eur J Cancer|year=2002|volume=38|issue=13|pages=1677–84|doi=10.1016/s0959-8049(02)00151-x}}</ref> When chemotherapy was introduced in the 1950s, the BSA formula was adopted as the official standard for chemotherapy dosing for lack of a better option.<ref name="pmid17305252">{{cite journal |vauthors=Kaestner SA, Sewell GJ | title = Chemotherapy dosing part I: scientific basis for current practice and use of body surface area | journal = Clinical Oncology | volume = 19 | issue = 1 | pages = 23–37 | date = Feb 2007 | pmid = 17305252 | doi = 10.1016/j.clon.2006.10.010 }}</ref><ref>{{cite journal|title=The Use of Body Surface Area as a Criterion of Drug Dosage in Cancer Chemotherapy|author=Donald Pinkel|journal=Cancer Res|date=August 1958|volume=18|issue=7|pages=853–6}}</ref> |
|||
Recently, the validity of this method in calculating uniform doses has been questioned. The reason for this is that the formula only takes into account the individual's weight and height. Drug absorption and clearance are influenced by multiple factors, including age, gender, metabolism, disease state, organ function, drug-to-drug interactions, genetics, and obesity, which has a major impact on the actual concentration of the drug in the patient's bloodstream.<ref name="pmid17305252" /><ref name="pmid11953888">{{cite journal | author = Gurney H | title = How to calculate the dose of chemotherapy | journal = British Journal of Cancer | volume = 86 | issue = 8 | pages = 1297–302 | date = Apr 2002 | pmid = 11953888 | pmc = 2375356 | doi = 10.1038/sj.bjc.6600139 }}</ref><ref name="pmid22965963">{{cite journal |vauthors=Beumer JH, Chu E, Salamone SJ | title = Body-surface area-based chemotherapy dosing: appropriate in the 21st century? | journal = Journal of Clinical Oncology | volume = 30 | issue = 31 | pages = 3896–7 | date = Nov 2012 | pmid = 22965963 | doi = 10.1200/JCO.2012.44.2863 }}</ref> As a result, there is high variability in the systemic chemotherapy drug concentration among patients dosed by BSA, and this variability has been demonstrated to be more than 10-fold for many drugs.<ref name="dosing strategies" /><ref name="role of body">{{cite journal|author1=Baker SD|author2=Verweij J|author3=Rowinsky EK|author4=Donehower RC|author5=Schellens JH|author6=Grochow LB|author7=Sparreboom A|title=Role of body surface area in dosing of investigational anticancer agents in adults, 1991–2001|journal=J Natl Cancer Inst|year=2002|volume=94|issue=24|pages=1883–8|doi=10.1093/jnci/94.24.1883}}</ref> In other words, if two patients receive the same dose of a given drug based on BSA, the concentration of that drug in the bloodstream of one patient may be 10 times higher or lower compared to that of the other patient.<ref name="role of body" /> This variability is typical with many chemotherapy drugs dosed by BSA, and, as shown below, was demonstrated in a study of 14 common chemotherapy drugs.<ref name="dosing strategies" /> |
|||
[[File:Improvement in Response Rate.jpg|thumb|180px|right|5-FU dose management results in significantly better response and survival rates versus BSA dosing.<ref name="individual fluorouracil" />]] |
|||
The result of this pharmacokinetic variability among patients is that many patients do not receive the right dose to achieve optimal treatment effectiveness with minimized toxic side effects. Some patients are overdosed while others are underdosed.<ref name="pmid17305252" /><ref name="pmid11953888" /><ref name="pmid22965963" /><ref name="individual fluorouracil">{{cite journal|author1=Gamelin EC|author2=Delva R|author3=Jacob J|author4=Merrouche Y|author5=Raoul JL|author6=Pezet D|author7=Dorval E|author8=Piot G|author9=Morel A|author10=Boisdron-Celle M|title= Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: Results of a multicenter randomized trial of patients with metastatic colorectal cancer|journal=J Clin Oncol|year=2008|volume=26|issue=13|pages=2099–2105|doi=10.1200/jco.2007.13.3934|pmid=18445839}}</ref><ref>{{cite journal|author1=Saam J|author2=Critchfield GC|author3=Hamilton SA|author4=Roa BB|author5=Wenstrup RJ|author6=Kaldate RR|title=Body Surface Area-based Dosing of 5-Fluorouracil Results in Extensive Interindividual Variability in 5-Fluorouracil Exposure in Colorectal Cancer Patients on FOLFOX Regimens|journal=Clin Colorectal Cancer|year=2011|volume=10|issue=3|pages=203–206|doi=10.1016/j.clcc.2011.03.015}}</ref><ref name="dose adjustment">{{cite journal|author1=Capitain O|author2=Asevoaia A|author3=Boisdron-Celle M|author4=Poirier AL|author5=Morel A|author6=Gamelin E|title=Individual Fluorouracil Dose Adjustment in FOLFOX Based on Pharmacokinetic Follow-Up Compared With Conventional Body-Area-Surface Dosing: A Phase II, Proof-of-Concept Study|journal=Clin Colorectal Cancer|year=2012|volume=11|issue=4|pages=263–267|doi=10.1016/j.clcc.2012.05.004}}</ref><ref>{{cite journal|author1=Kaldate RR|author2=Haregewoin A|author3=Grier CE|author4=Hamilton SA|author5=McLeod HL|title=Modeling the 5-fluorouracil area under the curve versus dose relationship to develop a pharmacokinetic dosing algorithm for colorectal cancer patients receiving FOLFOX6|journal=Oncologist |volume=17|issue=3|pages=296–302|doi=10.1634/theoncologist.2011-0357}}</ref> For example, in a randomized clinical trial, investigators found 85% of metastatic colorectal cancer patients treated with 5-fluorouracil (5-FU) did not receive the optimal therapeutic dose when dosed by the BSA standard—68% were underdosed and 17% were overdosed.<ref name="individual fluorouracil" /> |
|||
There has been recent controversy over the use of BSA to calculate chemotherapy doses for [[obese]] patients.<ref name="dosing chemotherapy">{{cite journal |vauthors=Hunter RJ, Navo MA, Thaker PH, Bodurka DC, Wolf JK, Smith JA | title = Dosing chemotherapy in obese patients: actual versus assigned body surface area (BSA) | journal = Cancer Treat Rev| volume = 35 | issue = 1 | pages = 69–78 | date = Feb 2009 | pmid = 18922643 | doi = 10.1016/j.ctrv.2008.07.005 }}</ref> Because of their higher BSA, clinicians often arbitrarily reduce the dose prescribed by the BSA formula for fear of [[overdosing]].<ref name="dosing chemotherapy" /> In many cases, this can result in sub-optimal treatment.<ref name="dosing chemotherapy" /> |
|||
Several clinical studies have demonstrated that when chemotherapy dosing is individualized to achieve optimal systemic drug exposure, treatment outcomes are improved and toxic side effects are reduced.<ref name="individual fluorouracil" /><ref name="dose adjustment" /> In the 5-FU clinical study cited above, patients whose dose was adjusted to achieve a pre-determined target exposure realized an 84% improvement in treatment response rate and a six-month improvement in overall survival (OS) compared with those dosed by BSA.<ref name="individual fluorouracil" /> |
|||
[[File:Toxicity.png|thumb|180px|left|5-FU dose management avoids serious side effects experienced with BSA dosing<ref name="individual fluorouracil" />]] |
|||
{{multiple image |
|||
| align = right |
|||
| direction = vertical |
|||
| width = 100 |
|||
| image1 = Response 1.jpg |
|||
| image2 = Survival 1.png |
|||
| caption2 = 5-FU dose management in the FOLFOX regimen increases treatment response significantly & improves survival by 6 months<ref name="dose adjustment" /> |
|||
}} |
|||
In the same study, investigators compared the incidence of common 5-FU-associated grade 3/4 toxicities between the dose-adjusted patients and the BSA-dosed patients.<ref name="individual fluorouracil" /> The incidence of debilitating grades of diarrhea was reduced from 18% in the BSA-dosed group to 4% in the dose-adjusted group of patients and serious hematologic side effects were eliminated.<ref name="individual fluorouracil" /> Because of the reduced toxicity, dose-adjusted patients were able to be treated for longer periods of time.<ref name="individual fluorouracil" /> BSA-dosed patients were treated for a total of 680 months while dose-adjusted patients were treated for a total of 791 months.<ref name="individual fluorouracil" /> Completing the course of treatment is an important factor in achieving better treatment outcomes. |
|||
Similar results were found in a study involving colorectal cancer patients treated with the popular [[FOLFOX]] regimen.<ref name="dose adjustment" /> The incidence of serious diarrhea was reduced from 12% in the BSA-dosed group of patients to 1.7% in the dose-adjusted group, and the incidence of severe mucositis was reduced from 15% to 0.8%.<ref name="dose adjustment" /> |
|||
The FOLFOX study also demonstrated an improvement in treatment outcomes.<ref name="dose adjustment" /> Positive response increased from 46% in the BSA-dosed patients to 70% in the dose-adjusted group. Median progression free survival (PFS) and overall survival (OS) both improved by six months in the dose adjusted group.<ref name="dose adjustment" /> |
|||
One approach that can help clinicians individualize chemotherapy dosing is to measure the drug levels in blood plasma over time and adjust dose according to a formula or algorithm to achieve optimal exposure. With an established target exposure for optimized treatment effectiveness with minimized toxicities, dosing can be personalized to achieve target exposure and optimal results for each patient. Such an algorithm was used in the clinical trials cited above and resulted in significantly improved treatment outcomes. |
|||
Oncologists are already individualizing dosing of some cancer drugs based on exposure. [[Carboplatin]]<ref name="isbn0-521-61816-9">Macbeth, p. 4</ref> and [[busulfan]]<ref>{{cite journal|author1=Buffery, PJ|author2=Allen, KM|author3=Chin, PKL|author4=Moore, GA|author5=Barclay, ML|author6=Begg, EJ|title=Thirteen Years' Experience of Pharmacokinetic Monitoring and Dosing of Busulfan: Can the Strategy Be Improved?|journal=Ther Drug Monit|year=2014|volume=36|issue=1|pages=86–92}}</ref><ref>{{cite journal|author1=Bartelink IH|author2=Bredius RG|author3=Belitser SV|author4=Suttorp MM|author5=Bierings M|author6=Knibbe CA|author7=Egeler M|author8=Lankester AC|author9=Egberts AC|author10=Zwaveling J|author11=Boelens JJ|title=Association Between Busulfan Exposure and Outcome in Children Receiving Intravenous Busulfan Before Hematopoietic Stem Cell Transplantation|journal=Ther Drug Monit|volume=36|issue=1|pages=93–99}}</ref> dosing rely upon results from blood tests to calculate the optimal dose for each patient. Simple blood tests are also available for dose optimization of [[methotrexate]],<ref>{{cite web|url=http://ark-tdm.com/DB_methotrexate.html|title=ARK™ Methotrexate Assay|publisher=Ark Diagnostics}}</ref> 5-FU, [[paclitaxel]], and [[docetaxel]].<ref>{{cite web|url=http://mycaretests.com|title=Customizing Chemotherapy for Better Cancer Care|publisher=My Care Diagnostics}}</ref><ref>{{cite web|url=http://bettercancercare.com|title=A Brief History of BSA Dosing|publisher=My Care Diagnostics}}</ref> |
|||
=== 種類(Types) === |
|||
[[File:Cross-linked DNA by nitrogen mustard.png|thumb|left| Two DNA bases that are cross-linked by a nitrogen mustard. Different nitrogen mustards will have different chemical groups (R). The nitrogen mustards most commonly alkylate the N7 nitrogen of guanine (as shown here) but other atoms can be alkylated.<ref name =Siddik />]] |
|||
==== 烷基化劑(Alkylating agents) ==== |
|||
{{Main|Alkylating antineoplastic agent}} |
|||
Alkylating agents are the oldest group of chemotherapeutics in use today. Originally derived from [[mustard gas]] used in [[World War I]], there are now many types of alkylating agents in use.<ref name=Corrie /> They are so named because of their ability to [[alkylation|alkylate]] many molecules, including [[protein]]s, [[RNA]] and [[DNA]]. This ability to bind [[covalent bond|covalently]] to DNA via their [[alkyl group]] is the primary cause for their anti-cancer effects.<ref name=lind>{{cite journal|last=Lind M.J.|title=Principles of cytotoxic chemotherapy|journal=Medicine|year=2008|volume=36|issue=1|pages=19–23|doi=10.1016/j.mpmed.2007.10.003|first1=M.J.}}</ref> DNA is made of two strands and the molecules may either bind twice to one strand of DNA (intrastrand crosslink) or may bind once to both strands (interstrand crosslink). If the cell tries to replicate crosslinked DNA during [[cell division]], or tries to repair it, the DNA strands can break. This leads to a form of programmed cell death called [[apoptosis]].<ref name =Siddik>{{cite book | name-list-format = vanc |last=Siddik ZH|title=Mechanisms of Action of Cancer Chemotherapeutic Agents: DNA-Interactive Alkylating Agents and Antitumour Platinum-Based Drugs|year=2005|publisher=John Wiley & Sons, Ltd|doi=10.1002/0470025077.chap84b}}</ref><ref name="pmid19002790" /> Alkylating agents will work at any point in the cell cycle and thus are known as cell cycle-independent drugs. For this reason the effect on the cell is dose dependent; the fraction of cells that die is directly proportional to the dose of drug.<ref name="pmid14508075" /> |
|||
The subtypes of alkylating agents are the [[nitrogen mustard]]s, [[nitrosoureas]], [[tetrazine]]s, [[aziridine]]s,<ref>{{cite journal |author1=Giorgi-Renault S. |author2=Renault J. |author3=Baron M. |author4=Gebel-Servolles P. |author5=Delic J. |author6=Cros S. |author7=Paoletti C. | year = 1988 | title = Heterocyclic quinones XIII. Dimerization in the series of 5,8-quinazolinediones: Synthesis and anti tumor effects of bis(4-amino-5,8-quinazolinediones) | url = | journal = Chem. Pharm. Bull. | volume = 36 | issue = 10| pages = 3933–3947 | doi=10.1248/cpb.36.3933}}</ref> [[cisplatin]]s and derivatives, and non-classical alkylating agents. Nitrogen mustards include [[mechlorethamine]], [[cyclophosphamide]], [[melphalan]], [[chlorambucil]], [[ifosfamide]] and [[busulfan]]. Nitrosoureas include [[N-Nitroso-N-methylurea]] (MNU), [[carmustine]] (BCNU), [[lomustine]] (CCNU) and [[semustine]] (MeCCNU), [[fotemustine]] and [[streptozotocin]]. Tetrazines include [[dacarbazine]], [[mitozolomide]] and [[temozolomide]]. Aziridines include [[thiotepa]], [[mytomycin]] and diaziquone (AZQ). Cisplatin and derivatives include [[cisplatin]], [[carboplatin]] and [[oxaliplatin]].<ref name=lind /><ref name="pmid19002790">{{cite journal |vauthors=Damia G, D'Incalci M | title = Mechanisms of resistance to alkylating agents | journal = Cytotechnology | volume = 27 | issue = 1–3 | pages = 165–73 | date = Sep 1998 | pmid = 19002790 | pmc = 3449574 | doi = 10.1023/A:1008060720608 }}</ref> They impair cell function by forming [[covalent bond]]s with the [[amino group|amino]], [[carboxyl group|carboxyl]], [[sulfhydryl group|sulfhydryl]], and [[phosphate group]]s in biologically important molecules.<ref name=takimoto>Takimoto CH, Calvo E.[http://www.cancernetwork.com/cancer-management-11/chapter03/article/10165/1402628 "Principles of Oncologic Pharmacotherapy"] in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) [http://www.cancernetwork.com/cancer-management-11/ Cancer Management: A Multidisciplinary Approach]. 11 ed. 2008.</ref> Non-classical alkylating agents include [[procarbazine]] and hexamethylmelamine.<ref name=lind /><ref name="pmid19002790" /> |
|||
==== Antimetabolites ==== |
|||
[[File:Deoxcytidine, Gemcitidine and Decitabine.png|thumb|[[Deoxycytidine]] (left) and two anti-metabolite drugs (center and right); [[gemcitabine]] and [[decitabine]]. The drugs are very similar but they have subtle differences in their [[chemical structure]].]] |
|||
{{Main|Antimetabolite}} |
|||
[[Anti-metabolite]]s are a group of molecules that impede DNA and RNA synthesis. Many of them have a similar structure to the building blocks of DNA and RNA. The building blocks are [[nucleotide]]s; a molecule comprising a [[nucleobase]], a sugar and a [[phosphate group]]. The nucleobases are divided into [[purine]]s ([[guanine]] and [[adenine]]) and [[pyrimidine]]s ([[cytosine]], [[thymine]] and [[uracil]]). Anti-metabolites resemble either nucleobases or nucleosides (a nucleotide without the phosphate group), but have altered [[chemical group]]s.<ref name="pmid19476376">{{cite journal | author = Parker WB | title = Enzymology of purine and pyrimidine antimetabolites used in the treatment of cancer | journal = Chemical Reviews | volume = 109 | issue = 7 | pages = 2880–93 | date = Jul 2009 | pmid = 19476376 | pmc = 2827868 | doi = 10.1021/cr900028p }}</ref> These drugs exert their effect by either blocking the enzymes required for DNA synthesis or becoming incorporated into DNA or RNA. By inhibiting the enzymes involved in DNA synthesis, they prevent mitosis because the DNA cannot duplicate itself. Also, after misincorporation of the molecules into DNA, [[DNA damage]] can occur and programmed cell death ([[apoptosis]]) is induced. Unlike alkylating agents, anti-metabolites are cell cycle dependent. This means that they only work during a specific part of the cell cycle, in this case [[S-phase]] (the DNA synthesis phase). For this reason, at a certain dose, the effect plateaus and proportionally no more cell death occurs with increased doses. Subtypes of the anti-metabolites are the [[antifolate|anti-folates]], fluoropyrimidines, deoxynucleoside analogues and [[thiopurine]]s.<ref name=lind /><ref name="pmid19476376" /> |
|||
The anti-folates include [[methotrexate]] and [[pemetrexed]]. Methotrexate inhibits [[dihydrofolate reductase]] (DHFR), an enzyme that regenerates [[tetrahydrofolate]] from [[dihydrofolate]]. When the enzyme is inhibited by methotrexate, the cellular levels of folate coenzymes diminish. These are required for [[thymidylate]] and purine production, which are both essential for DNA synthesis and cell division.<ref name="isbn0-470-09254-8" /><ref name="isbn0-443-07101-2">Wood, p. 11</ref> Pemetrexed is another anti-metabolite that affects purine and pyrimidine production, and therefore also inhibits DNA synthesis. It primarily inhibits the enzyme [[thymidylate synthase]], but also has effects on DHFR, aminoimidazole carboxamide ribonucleotide formyltransferase and [[glycinamide ribonucleotide formyltransferase]].<ref name="pmid15217974">{{cite journal | author = Adjei AA | title = Pemetrexed (ALIMTA), a novel multitargeted antineoplastic agent | journal = Clinical Cancer Research | volume = 10 | issue = 12 Pt 2 | pages = 4276s–4280s | date = Jun 2004 | pmid = 15217974 | doi = 10.1158/1078-0432.CCR-040010 }}</ref> The fluoropyrimidines include [[fluorouracil]] and [[capecitabine]]. Fluorouracil is a nucleobase analogue that is metabolised in cells to form at least two active products; 5-fluourouridine monophosphate (FUMP) and 5-fluoro-2'-deoxyuridine 5'-phosphate (fdUMP). FUMP becomes incorporated into RNA and fdUMP inhibits the enzyme thymidylate synthase; both of which lead to cell death.<ref name="isbn0-443-07101-2" /> Capecitabine is a [[prodrug]] of 5-fluorouracil that is broken down in cells to produce the active drug.<ref name="pmid12515569">{{cite journal |vauthors=Wagstaff AJ, Ibbotson T, Goa KL | title = Capecitabine: a review of its pharmacology and therapeutic efficacy in the management of advanced breast cancer | journal = Drugs | volume = 63 | issue = 2 | pages = 217–36 | year = 2003 | pmid = 12515569 | doi = 10.2165/00003495-200363020-00009 }}</ref> The deoxynucleoside analogues include [[cytarabine]], [[gemcitabine]], [[decitabine]], [[azacitidine]], [[fludarabine]], [[nelarabine]], [[cladribine]], [[clofarabine]], and [[pentostatin]]. The thiopurines include [[thioguanine]] and [[mercaptopurine]].<ref name=lind /><ref name="pmid19476376" /> |
|||
==== Anti-microtubule agents ==== |
|||
[[File:Microtubules and alkaloids.png|thumb|left|Vinca alkaloids prevent the assembly of microtubules, whereas taxanes prevent their disassembly. Both mechanisms cause defective mitosis.]] |
|||
[[Anti-microtubule agent]]s are [[plant]]-derived chemicals that block cell division by preventing [[microtubule]] function. Microtubules are an important cellular structure composed of two proteins; [[α-tubulin]] and [[β-tubulin]]. They are hollow rod shaped structures that are required for cell division, among other cellular functions.<ref name="pmid1687171">{{cite journal |vauthors=Rowinsky EK, Donehower RC | title = The clinical pharmacology and use of antimicrotubule agents in cancer chemotherapeutics | journal = Pharmacology & Therapeutics | volume = 52 | issue = 1 | pages = 35–84 | date = Oct 1991 | pmid = 1687171 | doi = 10.1016/0163-7258(91)90086-2 }}</ref> Microtubules are dynamic structures, which means that they are permanently in a state of assembly and disassembly. [[Vinca alkaloid]]s and [[taxane]]s are the two main groups of anti-microtubule agents, and although both of these groups of drugs cause microtubule dysfunction, their mechanisms of action are completely opposite. The vinca alkaloids prevent the formation of the microtubules, whereas the taxanes prevent the microtubule disassembly. By doing so, they prevent the cancer cells from completing mitosis. Following this, cell cycle arrest occurs, which induces programmed cell death ([[apoptosis]]).<ref name=lind /><ref name="pmid20577942" /> Also, these drugs can affect [[Angiogenesis|blood vessel growth]]; an essential process that tumours utilise in order to grow and metastasise.<ref name="pmid20577942">{{cite journal |vauthors=Yue QX, Liu X, Guo DA | title = Microtubule-binding natural products for cancer therapy | journal = Planta Medica | volume = 76 | issue = 11 | pages = 1037–43 | date = Aug 2010 | pmid = 20577942 | doi = 10.1055/s-0030-1250073 }}</ref> |
|||
Vinca alkaloids are derived from the [[Madagascar periwinkle]], ''Catharanthus roseus'' (formerly known as ''Vinca rosea''). They bind to specific sites on tubulin, inhibiting the assembly of tubulin into microtubules. The original vinca alkaloids are completely natural chemicals that include [[vincristine]] and [[vinblastine]]. Following the success of these drugs, semi-synthetic vinca alkaloids were produced: [[vinorelbine]], [[vindesine]], and [[vinflunine]].<ref name="pmid20577942" /> These drugs are [[cell cycle]]-specific. They bind to the tubulin molecules in [[S-phase]] and prevent proper microtubule formation required for [[M-phase]].<ref name="pmid14508075" /> |
|||
Taxanes are natural and semi-synthetic drugs. The first drug of their class, [[paclitaxel]], was originally extracted from the [[Pacific Yew]] tree, ''Taxus brevifolia''. Now this drug and another in this class, [[docetaxel]], are produced semi-synthetically from a chemical found in the bark of another Yew tree; ''[[Taxus baccata]]''. These drugs promote microtubule stability, preventing their disassembly. Paclitaxel prevents the cell cycle at the boundary of G2-M, whereas docetaxel exerts its effect during [[S-phase]]. Taxanes present difficulties in formulation as medicines because they are poorly soluble in water.<ref name="pmid20577942" /> |
|||
[[Podophyllotoxin]] is an antineoplastic [[lignan]] obtained primarily from the [[American Mayapple]] (''Podophyllum peltatum'') and [[Himalayan Mayapple]] (''Podophyllum hexandrum'' or ''Podophyllum emodi''). It has anti-microtubule activity, and its mechanism is similar to that of vinca alkaloids in that they bind to tubulin, inhibiting microtubule formation. Podophyllotoxin is used to produce two other drugs with different mechanisms of action: [[etoposide]] and [[teniposide]].<ref name="pmid9562603">{{cite journal |vauthors=Damayanthi Y, Lown JW | title = Podophyllotoxins: current status and recent developments | journal = Current Medicinal Chemistry | volume = 5 | issue = 3 | pages = 205–52 | date = Jun 1998 | pmid = 9562603 }}</ref><ref>{{cite journal|last=Liu YQ, Yang L, Tian X|title=Podophyllotoxin: current perspectives|journal=Curr Bioactive Compounds|year=2007|volume=3|issue=1|pages=37–66|doi=10.1016/j.jallcom.2006.06.070|first1=Cong|last2=Zhang|first2=Wei|last3=Qian|first3=Zhengnan|last4=Hua|first4=Zhong|last5=Zhao|first5=Qibo|last6=Sui|first6=Yu|last7=Su|first7=Wenhui|last8=Zhang|first8=Ming|last9=Liu|first9=Zhuhong|last10=Liu|first10=Guodong|last11=Wu|first11=Guangheng}}</ref> |
|||
==== Topoisomerase inhibitors ==== |
|||
[[File:Topoisomerase Inhibitor.JPG|thumb|Topoisomerase I and II Inhibitors]] |
|||
[[Topoisomerase inhibitor]]s are drugs that affect the activity of two enzymes: [[topoisomerase I]] and [[topoisomerase II]]. When the DNA double-strand helix is unwound, during DNA replication or [[transcription (biology)|transcription]], for example, the adjacent unopened DNA winds tighter (supercoils), like opening the middle of a twisted rope. The stress caused by this effect is in part aided by the topoisomerase enzymes. They produce single- or double-strand breaks into DNA, reducing the tension in the DNA strand. This allows the normal unwinding of DNA to occur during [[DNA replication|replication]] or [[transcription (biology)|transcription]]. Inhibition of topoisomerase I or II interferes with both of these processes.<ref>{{cite book | name-list-format = vanc |vauthors=Lodish H, Berk A, Zipursky SL |title=Molecular Cell Biology. 4th edition. The Role of Topoisomerases in DNA Replication|year=2000|publisher=New York: W. H. Freeman|url=http://www.ncbi.nlm.nih.gov/books/NBK21703/|displayauthors=etal }}</ref><ref name="pmid12351817">{{cite journal | author = Goodsell DS | title = The molecular perspective: DNA topoisomerases | journal = Stem Cells | volume = 20 | issue = 5 | pages = 470–1 | year = 2002 | pmid = 12351817 | doi = 10.1634/stemcells.20-5-470 }}</ref> |
|||
Two topoisomerase I inhibitors, [[irinotecan]] and [[topotecan]], are semi-synthetically derived from [[camptothecin]], which is obtained from the Chinese ornamental tree ''[[Camptotheca acuminata]]''.<ref name="pmid14508075" /> Drugs that target topoisomerase II can be divided into two groups. The topoisomerase II poisons cause increased levels enzymes bound to DNA. This prevents DNA replication and [[transcription (biology)|transcription]], causes DNA strand breaks, and leads to programmed cell death ([[apoptosis]]). These agents include [[etoposide]], [[doxorubicin]], [[mitoxantrone]] and [[teniposide]]. The second group, catalytic inhibitors, are drugs that block the activity of topoisomerase II, and therefore prevent DNA synthesis and translation because the DNA cannot unwind properly. This group includes [[novobiocin]], merbarone, and [[aclarubicin]], which also have other significant mechanisms of action.<ref name="pmid19377506">{{cite journal | author = Nitiss JL | title = Targeting DNA topoisomerase II in cancer chemotherapy | journal = Nature Reviews. Cancer | volume = 9 | issue = 5 | pages = 338–50 | date = May 2009 | pmid = 19377506 | pmc = 2748742 | doi = 10.1038/nrc2607 }}</ref> |
|||
==== Cytotoxic antibiotics ==== |
|||
The cytotoxic [[antibiotics]] are a varied group of drugs that have various mechanisms of action. The common theme that they share in their chemotherapy indication is that they interrupt [[cell division]]. The most important subgroup is the [[anthracycline]]s and the [[bleomycin]]s; other prominent examples include [[mitomycin C]], [[mitoxantrone]], and [[actinomycin]].<ref>Antineoplastic Agents in Encyclopedia of Molecular Pharmacology, 2nd Edition, Volume 1. Eds. Offermanns S and Rosenthal W. Springer, 2008. {{ISBN|9783540389163}} [https://books.google.com/books?id=iwwo5gx8aX8C&pg=PA155 P 155]</ref> |
|||
Among the anthracyclines, [[doxorubicin]] and [[daunorubicin]] were the first, and were obtained from the [[bacterium]] ''[[Streptomyces peucetius]]''.<ref>MInotti G et al. Anthracyclines in Encyclopedia of Molecular Pharmacology, 2nd Edition, Volume 1. Eds. Offermanns S and Rosenthal W. Springer, 2008. {{ISBN|9783540389163}} [https://books.google.com/books?id=iwwo5gx8aX8C&pg=PA91 P 91ff]</ref> Derivatives of these compounds include [[epirubicin]] and [[idarubicin]]. Other clinically used drugs in the anthracyline group are [[pirarubicin]], [[aclarubicin]], and [[mitoxantrone]]. The mechanisms of anthracyclines include [[DNA intercalation]] (molecules insert between the two strands of DNA), generation of highly reactive [[free radicals]] that damage intercellular molecules and topoisomerase inhibition.<ref name="pmid15169927">{{cite journal |vauthors=Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L | title = Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity | journal = Pharmacological Reviews | volume = 56 | issue = 2 | pages = 185–229 | date = Jun 2004 | pmid = 15169927 | doi = 10.1124/pr.56.2.6 }}</ref> |
|||
Actinomycin is a complex molecule that intercalates DNA and prevents [[RNA synthesis]].<ref name="pmid2410919">{{cite journal | author = Sobell HM | title = Actinomycin and DNA transcription | journal = Proceedings of the National Academy of Sciences of the United States of America | volume = 82 | issue = 16 | pages = 5328–31 | date = Aug 1985 | pmid = 2410919 | pmc = 390561 | doi = 10.1073/pnas.82.16.5328 | bibcode = 1985PNAS...82.5328S }}</ref> |
|||
Bleomycin, a [[glycopeptide]] isolated from ''Streptomyces verticillus'', also intercalates DNA, but produces [[free radical]]s that damage DNA. This occurs when bleomycin binds to a [[metal ion]], becomes [[reduction (chemistry)|chemically reduced]] and reacts with [[oxygen]].<ref name="pmid1384141">{{cite journal | author = Dorr RT | title = Bleomycin pharmacology: mechanism of action and resistance, and clinical pharmacokinetics | journal = Seminars in Oncology | volume = 19 | issue = 2 Suppl 5 | pages = 3–8 | date = Apr 1992 | pmid = 1384141 | doi = }}</ref><ref name="isbn0-470-09254-8 3">Airley, p. 87</ref> |
|||
Mitomycin is a cytotoxic antibiotic with the ability to alkylate DNA.<ref name="pmid2131038">{{cite journal |vauthors=Verweij J, Pinedo HM | title = Mitomycin C: mechanism of action, usefulness and limitations | journal = Anti-Cancer Drugs | volume = 1 | issue = 1 | pages = 5–13 | date = Oct 1990 | pmid = 2131038 | doi = 10.1097/00001813-199010000-00002 }}</ref> |
|||
=== Delivery === |
|||
[[File:Cyclophosphamide iv.jpg|thumb|140px|[[Cyclophosphamide]] IV drip]] |
|||
Most chemotherapy is [[Route of administration|delivered]] [[intravenous therapy|intravenously]], although a number of agents can be administered orally (e.g., [[melphalan]], [[busulfan]], [[capecitabine]]). |
|||
There are many intravenous methods of drug delivery, known as vascular access devices. These include the [[Winged infusion set|winged infusion device]], [[Intravenous therapy#Peripheral cannula|peripheral cannula]], midline catheter, [[peripherally inserted central catheter]] (PICC), [[central venous catheter]] and [[implantable port]]. The devices have different applications regarding duration of chemotherapy treatment, method of delivery and types of chemotherapeutic agent.<ref name="isbn0-443-07101-2 3">{{cite book | name-list-format = vanc |author1=Wood, Miriam |author2=David Brighton |title=The Royal Marsden Hospital handbook of cancer chemotherapy: a guide for the multidisciplinary team |publisher=Elsevier Churchill Livingstone |location=St. Louis, Mo |year=2005|pages=93–94 |isbn=0-443-07101-2 |oclc= |doi= }}</ref> |
|||
Depending on the patient, the cancer, the stage of cancer, the type of chemotherapy, and the dosage, intravenous chemotherapy may be given on either an [[inpatient]] or an [[outpatient]] basis. For continuous, frequent or prolonged intravenous chemotherapy administration, various systems may be surgically inserted into the vasculature to maintain access.<ref name="isbn0-443-07101-2 5">Wood, pp. 113-118</ref> Commonly used systems are the [[Hickman line]], the [[Port-a-Cath]], and the [[PICC line]]. These have a lower infection risk, are much less prone to [[phlebitis]] or [[extravasation]], and eliminate the need for repeated insertion of peripheral cannulae.{{citation needed|date=August 2013}} |
|||
[[Isolated limb perfusion]] (often used in [[melanoma]]),<ref name="pmid20348274">{{cite journal |vauthors=Moreno-Ramirez D, de la Cruz-Merino L, Ferrandiz L, Villegas-Portero R, Nieto-Garcia A | title = Isolated limb perfusion for malignant melanoma: systematic review on effectiveness and safety | journal = The Oncologist | volume = 15 | issue = 4 | pages = 416–27 | year = 2010 | pmid = 20348274 | pmc = 3227960 | doi = 10.1634/theoncologist.2009-0325 }}</ref> or isolated infusion of chemotherapy into the liver<ref name="pmid18722924">{{cite journal |vauthors=Verhoef C, de Wilt JH, ten Hagen TL, Eggermont AM | title = Isolated hepatic perfusion for the treatment of liver tumors: sunset or sunrise? | journal = Surgical Oncology Clinics of North America | volume = 17 | issue = 4 | pages = 877–94, xi | date = Oct 2008 | pmid = 18722924 | doi = 10.1016/j.soc.2008.04.007 }}</ref> or the lung have been used to treat some tumors. The main purpose of these approaches is to deliver a very high dose of chemotherapy to tumor sites without causing overwhelming systemic damage.<ref name="pmid10421507">{{cite journal |vauthors=Hendriks JM, Van Schil PE | title = Isolated lung perfusion for the treatment of pulmonary metastases | journal = Surgical Oncology | volume = 7 | issue = 1–2 | pages = 59–63 | year = 1998 | pmid = 10421507 | doi = 10.1016/S0960-7404(98)00028-0 }}</ref> These approaches can help control solitary or limited metastases, but they are by definition not systemic, and, therefore, do not treat distributed metastases or [[micrometastasis|micrometastases]]. |
|||
Topical chemotherapies, such as [[5-fluorouracil]], are used to treat some cases of [[non-melanoma skin cancer]].<ref>{{cite journal |vauthors=Chitwood K, Etzkorn J, Cohen G | title = Topical and intralesional treatment of nonmelanoma skin cancer: efficacy and cost comparisons | journal = Dermatologic Surgery | volume = 39 | issue = 9 | pages = 1306–16 | date = Sep 2013 | pmid = 23915332 | doi = 10.1111/dsu.12300 }}</ref> |
|||
If the cancer has [[central nervous system]] involvement, or with meningeal disease, [[intrathecal]] chemotherapy may be administered.<ref name=Corrie /> |
|||
== Adverse effects == |
|||
Chemotherapeutic techniques have a range of side-effects that depend on the type of medications used. The most common medications affect mainly the [[fast-dividing cells]] of the body, such as blood cells and the cells lining the mouth, stomach, and intestines. Chemotherapy-related toxicities can occur acutely after administration, within hours or days, or chronically, from weeks to years.<ref name="isbn0-470-09254-8 2">Airley, p. 265</ref> |
|||
=== Immunosuppression and myelosuppression === |
|||
Virtually all chemotherapeutic regimens can cause depression of the [[immune system]], often by paralysing the [[bone marrow]] and leading to a decrease of [[white blood cell]]s, [[red blood cell]]s, and [[platelet]]s. |
|||
[[Anemia]] and [[thrombocytopenia]], when they occur, are improved with [[blood transfusion]]. [[Neutropenia]] (a decrease of the [[neutrophil granulocyte]] count below 0.5 x 10<sup>9</sup>/[[litre]]) can be improved with synthetic [[G-CSF]] ([[granulocyte]]-colony-stimulating factor, e.g., [[filgrastim]], [[lenograstim]]). |
|||
In very severe [[myelosuppression]], which occurs in some regimens, almost all the bone marrow [[stem cell]]s (cells that produce [[white blood cells|white]] and [[red blood cell]]s) are destroyed, meaning ''allogenic'' or ''[[autologous]]'' [[bone marrow transplant|bone marrow cell transplants]] are necessary. (In autologous BMTs, cells are removed from the patient before the treatment, multiplied and then re-injected afterward; in ''allogenic'' BMTs, the source is a donor.) However, some patients still develop diseases because of this interference with bone marrow.{{citation needed|date=January 2017}} |
|||
Although patients are encouraged to wash their hands, avoid sick people, and take other infection-reducing steps, about 85% of infections are due to naturally occurring microorganisms in the patient's own [[Human gastrointestinal tract|gastrointestinal tract]] (including [[oral cavity]]) and skin.<ref name="internal_medicine_a05">Huang, p. 130</ref> This may manifest as systemic infections, such as [[sepsis]], or as localized outbreaks, such as [[Herpes simplex]], [[shingles]], or other members of the [[human herpes virus|Herpesviridea]].<ref name="HSV">{{cite journal |vauthors=Elad S, Zadik Y, Hewson I, Hovan A, Correa ME, Logan R, Elting LS, Spijkervet FK, Brennan MT | title = A systematic review of viral infections associated with oral involvement in cancer patients: a spotlight on Herpesviridea | journal = Supportive Care in Cancer | volume = 18 | issue = 8 | pages = 993–1006 | date = Aug 2010 | pmid = 20544224 | doi = 10.1007/s00520-010-0900-3 | url = http://www.springerlink.com/content/g476114717852h80/ }}</ref> The risk of illness and death can be reduced by taking common antibiotics such as [[quinolone]] or [[trimethoprim/sulfamethoxazole]] before any fever or sign of infection appears.<ref name=":1">{{Cite journal|last=Gafter-Gvili|first=Anat|last2=Fraser|first2=Abigail|last3=Paul|first3=Mical|last4=Vidal|first4=Liat|last5=Lawrie|first5=Theresa A.|last6=van de Wetering|first6=Marianne D.|last7=Kremer|first7=Leontien C. M.|last8=Leibovici|first8=Leonard|date=2012-01-18|year=|title=Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy|journal=The Cochrane Database of Systematic Reviews|volume=1|pages=CD004386|doi=10.1002/14651858.CD004386.pub3|issn=1469-493X|pmc=4170789|pmid=22258955|via=}}</ref> For every five people who are immunosuppressed following chemotherapy who take an antibiotic, one fever can be prevented; for every 34 who take an antibiotic, one death can be prevented.<ref name=":1" /> Sometimes, chemotherapy treatments are postponed because the immune system is suppressed to a critically low level. |
|||
In [[Japan]], the government has approved the use of some [[medicinal mushrooms]] like ''[[Trametes versicolor]]'', to counteract depression of the immune system in patients undergoing chemotherapy.<ref name="psk">{{cite web|url=http://www.cancer.org/docroot/ETO/content/ETO_5_3X_Coriolous_Versicolor.asp |title=Coriolus Versicolor |publisher=Cancer.org|date=2008-06-10 |accessdate=7 August 2012}}</ref> |
|||
=== Neutropenic enterocolitis === |
|||
Due to immune system suppression, [[neutropenic enterocolitis]] (typhlitis) is a "life-threatening gastrointestinal complication of chemotherapy."<ref>{{cite journal | author = Davila ML | title = Neutropenic enterocolitis | journal = Current Opinion in Gastroenterology | volume = 22 | issue = 1 | pages = 44–7 | date = Jan 2006 | pmid = 16319675 }}</ref> [[Typhlitis]] is an intestinal infection which may manifest itself through symptoms including [[nausea]], [[vomiting]], [[diarrhea]], a [[distended abdomen]], [[fever]], [[chills]], or [[abdominal pain]] and tenderness. |
|||
[[Typhlitis]] is a [[medical emergency]]. It has a very poor [[prognosis]] and is often fatal unless promptly recognized and aggressively treated.<ref name="Keidan 1989 206–9">{{cite journal |vauthors=Keidan RD, Fanning J, Gatenby RA, Weese JL | title = Recurrent typhlitis. A disease resulting from aggressive chemotherapy | journal = Diseases of the Colon and Rectum | volume = 32 | issue = 3 | pages = 206–9 | date = Mar 1989 | pmid = 2920627 | doi = 10.1007/BF02554529 }}</ref> Successful treatment hinges on early diagnosis provided by a high index of suspicion and the use of CT scanning, nonoperative treatment for uncomplicated cases, and sometimes elective right [[hemicolectomy]] to prevent recurrence.<ref name="Keidan 1989 206–9" /> |
|||
=== Gastrointestinal distress === |
|||
[[Nausea]], [[vomiting]], [[Anorexia (symptom)|anorexia]], [[diarrhoea]], abdominal cramps, and [[constipation]] are common side-effects of chemotherapeutic medications that kill fast-dividing cells.<ref name="pmid">{{cite journal |vauthors=Gibson RJ, Keefe DM | title = Cancer chemotherapy-induced diarrhoea and constipation: mechanisms of damage and prevention strategies | journal = Supportive Care in Cancer | volume = 14 | issue = 9 | pages = 890–900 | date = Sep 2006 | pmid = 16604351 | doi = 10.1007/s00520-006-0040-y }}</ref> [[Malnutrition]] and [[dehydration]] can result when the patient does not eat or drink enough, or when the patient vomits frequently, because of gastrointestinal damage. This can result in rapid weight loss, or occasionally in weight gain, if the patient eats too much in an effort to allay nausea or heartburn. Weight gain can also be caused by some steroid medications. These side-effects can frequently be reduced or eliminated with [[antiemetic]] drugs. Self-care measures, such as eating frequent small meals and drinking clear liquids or [[Ginger#Medicinal use|ginger]] tea, are often recommended. In general, this is a temporary effect, and frequently resolves within a week of finishing treatment. However, a high [[index of suspicion]] is appropriate, since [[diarrhea]] and bloating are also symptoms of [[typhlitis]], a very serious and potentially life-threatening [[medical emergency]] that requires immediate treatment. |
|||
=== Anemia === |
|||
[[Anemia]] in cancer patients can be a combined outcome caused by myelosuppressive chemotherapy, and possible cancer-related causes such as [[bleeding]], [[blood cell]] destruction ([[hemolysis]]), hereditary disease, kidney dysfunction, nutritional |
|||
deficiencies and/or [[anemia of chronic disease]]. Treatments to mitigate anemia include hormones to boost blood production ([[erythropoietin]]), [[iron supplement]]s, and [[blood transfusion]]s.<ref name="pmid10511589">{{cite journal |vauthors=Groopman JE, Itri LM | title = Chemotherapy-induced anemia in adults: incidence and treatment | journal = Journal of the National Cancer Institute | volume = 91 | issue = 19 | pages = 1616–34 | date = Oct 1999 | pmid = 10511589 | doi = 10.1093/jnci/91.19.1616 }}</ref><ref name="pmid16925107">{{cite journal | author = Henry DH | title = The role of intravenous iron in cancer-related anemia | journal = Oncology | volume = 20 | issue = 8 Suppl 6 | pages = 21–4 | date = Jul 2006 | pmid = 16925107 | doi = }}</ref><ref name="pmid18597709">{{cite journal |vauthors=Rodgers GM, Becker PS, Bennett CL, Cella D, Chanan-Khan A, Chesney C, Cleeland C, Coccia PF, Djulbegovic B, Garst JL, Gilreath JA, Kraut EH, Lin WC, Matulonis U, Millenson M, Reinke D, Rosenthal J, Sabbatini P, Schwartz RN, Stein RS, Vij R | title = Cancer- and chemotherapy-induced anemia | journal = Journal of the National Comprehensive Cancer Network | volume = 6 | issue = 6 | pages = 536–64 | date = Jul 2008 | pmid = 18597709 | doi = }}</ref> Myelosuppressive therapy can cause a tendency to bleed easily, leading to anemia. Medications that kill rapidly dividing cells or blood cells can reduce the number of [[platelet]]s in the blood, which can result in [[Hematoma|bruises]] and [[Hemorrhage|bleeding]]. Extremely low platelet counts may be temporarily boosted through [[platelet transfusion]]s and new drugs to increase platelet counts during chemotherapy are being developed.<ref name="pmid19245931">{{cite journal | author = Vadhan-Raj S | title = Management of chemotherapy-induced thrombocytopenia: current status of thrombopoietic agents | journal = Seminars in Hematology | volume = 46 | issue = 1 Suppl 2 | pages = S26–32 | date = Jan 2009 | pmid = 19245931 | doi = 10.1053/j.seminhematol.2008.12.007 }}</ref><ref name="pmid16711312">{{cite journal |vauthors=Sekhon SS, Roy V | title = Thrombocytopenia in adults: A practical approach to evaluation and management | journal = Southern Medical Journal | volume = 99 | issue = 5 | pages = 491–8; quiz 499–500, 533 | date = May 2006 | pmid = 16711312 | doi = 10.1097/01.smj.0000209275.75045.d4 }}</ref> Sometimes, chemotherapy treatments are postponed to allow platelet counts to recover. |
|||
=== Fatigue === |
|||
[[Cancer-related fatigue|Fatigue]] may be a consequence of the cancer or its treatment, and can last for months to years after treatment. One physiological cause of fatigue is [[anemia]], which can be caused by chemotherapy, [[surgery]], [[radiotherapy]], primary and metastatic disease and/or nutritional depletion.<ref name="pmid20870636">{{cite journal |vauthors=Berger AM, Abernethy AP, Atkinson A, Barsevick AM, Breitbart WS, Cella D, Cimprich B, Cleeland C, Eisenberger MA, Escalante CP, Jacobsen PB, Kaldor P, Ligibel JA, Murphy BA, O'Connor T, Pirl WF, Rodler E, Rugo HS, Thomas J, Wagner LI | title = Cancer-related fatigue | journal = Journal of the National Comprehensive Cancer Network | volume = 8 | issue = 8 | pages = 904–31 | date = Aug 2010 | pmid = 20870636 | doi = }}</ref><ref name="pmid16500197">{{cite journal |vauthors=Franklin DJ, Packel L | title = Cancer-related fatigue | journal = Archives of Physical Medicine and Rehabilitation | volume = 87 | issue = 3 Suppl 1 | pages = S91–3; quiz S94–5 | date = Mar 2006 | pmid = 16500197 | doi = 10.1016/j.apmr.2005.12.015 }}</ref> [[Anaerobic exercise]] has been found to be beneficial in reducing fatigue in people with [[solid tumour]]s.<ref name="pmid23152233">{{cite journal | author = Cramp F, Byron-Daniel J | title = Exercise for the management of cancer-related fatigue in adults | journal = The Cochrane Database of Systematic Reviews | volume = 11 | issue = | pages = CD006145 | year = 2012 | pmid = 23152233 | doi = 10.1002/14651858.CD006145.pub3 | editor1-last = Cramp | editor1-first = Fiona }}</ref> |
|||
=== Nausea and vomiting === |
|||
{{Further|Chemotherapy-induced nausea and vomiting}} |
|||
[[Nausea]] and [[vomiting]] are two of the most feared cancer treatment-related side-effects for cancer patients and their families. In 1983, Coates et al. found that patients receiving chemotherapy ranked nausea and vomiting as the first and second most severe side-effects, respectively. Up to 20% of patients receiving highly emetogenic agents in this era postponed, or even refused, potentially curative treatments.<ref>{{cite journal | url = http://www.springerlink.com/content/g152223567614560/ | title = Nausea and Vomiting in the Cancer Patient | accessdate = 2 September 2011 | year = 2006 | journal = Oncology | pages = 1482–1496 | doi = 10.1007/0-387-31056-8_83 | quote = Nausea and vomiting are two of the most feared cancer treatment-related side effects for cancer patients and their families. | last1 = Gill | first1 = Paula | last2 = Grothey | first2 = Axel | last3 = Loprinzi | first3 = Charles | isbn = 978-0-387-24291-0 }}</ref> Chemotherapy-induced nausea and vomiting (CINV) are common with many treatments and some forms of cancer. Since the 1990s, several novel classes of [[antiemetics]] have been developed and commercialized, becoming a nearly universal standard in chemotherapy regimens, and helping to successfully manage these symptoms in a large portion of patients. Effective mediation of these unpleasant and sometimes-crippling symptoms results in increased quality of life for the patient and more efficient treatment cycles, due to less stoppage of treatment due to better tolerance by the patient, and due to better overall health of the patient. |
|||
=== Hair loss === |
|||
[[Hair loss]] (Alopecia) can be caused by chemotherapy that kills rapidly dividing cells; other medications may cause hair to thin. These are most often temporary effects: hair usually starts to regrow a few weeks after the last treatment, and can sometimes change colour, texture, thickness and style. Sometimes hair has a tendency to curl after regrowth, resulting in "chemo curls." Severe hair loss occurs most often with drugs such as [[doxorubicin]], [[daunorubicin]], [[paclitaxel]], [[docetaxel]], [[cyclophosphamide]], [[ifosfamide]] and [[etoposide]]. Permanent thinning or hair loss can result from some standard chemotherapy regimens. |
|||
Chemotherapy induced hair loss occurs by a non-androgenic mechanism, and can manifest as [[alopecia totalis]], telogen effluvium, or less often [[alopecia areata]].<ref name="pmid17642856">{{cite journal |vauthors=Chadha V, Shenoi SD | title = Hair loss in cancer chemotherapeutic patients | journal = Indian Journal of Dermatology, Venereology and Leprology | volume = 69 | issue = 2 | pages = 131–132 | year = 2003 | pmid = 17642856 }}</ref> It is usually associated with systemic treatment due to the high mitotic rate of hair follicles, and more reversible than androgenic hair loss,<ref name="pmid23187775">{{cite journal | author = Lemieux J | title = Reducing chemotherapy-induced alopecia with scalp cooling | journal = Clinical Advances in Hematology & Oncology | volume = 10 | issue = 10 | pages = 681–682 | date = Oct 2012 | pmid = 23187775 }}</ref><ref>{{cite journal |vauthors=Shapiro J, Price VH | title = Hair regrowth. Therapeutic agents | journal = Dermatologic Clinics | volume = 16 | issue = 2 | pages = 341–356 | date = Apr 1998 | pmid = 9589208 | doi = 10.1016/S0733-8635(05)70017-6 }}</ref> although permanent cases can occur.<ref>{{cite journal |vauthors=Al-Mohanna H, Al-Khenaizan S | title = Permanent alopecia following cranial irradiation in a child | journal = Journal of Cutaneous Medicine and Surgery | volume = 14 | issue = 3 | pages = 141–143 | year = 2010 | pmid = 20487675 | doi=10.2310/7750.2010.09014}}</ref> Chemotherapy induces hair loss in women more often than men.<ref>{{cite journal |vauthors=Can G, Demir M, Erol O, Aydiner A | title = A comparison of men and women's experiences of chemotherapy-induced alopecia | journal = European Journal of Oncology Nursing | volume = 17 | issue = 3 | pages = 255–60 | date = Jun 2013 | pmid = 22901547 | pmc = | doi = 10.1016/j.ejon.2012.06.003 }}</ref> |
|||
[[Hypothermia cap|Scalp cooling]] offers a means of preventing both permanent and temporary hair loss; however, concerns about this method have been raised.<ref name="pmid19341937">{{cite journal | author = Trüeb RM | title = Chemotherapy-induced alopecia | journal = Seminars in Cutaneous Medicine and Surgery | volume = 28 | issue = 1 | pages = 11–4 | date = Mar 2009 | pmid = 19341937 | doi = 10.1016/j.sder.2008.12.001 }}</ref><ref name="pmid22178150">{{cite journal |vauthors=Chon SY, Champion RW, Geddes ER, Rashid RM | title = Chemotherapy-induced alopecia | journal = Journal of the American Academy of Dermatology | volume = 67 | issue = 1 | pages = e37–47 | date = Jul 2012 | pmid = 22178150 | doi = 10.1016/j.jaad.2011.02.026 }}</ref> |
|||
=== Secondary neoplasm === |
|||
Development of secondary neoplasia after successful chemotherapy and/or radiotherapy treatment can occur. The most common [[secondary neoplasm]] is secondary acute myeloid leukemia, which develops primarily after treatment with alkylating agents or topoisomerase inhibitors.<ref>U. Rüther, C. Nunnensiek, H.-J. Schmoll,''Secondary Neoplasias following Chemotherapy, Radiotherapy, and Immunosuppression'', Contributions to Oncology (Beiträge zur Onkologie); Vol 55, 2000, {{ISBN|3-8055-7116-X}}</ref> Survivors of [[childhood cancer]] are more than 13 times as likely to get a [[secondary neoplasm]] during the 30 years after treatment than the general population.<ref>{{cite journal |vauthors=Hijiya N, Hudson MM, Lensing S, Zacher M, Onciu M, Behm FG, Razzouk BI, Ribeiro RC, Rubnitz JE, Sandlund JT, Rivera GK, Evans WE, Relling MV, Pui CH | title = Cumulative incidence of secondary neoplasms as a first event after childhood acute lymphoblastic leukemia | journal = JAMA | volume = 297 | issue = 11 | pages = 1207–1215 | date = Mar 2007 | pmid = 17374815 | doi = 10.1001/jama.297.11.1207 }}</ref> Not all of this increase can be attributed to chemotherapy. |
|||
=== Infertility === |
|||
Some types of chemotherapy are gonadotoxic and may cause [[infertility]].<ref name=Brydoy>{{cite journal |vauthors=Brydøy M, Fosså SD, Dahl O, Bjøro T | title = Gonadal dysfunction and fertility problems in cancer survivors | journal = Acta Oncologica | volume = 46 | issue = 4 | pages = 480–9 | year = 2007 | pmid = 17497315 | doi = 10.1080/02841860601166958 | url = http://informahealthcare.com/doi/pdf/10.1080/02841860601166958 }}</ref> Chemotherapies with high risk include procarbazine and other alkylating drugs such as cyclophosphamide, ifosfamide, busulfan, melphalan, chlorambucil, and chlormethine.<ref name=Brydoy /> Drugs with medium risk include doxorubicin and platinum analogs such as cisplatin and carboplatin.<ref name=Brydoy /> On the other hand, therapies with low risk of gonadotoxicity include plant derivatives such as vincristine and vinblastine, [[antibiotics]] such as bleomycin and dactinomycin, and antimetabolites such as methotrexate, mercaptopurine, and 5-fluorouracil.<ref name=Brydoy /> |
|||
[[Female infertility]] by chemotherapy appears to be secondary to [[premature ovarian failure]] by loss of [[primordial follicles]].<ref name=Morgan2012>{{cite journal |vauthors=Morgan S, Anderson RA, Gourley C, Wallace WH, Spears N | title = How do chemotherapeutic agents damage the ovary? | journal = Human Reproduction Update | volume = 18 | issue = 5 | pages = 525–35 | year = 2012 | pmid = 22647504 | doi = 10.1093/humupd/dms022 }}</ref> This loss is not necessarily a direct effect of the chemotherapeutic agents, but could be due to an increased rate of growth initiation to replace damaged developing follicles.<ref name=Morgan2012 /> |
|||
Patients may choose between several methods of [[fertility preservation]] prior to chemotherapy, including [[cryopreservation]] of semen, ovarian tissue, oocytes, or embryos.<ref>{{cite journal |vauthors=Gurgan T, Salman C, Demirol A | title = Pregnancy and assisted reproduction techniques in men and women after cancer treatment | journal = Placenta | volume = 29 Suppl B | issue = | pages = 152–9 | date = Oct 2008 | pmid = 18790328 | doi = 10.1016/j.placenta.2008.07.007 }}</ref> As more than half of cancer patients are elderly, this adverse effect is only relevant for a minority of patients. A study in France between 1999 and 2011 came to the result that embryo freezing before administration of gonadotoxic agents to females caused a delay of treatment in 34% of cases, and a live birth in 27% of surviving cases who wanted to become pregnant, with the follow-up time varying between 1 and 13 years.<ref>{{cite journal |vauthors=Courbiere B, Decanter C, Bringer-Deutsch S, Rives N, Mirallié S, Pech JC, De Ziegler D, Carré-Pigeon F, May-Panloup P, Sifer C, Amice V, Schweitzer T, Porcu-Buisson G, Poirot C | title = Emergency IVF for embryo freezing to preserve female fertility: a French multicentre cohort study | journal = Human Reproduction | volume = 28 | issue = 9 | pages = 2381–8 | date = Sep 2013 | pmid = 23832792 | pmc = | doi = 10.1093/humrep/det268 }}</ref> |
|||
Potential protective or attenuating agents include [[GnRH analog]]s, where several studies have shown a protective effect ''[[in vivo]]'' in humans, but some studies show no such effect. [[Sphingosine-1-phosphate]] (S1P) has shown similar effect, but its mechanism of inhibiting the [[Sphingomyelin#Apoptosis|sphingomyelin apoptotic pathway]] may also interfere with the [[apoptosis]] action of chemotherapy drugs.<ref name="RonessKalich-Philosoph2014">{{cite journal |vauthors=Roness H, Kalich-Philosoph L, Meirow D | title = Prevention of chemotherapy-induced ovarian damage: possible roles for hormonal and non-hormonal attenuating agents | journal = Human Reproduction Update | volume = 20 | issue = 5 | pages = 759–774 | year = 2014 | pmid = 24833728 | doi = 10.1093/humupd/dmu019 }}</ref> |
|||
In chemotherapy as a [[conditioning regimen]] in hematopoietic stem cell transplantation, a study of patients conditioned with cyclophosphamide alone for severe aplastic anemia came to the result that ovarian recovery occurred in all women younger than 26 years at time of transplantation, but only in five of 16 women older than 26 years.<ref>{{cite journal |vauthors=Tichelli A, Rovó A | title = Fertility issues following hematopoietic stem cell transplantation | journal = Expert Review of Hematology | volume = 6 | issue = 4 | pages = 375–388 | date = Aug 2013 | pmid = 23991924 | doi = 10.1586/17474086.2013.816507 | url = http://www.medscape.com/viewarticle/810686_2?nlid=34365_904 }} |
|||
<br />In turn citing: {{cite journal |vauthors=Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ, Doney K, Storb R, Sullivan K, Witherspoon R, Appelbaum FR | title = Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation | journal = Blood | volume = 87 | issue = 7 | pages = 3045–3052 | date = Apr 1996 | pmid = 8639928 }}</ref> |
|||
=== Teratogenicity === |
|||
Chemotherapy is [[teratogenic]] during [[pregnancy]], especially during the [[first trimester]], to the extent that [[abortion]] usually is recommended if pregnancy in this period is found during chemotherapy.<ref name=arnon2011>{{cite journal |vauthors=Arnon J, Meirow D, Lewis-Roness H, Ornoy A | title = Genetic and teratogenic effects of cancer treatments on gametes and embryos | journal = Human Reproduction Update | volume = 7 | issue = 4 | pages = 394–403 | year = 2001 | pmid = 11476352 | doi = 10.1093/humupd/7.4.394 }} [http://humupd.oxfordjournals.org/content/7/4/394.full.pdf]</ref> Second- and third-trimester exposure does not usually increase the teratogenic risk and adverse effects on cognitive development, but it may increase the risk of various [[complications of pregnancy]] and fetal myelosuppression.<ref name=arnon2011 /> |
|||
In males previously having undergone chemotherapy or radiotherapy, there appears to be no increase in genetic defects or congenital malformations in their children conceived after therapy.<ref name=arnon2011 /> The use of [[assisted reproductive technologies]] and [[micromanipulation technique]]s might increase this risk.<ref name=arnon2011 /> In females previously having undergone chemotherapy, miscarriage and congenital malformations are not increased in subsequent conceptions.<ref name=arnon2011 /> However, when [[in vitro fertilization]] and [[embryo cryopreservation]]is practised between or shortly after treatment, possible genetic risks to the growing oocytes exist, and hence it has been recommended that the babies be screened.<ref name=arnon2011 /> |
|||
=== Peripheral neuropathy === |
|||
{{further|Chemotherapy-induced peripheral neuropathy}} |
|||
Between 30 and 40 percent of patients undergoing chemotherapy experience [[chemotherapy-induced peripheral neuropathy]] (CIPN), a progressive, enduring, and often irreversible condition, causing pain, tingling, numbness and sensitivity to cold, beginning in the hands and feet and sometimes progressing to the arms and legs.<ref name = NCI>{{vcite journal | author = del Pino BM | date = Feb 23, 2010 | journal = NCI Cancer Bulletin | volume = 7 | issue = 4 | page = 6 | title = Chemotherapy-induced Peripheral Neuropathy | url = http://www.cancer.gov/cancertopics/research/chemotherapy-induced-peripheral-neuropathy}}</ref> Chemotherapy drugs associated with CIPN include [[thalidomide]], [[epothilone]]s, [[vinca alkaloid]]s, [[taxane]]s, [[proteasome inhibitor]]s, and the platinum-based drugs.<ref name = NCI /><ref>{{vcite journal|url=http://www.kup.at/kup/pdf/10376.pdf|author=Grisold W, Oberndorfer S, Windebank AJ|journal=European Association of Neurooncology Magazine|title=Chemotherapy and polyneuropathies|year=2012|volume=12|issue=1}}</ref><ref>http://www.ehealthme.com/ds/herceptin/peripheral%20sensory%20neuropathy</ref> Whether CIPN arises, and to what degree, is determined by the choice of drug, duration of use, the total amount consumed and whether the patient already has [[peripheral neuropathy]]. Though the symptoms are mainly sensory, in some cases [[motor nerve]]s and the [[autonomic nervous system]] are affected.<ref name=Beijers>{{vcite journal|author=Beijers AJM, Jongen, JLM & Vreugdenhil1 G |date=January 2012 |journal=The Netherlands journal of medicine |volume=70 |issue=1 |pmid=22271810 |url=http://www.njmonline.nl/getpdf.php?id=10000794 |deadurl=yes |archiveurl=https://web.archive.org/web/20131203001320/http://www.njmonline.nl/getpdf.php?id=10000794 |archivedate=3 December 2013 |df=dmy }}</ref> CIPN often follows the first chemotherapy dose and increases in severity as treatment continues, but this progression usually levels off at completion of treatment. The platinum-based drugs are the exception; with these drugs, sensation may continue to deteriorate for several months after the end of treatment.<ref name= Windebank>{{vcite journal | author = Windebank AJ & Grisold W | title = Chemotherapy-induced neuropathy | journal = Journal of the Peripheral Nervous System | date = 2008 Mar | volume = 13 | issue = 1 | pages = 27–46 | pmid = 18346229 | doi=10.1111/j.1529-8027.2008.00156.x}}</ref> Some CIPN appears to be irreversible.<ref name= Windebank /> Pain can often be managed with drug or other treatment but the numbness is usually resistant to treatment.<ref name=Savage>{{vcite journal | journal = Journal of the National Cancer Institute| title = Chemotherapy-induced pain puzzles scientists | volume = 99 | issue = 14 | author = Savage L | date = 2007 | url = http://jnci.oxfordjournals.org/content/99/14/1070.long | pages = 1070–1071 | doi=10.1093/jnci/djm072 | pmid=17623791}}</ref> |
|||
=== Cognitive impairment === |
|||
Some patients report fatigue or non-specific neurocognitive problems, such as an inability to concentrate; this is sometimes called [[post-chemotherapy cognitive impairment]], referred to as "chemo brain" by patients' groups.<ref name="pmid15169812">{{cite journal |vauthors=Tannock IF, Ahles TA, Ganz PA, Van Dam FS | title = Cognitive impairment associated with chemotherapy for cancer: report of a workshop | journal = Journal of Clinical Oncology | volume = 22 | issue = 11 | pages = 2233–9 | date = Jun 2004 | pmid = 15169812 | doi = 10.1200/JCO.2004.08.094 | url = http://www.jco.org/cgi/pmidlookup?view=long&pmid=15169812 }}</ref> |
|||
=== Tumor lysis syndrome === |
|||
In particularly large tumors and cancers with high [[white cell count]]s, such as [[lymphoma]]s, [[teratoma]]s, and some [[leukemia]]s, some patients develop [[tumor lysis syndrome]]. The rapid breakdown of cancer cells causes the release of chemicals from the inside of the cells. Following this, high levels of [[hyperuricemia|uric acid]], [[hyperkalemia|potassium]] and [[hyperphosphatemia|phosphate]] are found in the blood. High levels of phosphate induce secondary hypoparathyroidism, resulting in low levels of calcium in the blood. This causes kidney damage and the high levels of potassium can cause [[Cardiac dysrhythmia|cardiac arrhythmia]]. Although prophylaxis is available and is often initiated in patients with large tumors, this is a dangerous side-effect that can lead to death if left untreated.<ref name="isbn0-443-07101-2 4">Wood, p. 202</ref> |
|||
=== Organ damage === |
|||
[[Cardiotoxicity]] (heart damage) is especially prominent with the use of [[anthracycline]] drugs ([[doxorubicin]], [[epirubicin]], [[idarubicin]], and [[liposomal doxorubicin]]). The cause of this is most likely due to the production of [[free radical]]s in the cell and subsequent [[DNA damage]]. Other chemotherapeutic agents that cause cardiotoxicity, but at a lower incidence, are [[cyclophosphamide]], [[docetaxel]] and [[clofarabine]].<ref name="pmid22382639">{{cite journal |vauthors=Shaikh AY, Shih JA | title = Chemotherapy-induced cardiotoxicity | journal = Current Heart Failure Reports | volume = 9 | issue = 2 | pages = 117–27 | date = Jun 2012 | pmid = 22382639 | doi = 10.1007/s11897-012-0083-y }}</ref> |
|||
[[Hepatotoxicity]] (liver damage) can be caused by many cytotoxic drugs. The susceptibility of an individual to liver damage can be altered by other factors such as the cancer itself, [[viral hepatitis]], [[immunosuppression]] and [[nutritional deficiency]]. The liver damage can consist of damage to liver cells, [[Hepatic veno-occlusive disease|hepatic sinusoidal syndrome]] (obstruction of the veins in the liver), [[cholestasis]] (where bile does not flow from the liver to the intestine) and [[liver fibrosis]].<ref>{{cite journal |vauthors=Thatishetty AV, Agresti N, O'Brien CB | title = Chemotherapy-induced hepatotoxicity | journal = Clinics in Liver Disease | volume = 17 | issue = 4 | pages = 671–86, ix–x | date = Nov 2013 | pmid = 24099024 | doi = 10.1016/j.cld.2013.07.010 | url = http://dx.doi.org/10.1016/j.cld.2013.07.010 }}</ref><ref name="pmid11306728">{{cite journal |vauthors=King PD, Perry MC | title = Hepatotoxicity of chemotherapy | journal = The Oncologist | volume = 6 | issue = 2 | pages = 162–76 | year = 2001 | pmid = 11306728 | doi = 10.1634/theoncologist.6-2-162 }}</ref> |
|||
[[Nephrotoxicity]] (kidney damage) can be caused by [[tumor lysis syndrome]] and also due direct effects of drug clearance by the kidneys. Different drugs will affect different parts of the kidney and the toxicity may be [[asymptomatic]] (only seen on blood or urine tests) or may cause [[acute renal failure]].<ref name="pmid16473645">{{cite journal |vauthors=de Jonge MJ, Verweij J | title = Renal toxicities of chemotherapy | journal = Seminars in Oncology | volume = 33 | issue = 1 | pages = 68–73 | date = Feb 2006 | pmid = 16473645 | doi = 10.1053/j.seminoncol.2005.11.011 }}</ref><ref name="pmid15574506">{{cite journal |vauthors=Humphreys BD, Soiffer RJ, Magee CC | title = Renal failure associated with cancer and its treatment: an update | journal = Journal of the American Society of Nephrology | volume = 16 | issue = 1 | pages = 151–61 | date = Jan 2005 | pmid = 15574506 | doi = 10.1681/ASN.2004100843 }}</ref> |
|||
[[Ototoxicity]] (damage to the inner ear) is a common side effect of platinum based drugs that can produce symptoms such as dizziness and [[Vertigo (medical)|vertigo]].<ref name="pmid22547603">{{cite journal |vauthors=Brock PR, Knight KR, Freyer DR, Campbell KC, Steyger PS, Blakley BW, Rassekh SR, Chang KW, Fligor BJ, Rajput K, Sullivan M, Neuwelt EA | title = Platinum-induced ototoxicity in children: a consensus review on mechanisms, predisposition, and protection, including a new International Society of Pediatric Oncology Boston ototoxicity scale | journal = Journal of Clinical Oncology | volume = 30 | issue = 19 | pages = 2408–17 | date = Jul 2012 | pmid = 22547603 | pmc = 3675696 | doi = 10.1200/JCO.2011.39.1110 }}</ref><ref name="pmid19851045">{{cite journal |vauthors=Rybak LP, Mukherjea D, Jajoo S, Ramkumar V | title = Cisplatin ototoxicity and protection: clinical and experimental studies | journal = The Tohoku Journal of Experimental Medicine | volume = 219 | issue = 3 | pages = 177–86 | date = Nov 2009 | pmid = 19851045 | pmc = 2927105 | doi = 10.1620/tjem.219.177 }}</ref> |
|||
=== Other side-effects === |
|||
Less common side-effects include red skin ([[erythema]]), dry skin, damaged fingernails, a dry mouth ([[xerostomia]]), [[Water retention (medicine)|water retention]], and [[sexual impotence]]. Some medications can trigger [[allergic]] or [[pseudoallergic]] reactions. |
|||
Specific chemotherapeutic agents are associated with organ-specific toxicities, including [[cardiovascular disease]] (e.g., [[doxorubicin]]), [[interstitial lung disease]] (e.g., [[bleomycin]]) and occasionally [[secondary neoplasm]] (e.g., [[MOPP (medicine)|MOPP]] therapy for Hodgkin's disease). |
|||
== Limitations == |
|||
Chemotherapy does not always work, and even when it is useful, it may not completely destroy the cancer. Patients frequently fail to understand its limitations. In one study of patients who had been newly diagnosed with incurable, [[Stage-4 cancer|stage 4 cancer]], more than two-thirds of patients with lung cancer and more than four-fifths of patients with colorectal cancer still believed that chemotherapy was likely to cure their cancer.<ref name=Weeks>{{cite journal |vauthors=Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, Schrag D | title = Patients' expectations about effects of chemotherapy for advanced cancer | journal = The New England Journal of Medicine | volume = 367 | issue = 17 | pages = 1616–25 | date = Oct 2012 | pmid = 23094723 | pmc = 3613151 | doi = 10.1056/NEJMoa1204410 }}</ref> |
|||
The [[blood–brain barrier]] poses a difficult obstacle to pass to deliver chemotherapy to the [[brain]]. This is because the brain has an extensive system in place to protect it from harmful chemicals. Drug transporters can pump out drugs from the brain and brain's blood vessel cells into the [[cerebrospinal fluid]] and blood circulation. These transporters pump out most chemotherapy drugs, which reduces their efficacy for treatment of brain tumors. Only small [[lipophilic]] [[alkylating agents]] such as [[lomustine]] or [[temozolomide]] are able to cross this blood–brain barrier.<ref name="pmid17363519">{{cite journal |vauthors=Deeken JF, Löscher W | title = The blood-brain barrier and cancer: transporters, treatment, and Trojan horses | journal = Clinical Cancer Research | volume = 13 | issue = 6 | pages = 1663–74 | date = Mar 2007 | pmid = 17363519 | doi = 10.1158/1078-0432.CCR-06-2854 }}</ref><ref name="pmid10794805">{{cite journal |vauthors=Agarwala SS, Kirkwood JM | title = Temozolomide, a novel alkylating agent with activity in the central nervous system, may improve the treatment of advanced metastatic melanoma | journal = The Oncologist | volume = 5 | issue = 2 | pages = 144–51 | year = 2000 | pmid = 10794805 | doi = 10.1634/theoncologist.5-2-144 }}</ref><ref name="pmid17538177">{{cite journal |vauthors=Gerstner ER, Fine RL | title = Increased permeability of the blood-brain barrier to chemotherapy in metastatic brain tumors: establishing a treatment paradigm | journal = Journal of Clinical Oncology | volume = 25 | issue = 16 | pages = 2306–12 | date = Jun 2007 | pmid = 17538177 | doi = 10.1200/JCO.2006.10.0677 }}</ref> |
|||
[[Blood vessel]]s in tumors are very different from those seen in normal tissues. As a tumor grows, tumor cells furthest away from the blood vessels become low in oxygen ([[Tumor hypoxia|hypoxic]]). To counteract this they then signal for new blood vessels to grow. The newly formed tumor vasculature is poorly formed and does not deliver an adequate blood supply to all areas of the tumor. This leads to issues with drug delivery because many drugs will be delivered to the tumor by the [[circulatory system]].<ref name="pmid16862189">{{cite journal |vauthors=Minchinton AI, Tannock IF | title = Drug penetration in solid tumours | journal = Nature Reviews. Cancer | volume = 6 | issue = 8 | pages = 583–92 | date = Aug 2006 | pmid = 16862189 | doi = 10.1038/nrc1893 }}</ref> |
|||
== Resistance == |
|||
[[Drug resistance|Resistance]] is a major cause of treatment failure in chemotherapeutic drugs. There are a few possible causes of resistance in cancer, one of which is the presence of small pumps on the surface of cancer cells that actively move chemotherapy from inside the cell to the outside. Cancer cells produce high amounts of these pumps, known as [[p-glycoprotein]], in order to protect themselves from chemotherapeutics. Research on [[p-glycoprotein]] and other such chemotherapy efflux pumps is currently ongoing. Medications to inhibit the function of [[p-glycoprotein]] are undergoing investigation, but due to toxicities and interactions with anti-cancer drugs their development has been difficult.<ref name="pmid12591977">{{cite journal | author = Goldman B | title = Multidrug resistance: can new drugs help chemotherapy score against cancer? | journal = Journal of the National Cancer Institute | volume = 95 | issue = 4 | pages = 255–7 | date = Feb 2003 | pmid = 12591977 | doi = 10.1093/jnci/95.4.255 }}</ref><ref>{{cite book | name-list-format = vanc |author1=E. Crowley |author2=CA. McDevitt |author3=R. Callaghan |title=Multidrug Resistance in Cancer. Generating Inhibitors of P-Glycoprotein: Where to, Now?|year=2009|publisher=Springer Protocols|pages=405–432}}</ref> Another mechanism of resistance is [[gene duplication|gene amplification]], a process in which multiple copies of a gene are produced by cancer cells. This overcomes the effect of drugs that reduce the expression of genes involved in replication. With more copies of the gene, the drug can not prevent all expression of the gene and therefore the cell can restore its proliferative ability. Cancer cells can also cause defects in the cellular pathways of [[apoptosis]] (programmed cell death). As most chemotherapy drugs kill cancer cells in this manner, defective apoptosis allows survival of these cells, making them resistant. Many chemotherapy drugs also cause DNA damage, which can be repaired by [[enzyme]]s in the cell that carry out [[DNA repair]]. Upregulation of these genes can overcome the DNA damage and prevent the induction of apoptosis. Mutations in genes that produce drug target proteins, such as [[tubulin]], can occur which prevent the drugs from binding to the protein, leading to resistance to these types of drugs.<ref name="pmid16103712">{{cite journal | author = Luqmani YA | title = Mechanisms of drug resistance in cancer chemotherapy | journal = Medical Principles and Practice | volume = 14 Suppl 1 | issue = | pages = 35–48 | year = 2005 | pmid = 16103712 | doi = 10.1159/000086183 }}</ref> Drugs used in chemotherapy can induce cell stress, which can kill a cancer cell; however, under certain conditions, cells stress can induce changes in gene expression that enables resistance to several types of drugs.<ref>{{cite journal|last1=Moschovi|first1=Maria|title=Drugs acting on homeostasis: challenging cancer cell adaptation.|journal=Expert Rev Anticancer Ther.|volume=15|issue=12|pages=1405–17|doi=10.1586/14737140.2015.1095095|pmid=26523494|url=http://www.tandfonline.com/doi/abs/10.1586/14737140.2015.1095095?journalCode=iery20|year=2015}}</ref> |
|||
== Cytotoxics and targeted therapies == |
|||
[[Targeted therapy|Targeted therapies]] are a relatively new class of cancer drugs that can overcome many of the issues seen with the use of cytotoxics. They are divided into two groups: small molecule and antibodies. The massive toxicity seen with the use of cytotoxics is due to the lack of cell specificity of the drugs. They will kill any rapidly dividing cell, tumor or normal. Targeted therapies are designed to affect cellular proteins or processes that are utilised by the cancer cells. This allows a high dose to cancer tissues with a relatively low dose to other tissues. As different proteins are utilised by different cancer types, the targeted therapy drugs are used on a cancer type specific, or even on a patient specific basis. Although the [[adverse effects|side effects]] are often less severe than that seen of cytotoxic chemotherapeutics, life-threatening effects can occur. Initially, the targeted therapeutics were supposed to be solely selective for one protein. Now it is clear that there is often a range of protein targets that the drug can bind. An example target for targeted therapy is the protein produced by the [[Philadelphia chromosome]], a genetic lesion found commonly in [[chronic myelomonocytic leukemia]]. This fusion protein has enzyme activity that can be inhibited by [[imatinib]], a [[small molecule]] drug.<ref name="pmid18297955">{{cite journal | author = Gerber DE | title = Targeted therapies: a new generation of cancer treatments | journal = American Family Physician | volume = 77 | issue = 3 | pages = 311–9 | date = Feb 2008 | pmid = 18297955 | doi = }}</ref><ref name="pmid12360278">{{cite journal | author = Allen TM | title = Ligand-targeted therapeutics in anticancer therapy | journal = Nature Reviews. Cancer | volume = 2 | issue = 10 | pages = 750–63 | date = Oct 2002 | pmid = 12360278 | doi = 10.1038/nrc903 }}</ref><ref name="pmid19581909">{{cite journal |vauthors=Chen HX, Cleck JN | title = Adverse effects of anticancer agents that target the VEGF pathway | journal = Nature Reviews. Clinical Oncology | volume = 6 | issue = 8 | pages = 465–77 | date = Aug 2009 | pmid = 19581909 | doi = 10.1038/nrclinonc.2009.94 }}</ref><ref name="pmid19104514">{{cite journal |vauthors=Zhang J, Yang PL, Gray NS | title = Targeting cancer with small molecule kinase inhibitors | journal = Nature Reviews. Cancer | volume = 9 | issue = 1 | pages = 28–39 | date = Jan 2009 | pmid = 19104514 | doi = 10.1038/nrc2559 }}</ref> |
|||
== Mechanism of action == |
|||
[[File:Cell cycle simple.png|thumb|The four phases of the cell cycle. G1 – the initial growth phase. S – the phase in which DNA is synthesised. G2 – the second growth phase in preparation for cell division. M – mitosis; where the cell divides to produce two daughter cells that continue the cell cycle.]] |
|||
[[Cancer]] is the uncontrolled growth of [[cell (biology)|cells]] coupled with [[malignant]] behaviour: invasion and [[metastasis]] (among other features).<ref name="pmid10647931">{{cite journal |vauthors=Hanahan D, Weinberg RA | title = The hallmarks of cancer | journal = Cell | volume = 100 | issue = 1 | pages = 57–70 | date = Jan 2000 | pmid = 10647931 | doi = 10.1016/S0092-8674(00)81683-9 }}</ref> It is caused by the interaction between [[gene]]tic susceptibility and environmental factors.<ref name="pmid18196605">{{cite journal | author = Hodgson S | title = Mechanisms of inherited cancer susceptibility | journal = Journal of Zhejiang University. Science. B | volume = 9 | issue = 1 | pages = 1–4 | date = Jan 2008 | pmid = 18196605 | pmc = 2170461 | doi = 10.1631/jzus.B073001 }}</ref><ref name="pmid9353182">{{cite journal | author = Perera FP | title = Environment and cancer: who are susceptible? | journal = Science | volume = 278 | issue = 5340 | pages = 1068–73 | date = Nov 1997 | pmid = 9353182 | doi = 10.1126/science.278.5340.1068 | bibcode = 1997Sci...278.1068P }}</ref> These factors lead to accumulations of [[genetic mutation]]s in [[oncogene]]s (genes that control the growth rate of cells) and [[tumor suppressor gene]]s (genes that help to prevent cancer), which gives cancer cells their malignant characteristics, such as uncontrolled growth.<ref>Randall, pp, 93-94</ref> |
|||
In the broad sense, most chemotherapeutic drugs work by impairing [[mitosis]] ([[cell division]]), effectively targeting [[fast-dividing cells]]. As these drugs cause damage to cells, they are termed ''cytotoxic''. They prevent mitosis by various mechanisms including damaging DNA and inhibition of the cellular machinery involved in cell division.<ref name="pmid14508075">{{cite journal |vauthors=Malhotra V, Perry MC | title = Classical chemotherapy: mechanisms, toxicities and the therapeutic window | journal = Cancer Biology & Therapy | volume = 2 | issue = 4 Suppl 1 | pages = S2–4 | year = 2003 | pmid = 14508075 | doi=10.4161/cbt.199}}</ref><ref name="pmid19651324">{{cite journal |vauthors=Kehe K, Balszuweit F, Steinritz D, Thiermann H | title = Molecular toxicology of sulfur mustard-induced cutaneous inflammation and blistering | journal = Toxicology | volume = 263 | issue = 1 | pages = 12–9 | date = Sep 2009 | pmid = 19651324 | doi = 10.1016/j.tox.2009.01.019 }}</ref> One theory as to why these drugs kill cancer cells is that they induce a programmed form of cell death known as [[apoptosis]].<ref name="pmid10928287">{{cite journal |vauthors=Makin G, Hickman JA | title = Apoptosis and cancer chemotherapy | journal = Cell and Tissue Research | volume = 301 | issue = 1 | pages = 143–52 | date = Jul 2000 | pmid = 10928287 | doi = 10.1007/s004419900160 | bibcode = 1994RSPTB.345..319H }}</ref> |
|||
As chemotherapy affects cell division, tumors with high [[proliferative index|growth rates]] (such as [[acute myelogenous leukemia]] and the aggressive [[lymphoma]]s, including [[Hodgkin's disease]]) are more sensitive to chemotherapy, as a larger proportion of the targeted cells are undergoing [[cell division]] at any time. Malignancies with slower growth rates, such as [[Indolent condition|indolent]] lymphomas, tend to respond to chemotherapy much more modestly.<ref name=Corrie>{{cite journal|last=Corrie PG|title=Cytotoxic chemotherapy: clinical aspects|journal=Medicine|year=2008|volume=36|issue=1|pages=24–28|doi=10.1016/j.mpmed.2007.10.012|first1=Pippa G.}}</ref> [[Tumour heterogeneity|Heterogeneic tumours]] may also display varying sensitivities to chemotherapy agents, depending on the subclonal populations within the tumor. |
|||
== Other uses == |
|||
Some chemotherapy drugs are used in diseases other than cancer, such as in autoimmune disorders,<ref name="pmid15100330" /> and noncancerous [[plasma cell dyscrasia]]. In some cases they are often used at lower doses, which means that the side effects are minimized,<ref name="pmid15100330">{{cite journal | author = Ben-Ari ET | title = Dual purpose: some cancer therapies used to treat autoimmune diseases | journal = Journal of the National Cancer Institute | volume = 96 | issue = 8 | pages = 577–9 | date = Apr 2004 | pmid = 15100330 | doi = 10.1093/jnci/96.8.577 }}</ref> while in other cases doses similar to ones used to treat cancer are used. [[Methotrexate]] is used in the treatment of [[rheumatoid arthritis]] (RA),<ref name="pmid11454634">{{cite journal |vauthors=Cutolo M, Sulli A, Pizzorni C, Seriolo B, Straub RH | title = Anti-inflammatory mechanisms of methotrexate in rheumatoid arthritis | journal = Annals of the Rheumatic Diseases | volume = 60 | issue = 8 | pages = 729–35 | date = Aug 2001 | pmid = 11454634 | pmc = 1753808 | doi = 10.1136/ard.60.8.729 }}</ref> [[psoriasis]],<ref name="pmid21388454">{{cite journal |vauthors=Montaudié H, Sbidian E, Paul C, Maza A, Gallini A, Aractingi S, Aubin F, Bachelez H, Cribier B, Joly P, Jullien D, Le Maître M, Misery L, Richard MA, Ortonne JP | title = Methotrexate in psoriasis: a systematic review of treatment modalities, incidence, risk factors and monitoring of liver toxicity | journal = Journal of the European Academy of Dermatology and Venereology | volume = 25 Suppl 2 | issue = | pages = 12–8 | date = May 2011 | pmid = 21388454 | doi = 10.1111/j.1468-3083.2011.03991.x }}</ref> [[ankylosing spondylitis]]<ref name="pmid23450553">{{cite journal | author = Chen J, Veras MM, Liu C, Lin J | title = Methotrexate for ankylosing spondylitis | journal = The Cochrane Database of Systematic Reviews | volume = 2 | issue = | pages = CD004524 | year = 2013 | pmid = 23450553 | doi = 10.1002/14651858.CD004524.pub4 | editor1-last = Chen | editor1-first = Junmin }}</ref> and [[multiple sclerosis]].<ref name="pmid15106195" /><ref name="pmid16900766" /> The anti-inflammatory response seen in RA is thought to be due to increases in [[adenosine]], which causes [[immunosuppression]]; effects on immuno-regulatory [[cyclooxygenase]]-2 enzyme pathways; reduction in pro-inflammatory [[cytokine]]s; and anti-proliferative properties.<ref name="pmid11454634" /> Although methotrexate is used to treat both multiple sclerosis and ankylosing spondylitis, its efficacy in these diseases is still uncertain.<ref name="pmid23450553" /><ref name="pmid15106195">{{cite journal | author = Gray O, McDonnell GV, Forbes RB | title = Methotrexate for multiple sclerosis | journal = The Cochrane Database of Systematic Reviews | volume = | issue = 2 | pages = CD003208 | year = 2004 | pmid = 15106195 | doi = 10.1002/14651858.CD003208.pub2 | editor1-last = Gray | editor1-first = Orla }}</ref><ref name="pmid16900766">{{cite journal |vauthors=Gray OM, McDonnell GV, Forbes RB | title = A systematic review of oral methotrexate for multiple sclerosis | journal = Multiple Sclerosis | volume = 12 | issue = 4 | pages = 507–10 | date = Aug 2006 | pmid = 16900766 | doi = 10.1191/1352458506ms1299oa }}</ref> [[Cyclophosphamide]] is sometimes used to treat [[lupus nephritis]], a common symptom of [[systemic lupus erythematosus]].<ref name="pmid20107927">{{cite journal |vauthors=Ntali S, Bertsias G, Boumpas DT | title = Cyclophosphamide and lupus nephritis: when, how, for how long? | journal = Clinical Reviews in Allergy & Immunology | volume = 40 | issue = 3 | pages = 181–91 | date = Jun 2011 | pmid = 20107927 | doi = 10.1007/s12016-009-8196-0 }}</ref> [[Dexamethasone]] along with either [[bortezomib]] or [[melphalan]] is commonly used as a treatment for [[AL amyloidosis]]. Recently, bortezomid in combination with [[cyclophosphamide]] and dexamethasone has also shown promise as a treatment for AL amyloidosis. Other drugs used to treat [[myeloma]] such as [[lenalidomide]] have shown promise in treating AL amyloidosis.<ref>{{cite web|title=NCCN Guidelines: Systemic Light Chain Amyloidosis|url=http://williams.medicine.wisc.edu/amyloidosis.pdf|publisher=National Comprehensive Cancer Network}}</ref> |
|||
Chemotherapy drugs are also used in [[conditioning regimen]]s prior to bone marow transplant ([[hematopoietic stem cell transplant]]). Conditioning regimens are used to suppress the recipient's immune system in order to allow a transplant to engraft. Cyclophosphamide is a common cytotoxic drug used in this manner, and is often used in conjunction with [[total body irradiation]]. Chemotherapeutic drugs may be used at high doses to permanently remove the recipient's bone marrow cells (myeloablative conditioning) or at lower doses that will prevent permanent bone marrow loss (non-myeloablative and reduced intensity conditioning).<ref>{{cite journal |vauthors=Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, Apperley J, Slavin S, Pasquini M, Sandmaier BM, Barrett J, Blaise D, Lowski R, Horowitz M | title = Defining the intensity of conditioning regimens: working definitions | journal = Biology of Blood and Marrow Transplantation | volume = 15 | issue = 12 | pages = 1628–33 | date = Dec 2009 | pmid = 19896087 | pmc = 2861656 | doi = 10.1016/j.bbmt.2009.07.004 }}</ref> When used in non-cancer setting, the treatment is still called Chemotherapy, and is often done in the same treatment center as cancer patients. |
|||
== Occupational precautions == |
|||
Healthcare workers exposed to antineoplastic agents take precautions to keep their exposure to a minimum. There is a limitation in cytotoxics dissolution in Australia and the United States to 20 dissolutions per pharmacist/nurse,{{Citation needed|date=August 2013}} since pharmacists who prepare these drugs or nurses who may prepare or administer them are the two occupational groups with the highest potential exposure to antineoplastic agents. In addition, physicians and operating room personnel may also be exposed through the treatment of patients. Hospital staff, such as shipping and receiving personnel, custodial workers, laundry workers, and waste handlers, all have potential exposure to these drugs during the course of their work. The increased use of antineoplastic agents in veterinary oncology also puts these workers at risk for exposure to these drugs.<ref>{{cite web|url=http://www.cdc.gov/niosh/topics/antineoplastic/|title=NIOSH Occupational Exposure to Antineoplastic Agents |accessdate=10 October 2007 |publisher=United States National Institute for Occupational Safety and Health}}</ref><ref name=":0">{{Cite web|url = http://www.medscape.com/viewarticle/738076|title = Hazardous Drugs in Healthcare|date = March 7, 2011|accessdate = |website = NIOSH: Workplace Safety and Health|publisher = Medscape & NIOSH|last = Connor|first = Thomas H.}}</ref> Routes of entry into the worker's body are skin absorption, [[inhalation]], and [[ingestion]] via hand-to-mouth.<ref name=":0" /> The long-term effects of exposure include [[chromosomal abnormality|chromosomal abnormalities]] and [[infertility]].<ref name="isbn0-443-07101-2 2">Wood, p. 38.</ref> |
|||
== Available agents == |
|||
{{Main|List of antineoplastic agents}} |
|||
There is an extensive [[list of antineoplastic agents]]. Several classification schemes have been used to subdivide the medicines used for cancer into several different types.{{citation needed|date=November 2015}} |
|||
== History == |
|||
{{Main|History of cancer chemotherapy}} |
|||
[[File:Sidney Farber nci-vol-1926-300.jpg|thumb|150px|[[Sidney Farber]] is regarded as the father of modern chemotherapy.]] |
|||
The first use of [[small-molecule drug]]s to treat cancer was in the early 20th century, although the specific chemicals first used were not originally intended for that purpose. [[Mustard gas]] was used as a [[chemical warfare]] agent during [[World War I]] and was discovered to be a potent suppressor of [[hematopoiesis]] (blood production).<ref>{{cite journal |author=Krumbhaar EB |title=Role of the blood and the bone marrow in certain forms of gas poisoning |journal=JAMA |volume=72 |pages=39–41 |year=1919 |doi=10.1001/jama.1919.26110010018009f }}</ref> A similar family of compounds known as [[nitrogen mustards]] were studied further during [[World War II]] at the [[Yale School of Medicine]].<ref name="Fenn">{{cite journal |vauthors=Fenn JE, Udelsman R | title = First use of intravenous chemotherapy cancer treatment: rectifying the record | journal = Journal of the American College of Surgeons | volume = 212 | issue = 3 | pages = 413–417 | date = Mar 2011 | pmid = 21247779 | doi = 10.1016/j.jamcollsurg.2010.10.018 }}</ref> It was reasoned that an agent that damaged the rapidly growing white blood cells might have a similar effect on cancer.<ref name="Fenn" /> Therefore, in December 1942, several patients with advanced [[lymphomas]] (cancers of the lymphatic system and lymph nodes) were given the drug by vein, rather than by breathing the irritating gas.<ref name="Fenn" /> Their improvement, although temporary, was remarkable.<ref>{{cite journal |author1 =Goodman LS |author1-link=Louis S. Goodman |author2=Wintrobe MM |author3=Dameshek W |author4=Goodman MJ |author5=Gilman A |author5-link=Alfred Goodman, Sr. |author6=McLennan MT | title = Nitrogen mustard therapy. Use of methyl-bis(beta-chloroethyl)amine hydrochloride and tris(beta-chloroethyl)amine hydrochloride for Hodgkin's disease, lymphosarcoma, leukemia and certain allied and miscellaneous disorders | journal = JAMA| volume = 132 | issue = 3 |pages = 126–132 | year = 1946 | doi = 10.1001/jama.1946.02870380008004 }}</ref> Concurrently, during a military operation in World War II, following a German [[Air raid on Bari|air raid]] on the Italian harbour of Bari, several hundred people were accidentally exposed to mustard gas, which had been transported there by the [[Allies of World War II|Allied forces]] to prepare for possible retaliation in the event of German use of chemical warfare. The survivors were later found to have very low white blood cell counts.<ref>Faguet, p. 71</ref> After WWII was over and the reports declassified, the experiences converged and led researchers to look for other substances that might have similar effects against cancer. The first chemotherapy drug to be developed from this line of research was [[mustine]]. Since then, many other drugs have been developed to treat cancer, and drug development has exploded into a multibillion-dollar industry, although the principles and limitations of chemotherapy discovered by the early researchers still apply.<ref>{{cite journal | author = Joensuu H | title = Systemic chemotherapy for cancer: from weapon to treatment | journal = The Lancet. Oncology | volume = 9 | issue = 3 | page = 304 | date = Mar 2008 | pmid = 18308256 | doi = 10.1016/S1470-2045(08)70075-5 }}</ref> |
|||
=== The term ''chemotherapy'' === |
|||
The word ''chemotherapy'' without a modifier usually refers to cancer treatment, but its historical meaning was broader. The term was coined in the early 1900s by [[Paul Ehrlich]] as meaning any use of chemicals to treat any disease (''[[wikt:chemo-|chemo]]-'' + ''[[wikt:-therapy|-therapy]]''), such as the use of [[antibiotic]]s (''antibacterial chemotherapy'').<ref name="DeVita">{{cite journal |vauthors=DeVita VT, Chu E | title = A history of cancer chemotherapy | journal = Cancer Research | volume = 68 | issue = 21 | pages = 8643–53 | date = Nov 2008 | pmid = 18974103 | doi = 10.1158/0008-5472.CAN-07-6611 }}</ref> Ehrlich was not optimistic that effective chemotherapy drugs would be found for the treatment of cancer.<ref name="DeVita" /> The first modern chemotherapeutic agent was [[arsphenamine]], an arsenic compound discovered in 1907 and used to treat [[syphilis]].<ref name="pmid19868743">{{cite journal |vauthors=Nichols HJ, Walker JE | title = EXPERIMENTAL OBSERVATIONS ON THE PROPHYLAXIS AND TREATMENT OF SYPHILIS | journal = The Journal of Experimental Medicine | volume = 37 | issue = 4 | pages = 525–42 | date = Mar 1923 | pmid = 19868743 | pmc = 2128372 | doi = 10.1084/jem.37.4.525 }}</ref> This was later followed by [[Sulfonamide (medicine)|sulfonamides]] (sulfa drugs) and [[penicillin]]. In today's [[usage]], the [[word sense|sense]] "any treatment of disease with drugs" is often expressed with the word ''[[pharmacotherapy]]''. |
|||
== Sales == |
|||
Many of the most commonly used chemotherapy agents, such as cisplatin/[[carboplatin]], [[docetaxel]], [[gemcitabine]], [[paclitaxel]], [[vinorelbine]] and [[pemetrexed]] are [[Off-patent Drugs Bill|off-patent]], so they don't cost billions of dollars. The top 10 best-selling (in terms of revenue) cancer drugs of 2013:<ref>[http://www.fiercepharma.com/special-reports/top-10-best-selling-cancer-drugs-2013 Top 10 best-selling cancer drugs of 2013; May 29, 2014]</ref> |
|||
{| class="wikitable" |
|||
|- |
|||
! No. !! 2013 Global Sales !! [[International Nonproprietary Name|INN]] !! Trade names !! Companies !! Indications |
|||
|- |
|||
| 1 || $7.78 billion || [[Rituximab]] || Rituxan/MabThera || Roche, Pharmstandard || non-Hodgkin's lymphoma, CLL |
|||
|- |
|||
| 2 || $6.75 billion || [[Bevacizumab]] || Avastin || Roche || Colorectal, lung, ovarian and brain cancer |
|||
|- |
|||
| 3 || $6.56 billion || [[Trastuzumab]] || Herceptin || Roche || Breast, esophagus and stomach cancer |
|||
|- |
|||
| 4 || $4.69 billion || [[Imatinib]] || Gleevec || Novartis || Leukemia, GI cancer |
|||
|- |
|||
| 5 || $1.09 billion || [[Lenalidomide]] || Revlimid || Celgene, Pharmstandard || Multiple myeloma, mantle cell lymphoma |
|||
|- |
|||
| 6 || $2.7 billion || [[Pemetrexed]] || Alimta || Eli Lilly || Lung cancer |
|||
|- |
|||
| 7 || $2.6 billion || [[Bortezomib]] || Velcade || Johnson & Johnson, Takeda, Pharmstandard || Multiple myeloma |
|||
|- |
|||
| 8 || $1.87 billion || [[Cetuximab]] || Erbitux || Merck KGaA, Bristol-Myers Squibb || Colon and head and neck cancer |
|||
|- |
|||
| 9 || $1.73 billion || [[Leuprorelin]] || Lupron, Eligard || AbbVie and Takeda; Sanofi and Astellas Pharma || Prostate and ovarian cancer |
|||
|- |
|||
| 10 || $1.7 billion || [[Abiraterone]] || Zytiga || Johnson & Johnson || Prostate cancer |
|||
|} |
|||
== Research == |
|||
[[File:Mesoporous silica SEM.jpg|thumb|[[Scanning electron micrograph]] of [[mesoporous silica]]; a type of [[nanoparticle]] used in the delivery of chemotherapeutic drugs.]] |
|||
{{Main|Experimental cancer treatments}} |
|||
=== Targeted therapies === |
|||
Specially targeted delivery vehicles aim to increase effective levels of chemotherapy for tumor cells while reducing effective levels for other cells. This should result in an increased tumor kill and/or reduced toxicity.<ref name="pmid21501554">{{cite journal | author = Chidambaram M, Manavalan R, Kathiresan K | title = Nanotherapeutics to overcome conventional cancer chemotherapy limitations | journal = Journal of Pharmacy & Pharmaceutical Sciences | volume = 14 | issue = 1 | pages = 67–77 | year = 2011 | pmid = 21501554 | doi = }}</ref> |
|||
==== Antibody-drug conjugates ==== |
|||
[[Antibody-drug conjugate]]s (ADCs) comprise an [[antibody]], drug and a linker between them. The antibody will be targeted at a preferentially expressed protein in the tumour cells (known as a [[tumor antigen]]) or on cells that the tumor can utilise, such as blood vessel [[endothelial cells]]. They bind to the tumor antigen and are internalised, where the linker releases the drug into the cell. These specially targeted delivery vehicles vary in their stability, selectivity, and choice of target, but, in essence, they all aim to increase the maximum effective dose that can be delivered to the tumor cells.<ref name="pmid22003066">{{cite journal |vauthors=Teicher BA, Chari RV | title = Antibody conjugate therapeutics: challenges and potential | journal = Clinical Cancer Research | volume = 17 | issue = 20 | pages = 6389–97 | date = Oct 2011 | pmid = 22003066 | doi = 10.1158/1078-0432.CCR-11-1417 }}</ref> Reduced systemic toxicity means that they can also be used in sicker patients, and that they can carry new chemotherapeutic agents that would have been far too toxic to deliver via traditional systemic approaches.{{citation needed|date=August 2013}} |
|||
The first approved drug of this type was [[gemtuzumab ozogamicin]] (Mylotarg), released by [[Wyeth]] (now [[Pfizer]]). The drug was approved to treat [[acute myeloid leukemia]], but has now been withdrawn from the market because the drug did not meet efficacy targets in further clinical trials.<ref name="pmid11673694">{{cite journal |vauthors=Sievers EL, Linenberger M | title = Mylotarg: antibody-targeted chemotherapy comes of age | journal = Current Opinion in Oncology | volume = 13 | issue = 6 | pages = 522–7 | date = Nov 2001 | pmid = 11673694 | doi = 10.1097/00001622-200111000-00016 }}</ref><ref>{{cite web|last=FDA|title=Mylotarg (gemtuzumab ozogamicin): Market Withdrawal|url=http://www.fda.gov/safety/medwatch/safetyinformation/safetyalertsforhumanmedicalproducts/ucm216458.htm|accessdate=18 August 2013}}</ref> Two other drugs, [[trastuzumab emtansine]] and [[brentuximab vedotin]], are both in late clinical trials, and the latter has been granted accelerated approval for the treatment of [[refractory]] [[Hodgkin's lymphoma]] and systemic [[anaplastic large cell lymphoma]].<ref name="pmid22003066" /> |
|||
==== Nanoparticles ==== |
|||
[[Nanoparticles]] are 1-1000 [[nanometer]] (nm) sized particles that can promote tumor selectivity and aid in delivering low-[[solubility]] drugs. Nanoparticles can be targeted passively or actively. Passive targeting exploits the difference between tumor blood vessels and normal blood vessels. Blood vessels in tumors are "leaky" because they have gaps from 200-2000 nm, which allow nanoparticles to escape into the tumor. Active targeting uses biological molecules ([[antibodies]], [[protein]]s, [[DNA]] and [[receptor ligand]]s) to preferentially target the nanoparticles to the tumor cells. There are many types of nanoparticle delivery systems, such as [[mesoporous silica|silica]], [[polymer]]s, [[liposome]]s and [[magnetic particles]]. Nanoparticles made of magnetic material can also be used to concentrate agents at tumor sites using an externally applied magnetic field.<ref name="pmid21501554" /> They have emerged as a useful vehicle in [[magnetic drug delivery]] for poorly soluble agents such as [[paclitaxel]].<ref name="pmid19554862">{{cite journal |vauthors=Vines T, Faunce T | title = Assessing the safety and cost-effectiveness of early nanodrugs | journal = Journal of Law and Medicine | volume = 16 | issue = 5 | pages = 822–45 | date = May 2009 | pmid = 19554862 | doi = }}</ref> |
|||
=== Electrochemotherapy === |
|||
{{Main|Electrochemotherapy}} |
|||
Electrochemotherapy is the combined treatment in which injection of a chemotherapeutic drug is followed by application of high-voltage electric pulses locally to the tumor. The treatment enables the chemotherapeutic drugs, which otherwise cannot or hardly go through the membrane of cells (such as bleomycin and cisplatin), to enter the cancer cells. Hence, greater effectiveness of antitumor treatment is achieved. |
|||
Clinical electrochemotherapy has been successfully used for treatment of cutaneous and subcutaneous tumors irrespective of their histological origin.<ref>{{cite journal |vauthors=Heller R, Gilbert R, Jaroszeski MJ | title = Clinical applications of electrochemotherapy | journal = Advanced Drug Delivery Reviews | volume = 35 | issue = 1 | pages = 119–129 | date = Jan 1999 | pmid = 10837693 | doi = 10.1016/S0169-409X(98)00067-2 }}</ref><ref>{{cite journal |vauthors=Larkin JO, Collins CG, Aarons S, Tangney M, Whelan M, O'Reily S, Breathnach O, Soden DM, O'Sullivan GC | title = Electrochemotherapy: aspects of preclinical development and early clinical experience | journal = Annals of Surgery | volume = 245 | issue = 3 | pages = 469–479 | date = Mar 2007 | pmid = 17435555 | pmc = 1877027 | doi = 10.1097/01.sla.0000250419.36053.33 }}</ref><ref name="Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, Billard V, Geertsen PF, Larkin JO, Miklavcic D, Pavlovic I, Paulin-Kosir SM, Cemazar M, Morsli N, Soden DM, Rudolf Z, Robert C, O'Sullivan GC, Mir LM. 2006">{{cite journal |vauthors=Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, Billard V, Geertsen PF, Larkin JO, Miklavcic D, Pavlovic I, Paulin-Kosir SM, Cemazar M, Morsli N, Soden DM, Rudolf Z, Robert C, O'Sullivan GC, Mir LM |title=Electrochemotherapy – An easy, highly effective and safe treatment of cutaneous and subcutaneous metastases |pages=3–13 |journal=Eur J Cancer Suppl |volume=4 |issue=11 |year=2006|doi=10.1016/j.ejcsup.2006.08.002 }}</ref><ref>{{cite journal |vauthors=Möller MG, Salwa S, Soden DM, O'Sullivan GC | title = Electrochemotherapy as an adjunct or alternative to other treatments for unresectable or in-transit melanoma | journal = Expert Review of Anticancer Therapy | volume = 9 | issue = 11 | pages = 1611–1630 | date = Nov 2009 | pmid = 19895245 | doi = 10.1586/era.09.129 }}</ref><ref>{{cite journal |vauthors=Testori A, Tosti G, Martinoli C, Spadola G, Cataldo F, Verrecchia F, Baldini F, Mosconi M, Soteldo J, Tedeschi I, Passoni C, Pari C, Di Pietro A, Ferrucci PF | title = Electrochemotherapy for cutaneous and subcutaneous tumor lesions: a novel therapeutic approach | journal = Dermatologic Therapy | volume = 23 | issue = 6 | pages = 651–661 | year = 2010 | pmid = 21054709 | doi = 10.1111/j.1529-8019.2010.01370.x }}</ref><ref>{{cite journal | author = Hampton T | title = Electric pulses help with chemotherapy, may open new paths for other agents | journal = JAMA | volume = 305 | issue = 6 | pages = 549–551 | date = Feb 2011 | pmid = 21304073 | doi = 10.1001/jama.2011.92 }}</ref> The method has been reported as safe, simple and highly effective in all reports on clinical use of electrochemotherapy. According to the ESOPE project (European Standard Operating Procedures of Electrochemotherapy), the Standard Operating Procedures (SOP) for electrochemotherapy were prepared, based on the experience of the leading European cancer centres on electrochemotherapy.<ref name="Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, Billard V, Geertsen PF, Larkin JO, Miklavcic D, Pavlovic I, Paulin-Kosir SM, Cemazar M, Morsli N, Soden DM, Rudolf Z, Robert C, O'Sullivan GC, Mir LM. 2006" /><ref>{{cite journal |vauthors=Mir LM, Gehl J, Sersa G, Collins CG, Garbay JR, Billard V, Geertsen PF, Rudolf Z, O'Sullivan GC, Marty M |title=Standard operating procedures of the electrochemotherapy: Instructions for the use of bleomycin or cisplatin administered either systemically or locally and electric pulses delivered by the CliniporatorTM by means of invasive or non-invasive electrodes |journal=Eur J Cancer Suppl |volume=4 |issue=11 |pages=14–25 |year=2006 |doi=10.1016/j.ejcsup.2006.08.003 }}</ref> Recently, new electrochemotherapy modalities have been developed for treatment of internal tumors using surgical procedures, endoscopic routes or percutaneous approaches to gain access to the treatment area.<ref>{{cite journal |vauthors=Soden DM, Larkin JO, Collins CG, Tangney M, Aarons S, Piggott J, Morrissey A, Dunne C, O'Sullivan GC | title = Successful application of targeted electrochemotherapy using novel flexible electrodes and low dose bleomycin to solid tumours | journal = Cancer Letters | volume = 232 | issue = 2 | pages = 300–310 | date = Feb 2006 | pmid = 15964138 | doi = 10.1016/j.canlet.2005.03.057 }}</ref><ref>{{cite journal |vauthors=Miklavcic D, Snoj M, Zupanic A, Kos B, Cemazar M, Kropivnik M, Bracko M, Pecnik T, Gadzijev E, Sersa G | title = Towards treatment planning and treatment of deep-seated solid tumors by electrochemotherapy | journal = BioMedical Engineering OnLine | volume = 9 | issue = 1 | page = 10 | year = 2010 | pmid = 20178589 | pmc = 2843684 | doi = 10.1186/1475-925X-9-10 }}</ref> |
|||
=== Hyperthermia therapy === |
|||
[[Hyperthermia therapy]] is heat treatment for cancer that can be a powerful tool when used in combination with chemotherapy (thermochemotherapy) or radiation for the control of a variety of cancers. The heat can be applied locally to the tumor site, which will dilate blood vessels to the tumor, allowing more chemotherapeutic medication to enter the tumor. Additionally, the bi-lipid layer of the tumor cell membrane will become more porous, further allowing more of the chemotherapeutic medicine to enter the tumor cell. |
|||
Hyperthermia has also been shown to help prevent or reverse "chemo-resistance." Chemotherapy resistance sometimes develops over time as the tumors adapt and can overcome the toxicity of the chemo medication. "Overcoming chemoresistance has been extensively studied within the past, especially using CDDP-resistant cells. In regard to the potential benefit that drug-resistant cells can be recruited for effective therapy by combining chemotherapy with hyperthermia, it was important to show that chemoresistance against several anticancer drugs (e.g. mitomycin C, anthracyclines, BCNU, melphalan) including CDDP could be reversed at least partially by the addition of heat.<ref>{{cite journal|last=Issels|first=R.|title=Hyperthermia Combined with Chemotherapy – Biological Rationale, Clinical Application, and Treatment Results|journal=Onkologie|year=1999|volume=22|issue=5|pages=374–381|doi=10.1159/000026986}}</ref> |
|||
== Other animals == |
|||
Chemotherapy is used in veterinary medicine similar to how it is used in human medicine.<ref>{{cite journal | author = McKnight JA | title = Principles of chemotherapy | journal = Clinical Techniques in Small Animal Practice | volume = 18 | issue = 2 | pages = 67–72 | date = May 2003 | pmid = 12831063 | doi = 10.1053/svms.2003.36617 }}</ref> |
|||
== 參見 == |
== 參見 == |
||
2017年5月15日 (一) 12:31的版本
| ||||||||||||||||||||||||||||||||||||||||||||
化学疗法(英語:Chemotherapy),简称化疗(Chemo),是用特殊的药物来治疗疾病,為目前治疗肿瘤及某些自身免疫性疾病的主要手段之一,不過在治疗中,普遍會為患者帶來明显的恶心及呕吐等副作用,為患者带来不适感。化疗是指应用药物治疗癌症。这些可杀灭肿瘤细胞,有时称为细胞毒药物。许多化疗药物来源于自然,如:植物,其他是人工合成。目前已超过50种化疗药物,常用的有:表阿霉素、阿霉素、柔红霉素、丝裂霉素、氟脲嘧啶脱氧核苷酸等。这些药物经常以不同的强度联合应用。
化疗是一种全身性治疗手段对原发灶、转移灶和亚临床转移灶均有治疗作用,但是化疗治疗肿瘤在杀伤肿瘤细胞的同时,也可能将正常细胞和免疫(抵抗)细胞一同杀灭,所以化疗是一种“兩害相權取其輕”的治疗手段。
醫療機制
由于癌细胞的增殖比正常细胞快,抗癌药物的作用原理通常是阻断细胞分裂以抑制癌细胞生长,如一些药物可以抑制脱氧核醣核酸進行复制。化疗药物一般也同时杀死正常细胞,因而伤害了需要进行分裂以维持正常功能的健康组织,例如毛发基部细胞和肠粘膜细胞,使病人常伴有脱发及恶心呕吐等症状。一般情况下,化疗药物是毒性强的先打,时间短的先打,化疗药物换的时候一般用生理盐水冲洗,以减少药物过敏。例如长春瑞滨毒性较强,一般先打,打之前推地塞米松抗过敏,打的时候速度要快,使其尽快通过血管;多西他赛这种药物乃是紫杉醇的衍生物,这种药物毒性小,效果好,打的时候要给病人上心电监护,随时观察。不过在打格拉司琼的时候后面可以直接打化疗药物。如果发生化疗药物外渗,则立即停止注入,尽快吸收针头内的残留液体,拔出针头,局部冷敷湿敷,用硫酸镁溶液局部湿敷或用土豆片湿敷[來源請求],并抬高患肢24小时。
当然,也有用于非肿瘤治疗,如指抗生素(抗菌化疗)。从这个意义上讲,首先应用化疗剂的是保罗·埃利希,他于1909年用含砷化合物治疗梅毒。其他化学疗法的用法可以是用于治疗自身免疫性疾病,如多发性硬化症、类风湿性关节炎和抑制器官移植後的排斥反应等。
图片
-
西德尼·法伯,现代化疗之父
治療策略(Treatment strategies)
| Cancer type | Drugs | Acronym |
|---|---|---|
| Breast cancer | Cyclophosphamide, methotrexate, 5-fluorouracil | CMF |
| Doxorubicin, cyclophosphamide | AC | |
| Hodgkin's disease | Mustine, vincristine, procarbazine, prednisolone | MOPP |
| Doxorubicin, bleomycin, vinblastine, dacarbazine | ABVD | |
| Non-Hodgkin's lymphoma | Cyclophosphamide, doxorubicin, vincristine, prednisolone | CHOP |
| Germ cell tumor | Bleomycin, etoposide, cisplatin | BEP |
| Stomach cancer | Epirubicin, cisplatin, 5-fluorouracil | ECF |
| Epirubicin, cisplatin, capecitabine | ECX | |
| Bladder cancer | Methotrexate, vincristine, doxorubicin, cisplatin | MVAC |
| Lung cancer | Cyclophosphamide, doxorubicin, vincristine, | CAV |
| Colorectal cancer | 5-fluorouracil, folinic acid, oxaliplatin | FOLFOX |
There are a number of strategies in the administration of chemotherapeutic drugs used today. Chemotherapy may be given with a curative intent or it may aim to prolong life or to palliate symptoms.
- Induction chemotherapy is the first line treatment of cancer with a chemotherapeutic drug. This type of chemotherapy is used for curative intent.[2]
- Combined modality chemotherapy is the use of drugs with other cancer treatments, such as surgery, radiation therapy, and/or hyperthermia therapy.
- Consolidation chemotherapy is given after remission in order to prolong the overall disease-free time and improve overall survival. The drug that is administered is the same as the drug that achieved remission.[2]
- Intensification chemotherapy is identical to consolidation chemotherapy but a different drug than the induction chemotherapy is used.[2]
- Combination chemotherapy involves treating a patient with a number of different drugs simultaneously. The drugs differ in their mechanism and side-effects. The biggest advantage is minimising the chances of resistance developing to any one agent. Also, the drugs can often be used at lower doses, reducing toxicity.[2][3]
- Neoadjuvant chemotherapy is given prior to a local treatment such as surgery, and is designed to shrink the primary tumor.[2] It is also given to cancers with a high risk of micrometastatic disease.[4]
- Adjuvant chemotherapy is given after a local treatment (radiotherapy or surgery). It can be used when there is little evidence of cancer present, but there is risk of recurrence.[2] It is also useful in killing any cancerous cells that have spread to other parts of the body. These micrometastases can be treated with adjuvant chemotherapy and can reduce relapse rates caused by these disseminated cells.[5]
- Maintenance chemotherapy is a repeated low-dose treatment to prolong remission.[2]
- Salvage chemotherapy or palliative chemotherapy is given without curative intent, but simply to decrease tumor load and increase life expectancy. For these regimens, in general, a better toxicity profile is expected.[2]
All chemotherapy regimens require that the patient be capable of undergoing the treatment. Performance status is often used as a measure to determine whether a patient can receive chemotherapy, or whether dose reduction is required. Because only a fraction of the cells in a tumor die with each treatment (fractional kill), repeated doses must be administered to continue to reduce the size of the tumor.[6] Current chemotherapy regimens apply drug treatment in cycles, with the frequency and duration of treatments limited by toxicity to the patient.[7]
治療效果(Efficacy)
The efficacy of chemotherapy depends on the type of cancer and the stage. The overall effectiveness ranges from being curative for some cancers, such as some leukemias,[8][9] to being ineffective, such as in some brain tumors,[10] to being needless in others, like most non-melanoma skin cancers.[11]
劑量(Dosage)

Dosage of chemotherapy can be difficult: If the dose is too low, it will be ineffective against the tumor, whereas, at excessive doses, the toxicity (side-effects) will be intolerable to the patient.[1] The standard method of determining chemotherapy dosage is based on calculated body surface area (BSA). The BSA is usually calculated with a mathematical formula or a nomogram, using a patient's weight and height, rather than by direct measurement of body mass. This formula was originally derived in a 1916 study and attempted to translate medicinal doses established with laboratory animals to equivalent doses for humans.[12] The study only included 9 human subjects.[13] When chemotherapy was introduced in the 1950s, the BSA formula was adopted as the official standard for chemotherapy dosing for lack of a better option.[14][15]
Recently, the validity of this method in calculating uniform doses has been questioned. The reason for this is that the formula only takes into account the individual's weight and height. Drug absorption and clearance are influenced by multiple factors, including age, gender, metabolism, disease state, organ function, drug-to-drug interactions, genetics, and obesity, which has a major impact on the actual concentration of the drug in the patient's bloodstream.[14][16][17] As a result, there is high variability in the systemic chemotherapy drug concentration among patients dosed by BSA, and this variability has been demonstrated to be more than 10-fold for many drugs.[13][18] In other words, if two patients receive the same dose of a given drug based on BSA, the concentration of that drug in the bloodstream of one patient may be 10 times higher or lower compared to that of the other patient.[18] This variability is typical with many chemotherapy drugs dosed by BSA, and, as shown below, was demonstrated in a study of 14 common chemotherapy drugs.[13]
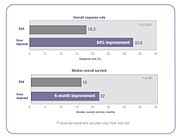
The result of this pharmacokinetic variability among patients is that many patients do not receive the right dose to achieve optimal treatment effectiveness with minimized toxic side effects. Some patients are overdosed while others are underdosed.[14][16][17][19][20][21][22] For example, in a randomized clinical trial, investigators found 85% of metastatic colorectal cancer patients treated with 5-fluorouracil (5-FU) did not receive the optimal therapeutic dose when dosed by the BSA standard—68% were underdosed and 17% were overdosed.[19]
There has been recent controversy over the use of BSA to calculate chemotherapy doses for obese patients.[23] Because of their higher BSA, clinicians often arbitrarily reduce the dose prescribed by the BSA formula for fear of overdosing.[23] In many cases, this can result in sub-optimal treatment.[23]
Several clinical studies have demonstrated that when chemotherapy dosing is individualized to achieve optimal systemic drug exposure, treatment outcomes are improved and toxic side effects are reduced.[19][21] In the 5-FU clinical study cited above, patients whose dose was adjusted to achieve a pre-determined target exposure realized an 84% improvement in treatment response rate and a six-month improvement in overall survival (OS) compared with those dosed by BSA.[19]
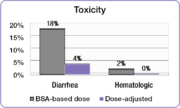
In the same study, investigators compared the incidence of common 5-FU-associated grade 3/4 toxicities between the dose-adjusted patients and the BSA-dosed patients.[19] The incidence of debilitating grades of diarrhea was reduced from 18% in the BSA-dosed group to 4% in the dose-adjusted group of patients and serious hematologic side effects were eliminated.[19] Because of the reduced toxicity, dose-adjusted patients were able to be treated for longer periods of time.[19] BSA-dosed patients were treated for a total of 680 months while dose-adjusted patients were treated for a total of 791 months.[19] Completing the course of treatment is an important factor in achieving better treatment outcomes.
Similar results were found in a study involving colorectal cancer patients treated with the popular FOLFOX regimen.[21] The incidence of serious diarrhea was reduced from 12% in the BSA-dosed group of patients to 1.7% in the dose-adjusted group, and the incidence of severe mucositis was reduced from 15% to 0.8%.[21]
The FOLFOX study also demonstrated an improvement in treatment outcomes.[21] Positive response increased from 46% in the BSA-dosed patients to 70% in the dose-adjusted group. Median progression free survival (PFS) and overall survival (OS) both improved by six months in the dose adjusted group.[21]
One approach that can help clinicians individualize chemotherapy dosing is to measure the drug levels in blood plasma over time and adjust dose according to a formula or algorithm to achieve optimal exposure. With an established target exposure for optimized treatment effectiveness with minimized toxicities, dosing can be personalized to achieve target exposure and optimal results for each patient. Such an algorithm was used in the clinical trials cited above and resulted in significantly improved treatment outcomes.
Oncologists are already individualizing dosing of some cancer drugs based on exposure. Carboplatin[24] and busulfan[25][26] dosing rely upon results from blood tests to calculate the optimal dose for each patient. Simple blood tests are also available for dose optimization of methotrexate,[27] 5-FU, paclitaxel, and docetaxel.[28][29]
種類(Types)

烷基化劑(Alkylating agents)
Alkylating agents are the oldest group of chemotherapeutics in use today. Originally derived from mustard gas used in World War I, there are now many types of alkylating agents in use.[1] They are so named because of their ability to alkylate many molecules, including proteins, RNA and DNA. This ability to bind covalently to DNA via their alkyl group is the primary cause for their anti-cancer effects.[31] DNA is made of two strands and the molecules may either bind twice to one strand of DNA (intrastrand crosslink) or may bind once to both strands (interstrand crosslink). If the cell tries to replicate crosslinked DNA during cell division, or tries to repair it, the DNA strands can break. This leads to a form of programmed cell death called apoptosis.[30][32] Alkylating agents will work at any point in the cell cycle and thus are known as cell cycle-independent drugs. For this reason the effect on the cell is dose dependent; the fraction of cells that die is directly proportional to the dose of drug.[33]
The subtypes of alkylating agents are the nitrogen mustards, nitrosoureas, tetrazines, aziridines,[34] cisplatins and derivatives, and non-classical alkylating agents. Nitrogen mustards include mechlorethamine, cyclophosphamide, melphalan, chlorambucil, ifosfamide and busulfan. Nitrosoureas include N-Nitroso-N-methylurea (MNU), carmustine (BCNU), lomustine (CCNU) and semustine (MeCCNU), fotemustine and streptozotocin. Tetrazines include dacarbazine, mitozolomide and temozolomide. Aziridines include thiotepa, mytomycin and diaziquone (AZQ). Cisplatin and derivatives include cisplatin, carboplatin and oxaliplatin.[31][32] They impair cell function by forming covalent bonds with the amino, carboxyl, sulfhydryl, and phosphate groups in biologically important molecules.[35] Non-classical alkylating agents include procarbazine and hexamethylmelamine.[31][32]
Antimetabolites

Anti-metabolites are a group of molecules that impede DNA and RNA synthesis. Many of them have a similar structure to the building blocks of DNA and RNA. The building blocks are nucleotides; a molecule comprising a nucleobase, a sugar and a phosphate group. The nucleobases are divided into purines (guanine and adenine) and pyrimidines (cytosine, thymine and uracil). Anti-metabolites resemble either nucleobases or nucleosides (a nucleotide without the phosphate group), but have altered chemical groups.[36] These drugs exert their effect by either blocking the enzymes required for DNA synthesis or becoming incorporated into DNA or RNA. By inhibiting the enzymes involved in DNA synthesis, they prevent mitosis because the DNA cannot duplicate itself. Also, after misincorporation of the molecules into DNA, DNA damage can occur and programmed cell death (apoptosis) is induced. Unlike alkylating agents, anti-metabolites are cell cycle dependent. This means that they only work during a specific part of the cell cycle, in this case S-phase (the DNA synthesis phase). For this reason, at a certain dose, the effect plateaus and proportionally no more cell death occurs with increased doses. Subtypes of the anti-metabolites are the anti-folates, fluoropyrimidines, deoxynucleoside analogues and thiopurines.[31][36]
The anti-folates include methotrexate and pemetrexed. Methotrexate inhibits dihydrofolate reductase (DHFR), an enzyme that regenerates tetrahydrofolate from dihydrofolate. When the enzyme is inhibited by methotrexate, the cellular levels of folate coenzymes diminish. These are required for thymidylate and purine production, which are both essential for DNA synthesis and cell division.[2][37] Pemetrexed is another anti-metabolite that affects purine and pyrimidine production, and therefore also inhibits DNA synthesis. It primarily inhibits the enzyme thymidylate synthase, but also has effects on DHFR, aminoimidazole carboxamide ribonucleotide formyltransferase and glycinamide ribonucleotide formyltransferase.[38] The fluoropyrimidines include fluorouracil and capecitabine. Fluorouracil is a nucleobase analogue that is metabolised in cells to form at least two active products; 5-fluourouridine monophosphate (FUMP) and 5-fluoro-2'-deoxyuridine 5'-phosphate (fdUMP). FUMP becomes incorporated into RNA and fdUMP inhibits the enzyme thymidylate synthase; both of which lead to cell death.[37] Capecitabine is a prodrug of 5-fluorouracil that is broken down in cells to produce the active drug.[39] The deoxynucleoside analogues include cytarabine, gemcitabine, decitabine, azacitidine, fludarabine, nelarabine, cladribine, clofarabine, and pentostatin. The thiopurines include thioguanine and mercaptopurine.[31][36]
Anti-microtubule agents

Anti-microtubule agents are plant-derived chemicals that block cell division by preventing microtubule function. Microtubules are an important cellular structure composed of two proteins; α-tubulin and β-tubulin. They are hollow rod shaped structures that are required for cell division, among other cellular functions.[40] Microtubules are dynamic structures, which means that they are permanently in a state of assembly and disassembly. Vinca alkaloids and taxanes are the two main groups of anti-microtubule agents, and although both of these groups of drugs cause microtubule dysfunction, their mechanisms of action are completely opposite. The vinca alkaloids prevent the formation of the microtubules, whereas the taxanes prevent the microtubule disassembly. By doing so, they prevent the cancer cells from completing mitosis. Following this, cell cycle arrest occurs, which induces programmed cell death (apoptosis).[31][41] Also, these drugs can affect blood vessel growth; an essential process that tumours utilise in order to grow and metastasise.[41]
Vinca alkaloids are derived from the Madagascar periwinkle, Catharanthus roseus (formerly known as Vinca rosea). They bind to specific sites on tubulin, inhibiting the assembly of tubulin into microtubules. The original vinca alkaloids are completely natural chemicals that include vincristine and vinblastine. Following the success of these drugs, semi-synthetic vinca alkaloids were produced: vinorelbine, vindesine, and vinflunine.[41] These drugs are cell cycle-specific. They bind to the tubulin molecules in S-phase and prevent proper microtubule formation required for M-phase.[33]
Taxanes are natural and semi-synthetic drugs. The first drug of their class, paclitaxel, was originally extracted from the Pacific Yew tree, Taxus brevifolia. Now this drug and another in this class, docetaxel, are produced semi-synthetically from a chemical found in the bark of another Yew tree; Taxus baccata. These drugs promote microtubule stability, preventing their disassembly. Paclitaxel prevents the cell cycle at the boundary of G2-M, whereas docetaxel exerts its effect during S-phase. Taxanes present difficulties in formulation as medicines because they are poorly soluble in water.[41]
Podophyllotoxin is an antineoplastic lignan obtained primarily from the American Mayapple (Podophyllum peltatum) and Himalayan Mayapple (Podophyllum hexandrum or Podophyllum emodi). It has anti-microtubule activity, and its mechanism is similar to that of vinca alkaloids in that they bind to tubulin, inhibiting microtubule formation. Podophyllotoxin is used to produce two other drugs with different mechanisms of action: etoposide and teniposide.[42][43]
Topoisomerase inhibitors

Topoisomerase inhibitors are drugs that affect the activity of two enzymes: topoisomerase I and topoisomerase II. When the DNA double-strand helix is unwound, during DNA replication or transcription, for example, the adjacent unopened DNA winds tighter (supercoils), like opening the middle of a twisted rope. The stress caused by this effect is in part aided by the topoisomerase enzymes. They produce single- or double-strand breaks into DNA, reducing the tension in the DNA strand. This allows the normal unwinding of DNA to occur during replication or transcription. Inhibition of topoisomerase I or II interferes with both of these processes.[44][45]
Two topoisomerase I inhibitors, irinotecan and topotecan, are semi-synthetically derived from camptothecin, which is obtained from the Chinese ornamental tree Camptotheca acuminata.[33] Drugs that target topoisomerase II can be divided into two groups. The topoisomerase II poisons cause increased levels enzymes bound to DNA. This prevents DNA replication and transcription, causes DNA strand breaks, and leads to programmed cell death (apoptosis). These agents include etoposide, doxorubicin, mitoxantrone and teniposide. The second group, catalytic inhibitors, are drugs that block the activity of topoisomerase II, and therefore prevent DNA synthesis and translation because the DNA cannot unwind properly. This group includes novobiocin, merbarone, and aclarubicin, which also have other significant mechanisms of action.[46]
Cytotoxic antibiotics
The cytotoxic antibiotics are a varied group of drugs that have various mechanisms of action. The common theme that they share in their chemotherapy indication is that they interrupt cell division. The most important subgroup is the anthracyclines and the bleomycins; other prominent examples include mitomycin C, mitoxantrone, and actinomycin.[47]
Among the anthracyclines, doxorubicin and daunorubicin were the first, and were obtained from the bacterium Streptomyces peucetius.[48] Derivatives of these compounds include epirubicin and idarubicin. Other clinically used drugs in the anthracyline group are pirarubicin, aclarubicin, and mitoxantrone. The mechanisms of anthracyclines include DNA intercalation (molecules insert between the two strands of DNA), generation of highly reactive free radicals that damage intercellular molecules and topoisomerase inhibition.[49]
Actinomycin is a complex molecule that intercalates DNA and prevents RNA synthesis.[50]
Bleomycin, a glycopeptide isolated from Streptomyces verticillus, also intercalates DNA, but produces free radicals that damage DNA. This occurs when bleomycin binds to a metal ion, becomes chemically reduced and reacts with oxygen.[51][52]
Mitomycin is a cytotoxic antibiotic with the ability to alkylate DNA.[53]
Delivery

Most chemotherapy is delivered intravenously, although a number of agents can be administered orally (e.g., melphalan, busulfan, capecitabine).
There are many intravenous methods of drug delivery, known as vascular access devices. These include the winged infusion device, peripheral cannula, midline catheter, peripherally inserted central catheter (PICC), central venous catheter and implantable port. The devices have different applications regarding duration of chemotherapy treatment, method of delivery and types of chemotherapeutic agent.[54]
Depending on the patient, the cancer, the stage of cancer, the type of chemotherapy, and the dosage, intravenous chemotherapy may be given on either an inpatient or an outpatient basis. For continuous, frequent or prolonged intravenous chemotherapy administration, various systems may be surgically inserted into the vasculature to maintain access.[55] Commonly used systems are the Hickman line, the Port-a-Cath, and the PICC line. These have a lower infection risk, are much less prone to phlebitis or extravasation, and eliminate the need for repeated insertion of peripheral cannulae.[來源請求]
Isolated limb perfusion (often used in melanoma),[56] or isolated infusion of chemotherapy into the liver[57] or the lung have been used to treat some tumors. The main purpose of these approaches is to deliver a very high dose of chemotherapy to tumor sites without causing overwhelming systemic damage.[58] These approaches can help control solitary or limited metastases, but they are by definition not systemic, and, therefore, do not treat distributed metastases or micrometastases.
Topical chemotherapies, such as 5-fluorouracil, are used to treat some cases of non-melanoma skin cancer.[59]
If the cancer has central nervous system involvement, or with meningeal disease, intrathecal chemotherapy may be administered.[1]
Adverse effects
Chemotherapeutic techniques have a range of side-effects that depend on the type of medications used. The most common medications affect mainly the fast-dividing cells of the body, such as blood cells and the cells lining the mouth, stomach, and intestines. Chemotherapy-related toxicities can occur acutely after administration, within hours or days, or chronically, from weeks to years.[60]
Immunosuppression and myelosuppression
Virtually all chemotherapeutic regimens can cause depression of the immune system, often by paralysing the bone marrow and leading to a decrease of white blood cells, red blood cells, and platelets. Anemia and thrombocytopenia, when they occur, are improved with blood transfusion. Neutropenia (a decrease of the neutrophil granulocyte count below 0.5 x 109/litre) can be improved with synthetic G-CSF (granulocyte-colony-stimulating factor, e.g., filgrastim, lenograstim).
In very severe myelosuppression, which occurs in some regimens, almost all the bone marrow stem cells (cells that produce white and red blood cells) are destroyed, meaning allogenic or autologous bone marrow cell transplants are necessary. (In autologous BMTs, cells are removed from the patient before the treatment, multiplied and then re-injected afterward; in allogenic BMTs, the source is a donor.) However, some patients still develop diseases because of this interference with bone marrow.[來源請求]
Although patients are encouraged to wash their hands, avoid sick people, and take other infection-reducing steps, about 85% of infections are due to naturally occurring microorganisms in the patient's own gastrointestinal tract (including oral cavity) and skin.[61] This may manifest as systemic infections, such as sepsis, or as localized outbreaks, such as Herpes simplex, shingles, or other members of the Herpesviridea.[62] The risk of illness and death can be reduced by taking common antibiotics such as quinolone or trimethoprim/sulfamethoxazole before any fever or sign of infection appears.[63] For every five people who are immunosuppressed following chemotherapy who take an antibiotic, one fever can be prevented; for every 34 who take an antibiotic, one death can be prevented.[63] Sometimes, chemotherapy treatments are postponed because the immune system is suppressed to a critically low level.
In Japan, the government has approved the use of some medicinal mushrooms like Trametes versicolor, to counteract depression of the immune system in patients undergoing chemotherapy.[64]
Neutropenic enterocolitis
Due to immune system suppression, neutropenic enterocolitis (typhlitis) is a "life-threatening gastrointestinal complication of chemotherapy."[65] Typhlitis is an intestinal infection which may manifest itself through symptoms including nausea, vomiting, diarrhea, a distended abdomen, fever, chills, or abdominal pain and tenderness.
Typhlitis is a medical emergency. It has a very poor prognosis and is often fatal unless promptly recognized and aggressively treated.[66] Successful treatment hinges on early diagnosis provided by a high index of suspicion and the use of CT scanning, nonoperative treatment for uncomplicated cases, and sometimes elective right hemicolectomy to prevent recurrence.[66]
Gastrointestinal distress
Nausea, vomiting, anorexia, diarrhoea, abdominal cramps, and constipation are common side-effects of chemotherapeutic medications that kill fast-dividing cells.[67] Malnutrition and dehydration can result when the patient does not eat or drink enough, or when the patient vomits frequently, because of gastrointestinal damage. This can result in rapid weight loss, or occasionally in weight gain, if the patient eats too much in an effort to allay nausea or heartburn. Weight gain can also be caused by some steroid medications. These side-effects can frequently be reduced or eliminated with antiemetic drugs. Self-care measures, such as eating frequent small meals and drinking clear liquids or ginger tea, are often recommended. In general, this is a temporary effect, and frequently resolves within a week of finishing treatment. However, a high index of suspicion is appropriate, since diarrhea and bloating are also symptoms of typhlitis, a very serious and potentially life-threatening medical emergency that requires immediate treatment.
Anemia
Anemia in cancer patients can be a combined outcome caused by myelosuppressive chemotherapy, and possible cancer-related causes such as bleeding, blood cell destruction (hemolysis), hereditary disease, kidney dysfunction, nutritional deficiencies and/or anemia of chronic disease. Treatments to mitigate anemia include hormones to boost blood production (erythropoietin), iron supplements, and blood transfusions.[68][69][70] Myelosuppressive therapy can cause a tendency to bleed easily, leading to anemia. Medications that kill rapidly dividing cells or blood cells can reduce the number of platelets in the blood, which can result in bruises and bleeding. Extremely low platelet counts may be temporarily boosted through platelet transfusions and new drugs to increase platelet counts during chemotherapy are being developed.[71][72] Sometimes, chemotherapy treatments are postponed to allow platelet counts to recover.
Fatigue
Fatigue may be a consequence of the cancer or its treatment, and can last for months to years after treatment. One physiological cause of fatigue is anemia, which can be caused by chemotherapy, surgery, radiotherapy, primary and metastatic disease and/or nutritional depletion.[73][74] Anaerobic exercise has been found to be beneficial in reducing fatigue in people with solid tumours.[75]
Nausea and vomiting
Nausea and vomiting are two of the most feared cancer treatment-related side-effects for cancer patients and their families. In 1983, Coates et al. found that patients receiving chemotherapy ranked nausea and vomiting as the first and second most severe side-effects, respectively. Up to 20% of patients receiving highly emetogenic agents in this era postponed, or even refused, potentially curative treatments.[76] Chemotherapy-induced nausea and vomiting (CINV) are common with many treatments and some forms of cancer. Since the 1990s, several novel classes of antiemetics have been developed and commercialized, becoming a nearly universal standard in chemotherapy regimens, and helping to successfully manage these symptoms in a large portion of patients. Effective mediation of these unpleasant and sometimes-crippling symptoms results in increased quality of life for the patient and more efficient treatment cycles, due to less stoppage of treatment due to better tolerance by the patient, and due to better overall health of the patient.
Hair loss
Hair loss (Alopecia) can be caused by chemotherapy that kills rapidly dividing cells; other medications may cause hair to thin. These are most often temporary effects: hair usually starts to regrow a few weeks after the last treatment, and can sometimes change colour, texture, thickness and style. Sometimes hair has a tendency to curl after regrowth, resulting in "chemo curls." Severe hair loss occurs most often with drugs such as doxorubicin, daunorubicin, paclitaxel, docetaxel, cyclophosphamide, ifosfamide and etoposide. Permanent thinning or hair loss can result from some standard chemotherapy regimens.
Chemotherapy induced hair loss occurs by a non-androgenic mechanism, and can manifest as alopecia totalis, telogen effluvium, or less often alopecia areata.[77] It is usually associated with systemic treatment due to the high mitotic rate of hair follicles, and more reversible than androgenic hair loss,[78][79] although permanent cases can occur.[80] Chemotherapy induces hair loss in women more often than men.[81]
Scalp cooling offers a means of preventing both permanent and temporary hair loss; however, concerns about this method have been raised.[82][83]
Secondary neoplasm
Development of secondary neoplasia after successful chemotherapy and/or radiotherapy treatment can occur. The most common secondary neoplasm is secondary acute myeloid leukemia, which develops primarily after treatment with alkylating agents or topoisomerase inhibitors.[84] Survivors of childhood cancer are more than 13 times as likely to get a secondary neoplasm during the 30 years after treatment than the general population.[85] Not all of this increase can be attributed to chemotherapy.
Infertility
Some types of chemotherapy are gonadotoxic and may cause infertility.[86] Chemotherapies with high risk include procarbazine and other alkylating drugs such as cyclophosphamide, ifosfamide, busulfan, melphalan, chlorambucil, and chlormethine.[86] Drugs with medium risk include doxorubicin and platinum analogs such as cisplatin and carboplatin.[86] On the other hand, therapies with low risk of gonadotoxicity include plant derivatives such as vincristine and vinblastine, antibiotics such as bleomycin and dactinomycin, and antimetabolites such as methotrexate, mercaptopurine, and 5-fluorouracil.[86]
Female infertility by chemotherapy appears to be secondary to premature ovarian failure by loss of primordial follicles.[87] This loss is not necessarily a direct effect of the chemotherapeutic agents, but could be due to an increased rate of growth initiation to replace damaged developing follicles.[87]
Patients may choose between several methods of fertility preservation prior to chemotherapy, including cryopreservation of semen, ovarian tissue, oocytes, or embryos.[88] As more than half of cancer patients are elderly, this adverse effect is only relevant for a minority of patients. A study in France between 1999 and 2011 came to the result that embryo freezing before administration of gonadotoxic agents to females caused a delay of treatment in 34% of cases, and a live birth in 27% of surviving cases who wanted to become pregnant, with the follow-up time varying between 1 and 13 years.[89]
Potential protective or attenuating agents include GnRH analogs, where several studies have shown a protective effect in vivo in humans, but some studies show no such effect. Sphingosine-1-phosphate (S1P) has shown similar effect, but its mechanism of inhibiting the sphingomyelin apoptotic pathway may also interfere with the apoptosis action of chemotherapy drugs.[90]
In chemotherapy as a conditioning regimen in hematopoietic stem cell transplantation, a study of patients conditioned with cyclophosphamide alone for severe aplastic anemia came to the result that ovarian recovery occurred in all women younger than 26 years at time of transplantation, but only in five of 16 women older than 26 years.[91]
Teratogenicity
Chemotherapy is teratogenic during pregnancy, especially during the first trimester, to the extent that abortion usually is recommended if pregnancy in this period is found during chemotherapy.[92] Second- and third-trimester exposure does not usually increase the teratogenic risk and adverse effects on cognitive development, but it may increase the risk of various complications of pregnancy and fetal myelosuppression.[92]
In males previously having undergone chemotherapy or radiotherapy, there appears to be no increase in genetic defects or congenital malformations in their children conceived after therapy.[92] The use of assisted reproductive technologies and micromanipulation techniques might increase this risk.[92] In females previously having undergone chemotherapy, miscarriage and congenital malformations are not increased in subsequent conceptions.[92] However, when in vitro fertilization and embryo cryopreservationis practised between or shortly after treatment, possible genetic risks to the growing oocytes exist, and hence it has been recommended that the babies be screened.[92]
Peripheral neuropathy
Between 30 and 40 percent of patients undergoing chemotherapy experience chemotherapy-induced peripheral neuropathy (CIPN), a progressive, enduring, and often irreversible condition, causing pain, tingling, numbness and sensitivity to cold, beginning in the hands and feet and sometimes progressing to the arms and legs.[93] Chemotherapy drugs associated with CIPN include thalidomide, epothilones, vinca alkaloids, taxanes, proteasome inhibitors, and the platinum-based drugs.[93][94][95] Whether CIPN arises, and to what degree, is determined by the choice of drug, duration of use, the total amount consumed and whether the patient already has peripheral neuropathy. Though the symptoms are mainly sensory, in some cases motor nerves and the autonomic nervous system are affected.[96] CIPN often follows the first chemotherapy dose and increases in severity as treatment continues, but this progression usually levels off at completion of treatment. The platinum-based drugs are the exception; with these drugs, sensation may continue to deteriorate for several months after the end of treatment.[97] Some CIPN appears to be irreversible.[97] Pain can often be managed with drug or other treatment but the numbness is usually resistant to treatment.[98]
Cognitive impairment
Some patients report fatigue or non-specific neurocognitive problems, such as an inability to concentrate; this is sometimes called post-chemotherapy cognitive impairment, referred to as "chemo brain" by patients' groups.[99]
Tumor lysis syndrome
In particularly large tumors and cancers with high white cell counts, such as lymphomas, teratomas, and some leukemias, some patients develop tumor lysis syndrome. The rapid breakdown of cancer cells causes the release of chemicals from the inside of the cells. Following this, high levels of uric acid, potassium and phosphate are found in the blood. High levels of phosphate induce secondary hypoparathyroidism, resulting in low levels of calcium in the blood. This causes kidney damage and the high levels of potassium can cause cardiac arrhythmia. Although prophylaxis is available and is often initiated in patients with large tumors, this is a dangerous side-effect that can lead to death if left untreated.[100]
Organ damage
Cardiotoxicity (heart damage) is especially prominent with the use of anthracycline drugs (doxorubicin, epirubicin, idarubicin, and liposomal doxorubicin). The cause of this is most likely due to the production of free radicals in the cell and subsequent DNA damage. Other chemotherapeutic agents that cause cardiotoxicity, but at a lower incidence, are cyclophosphamide, docetaxel and clofarabine.[101]
Hepatotoxicity (liver damage) can be caused by many cytotoxic drugs. The susceptibility of an individual to liver damage can be altered by other factors such as the cancer itself, viral hepatitis, immunosuppression and nutritional deficiency. The liver damage can consist of damage to liver cells, hepatic sinusoidal syndrome (obstruction of the veins in the liver), cholestasis (where bile does not flow from the liver to the intestine) and liver fibrosis.[102][103]
Nephrotoxicity (kidney damage) can be caused by tumor lysis syndrome and also due direct effects of drug clearance by the kidneys. Different drugs will affect different parts of the kidney and the toxicity may be asymptomatic (only seen on blood or urine tests) or may cause acute renal failure.[104][105]
Ototoxicity (damage to the inner ear) is a common side effect of platinum based drugs that can produce symptoms such as dizziness and vertigo.[106][107]
Other side-effects
Less common side-effects include red skin (erythema), dry skin, damaged fingernails, a dry mouth (xerostomia), water retention, and sexual impotence. Some medications can trigger allergic or pseudoallergic reactions.
Specific chemotherapeutic agents are associated with organ-specific toxicities, including cardiovascular disease (e.g., doxorubicin), interstitial lung disease (e.g., bleomycin) and occasionally secondary neoplasm (e.g., MOPP therapy for Hodgkin's disease).
Limitations
Chemotherapy does not always work, and even when it is useful, it may not completely destroy the cancer. Patients frequently fail to understand its limitations. In one study of patients who had been newly diagnosed with incurable, stage 4 cancer, more than two-thirds of patients with lung cancer and more than four-fifths of patients with colorectal cancer still believed that chemotherapy was likely to cure their cancer.[108]
The blood–brain barrier poses a difficult obstacle to pass to deliver chemotherapy to the brain. This is because the brain has an extensive system in place to protect it from harmful chemicals. Drug transporters can pump out drugs from the brain and brain's blood vessel cells into the cerebrospinal fluid and blood circulation. These transporters pump out most chemotherapy drugs, which reduces their efficacy for treatment of brain tumors. Only small lipophilic alkylating agents such as lomustine or temozolomide are able to cross this blood–brain barrier.[109][110][111]
Blood vessels in tumors are very different from those seen in normal tissues. As a tumor grows, tumor cells furthest away from the blood vessels become low in oxygen (hypoxic). To counteract this they then signal for new blood vessels to grow. The newly formed tumor vasculature is poorly formed and does not deliver an adequate blood supply to all areas of the tumor. This leads to issues with drug delivery because many drugs will be delivered to the tumor by the circulatory system.[112]
Resistance
Resistance is a major cause of treatment failure in chemotherapeutic drugs. There are a few possible causes of resistance in cancer, one of which is the presence of small pumps on the surface of cancer cells that actively move chemotherapy from inside the cell to the outside. Cancer cells produce high amounts of these pumps, known as p-glycoprotein, in order to protect themselves from chemotherapeutics. Research on p-glycoprotein and other such chemotherapy efflux pumps is currently ongoing. Medications to inhibit the function of p-glycoprotein are undergoing investigation, but due to toxicities and interactions with anti-cancer drugs their development has been difficult.[113][114] Another mechanism of resistance is gene amplification, a process in which multiple copies of a gene are produced by cancer cells. This overcomes the effect of drugs that reduce the expression of genes involved in replication. With more copies of the gene, the drug can not prevent all expression of the gene and therefore the cell can restore its proliferative ability. Cancer cells can also cause defects in the cellular pathways of apoptosis (programmed cell death). As most chemotherapy drugs kill cancer cells in this manner, defective apoptosis allows survival of these cells, making them resistant. Many chemotherapy drugs also cause DNA damage, which can be repaired by enzymes in the cell that carry out DNA repair. Upregulation of these genes can overcome the DNA damage and prevent the induction of apoptosis. Mutations in genes that produce drug target proteins, such as tubulin, can occur which prevent the drugs from binding to the protein, leading to resistance to these types of drugs.[115] Drugs used in chemotherapy can induce cell stress, which can kill a cancer cell; however, under certain conditions, cells stress can induce changes in gene expression that enables resistance to several types of drugs.[116]
Cytotoxics and targeted therapies
Targeted therapies are a relatively new class of cancer drugs that can overcome many of the issues seen with the use of cytotoxics. They are divided into two groups: small molecule and antibodies. The massive toxicity seen with the use of cytotoxics is due to the lack of cell specificity of the drugs. They will kill any rapidly dividing cell, tumor or normal. Targeted therapies are designed to affect cellular proteins or processes that are utilised by the cancer cells. This allows a high dose to cancer tissues with a relatively low dose to other tissues. As different proteins are utilised by different cancer types, the targeted therapy drugs are used on a cancer type specific, or even on a patient specific basis. Although the side effects are often less severe than that seen of cytotoxic chemotherapeutics, life-threatening effects can occur. Initially, the targeted therapeutics were supposed to be solely selective for one protein. Now it is clear that there is often a range of protein targets that the drug can bind. An example target for targeted therapy is the protein produced by the Philadelphia chromosome, a genetic lesion found commonly in chronic myelomonocytic leukemia. This fusion protein has enzyme activity that can be inhibited by imatinib, a small molecule drug.[117][118][119][120]
Mechanism of action

Cancer is the uncontrolled growth of cells coupled with malignant behaviour: invasion and metastasis (among other features).[121] It is caused by the interaction between genetic susceptibility and environmental factors.[122][123] These factors lead to accumulations of genetic mutations in oncogenes (genes that control the growth rate of cells) and tumor suppressor genes (genes that help to prevent cancer), which gives cancer cells their malignant characteristics, such as uncontrolled growth.[124]
In the broad sense, most chemotherapeutic drugs work by impairing mitosis (cell division), effectively targeting fast-dividing cells. As these drugs cause damage to cells, they are termed cytotoxic. They prevent mitosis by various mechanisms including damaging DNA and inhibition of the cellular machinery involved in cell division.[33][125] One theory as to why these drugs kill cancer cells is that they induce a programmed form of cell death known as apoptosis.[126]
As chemotherapy affects cell division, tumors with high growth rates (such as acute myelogenous leukemia and the aggressive lymphomas, including Hodgkin's disease) are more sensitive to chemotherapy, as a larger proportion of the targeted cells are undergoing cell division at any time. Malignancies with slower growth rates, such as indolent lymphomas, tend to respond to chemotherapy much more modestly.[1] Heterogeneic tumours may also display varying sensitivities to chemotherapy agents, depending on the subclonal populations within the tumor.
Other uses
Some chemotherapy drugs are used in diseases other than cancer, such as in autoimmune disorders,[127] and noncancerous plasma cell dyscrasia. In some cases they are often used at lower doses, which means that the side effects are minimized,[127] while in other cases doses similar to ones used to treat cancer are used. Methotrexate is used in the treatment of rheumatoid arthritis (RA),[128] psoriasis,[129] ankylosing spondylitis[130] and multiple sclerosis.[131][132] The anti-inflammatory response seen in RA is thought to be due to increases in adenosine, which causes immunosuppression; effects on immuno-regulatory cyclooxygenase-2 enzyme pathways; reduction in pro-inflammatory cytokines; and anti-proliferative properties.[128] Although methotrexate is used to treat both multiple sclerosis and ankylosing spondylitis, its efficacy in these diseases is still uncertain.[130][131][132] Cyclophosphamide is sometimes used to treat lupus nephritis, a common symptom of systemic lupus erythematosus.[133] Dexamethasone along with either bortezomib or melphalan is commonly used as a treatment for AL amyloidosis. Recently, bortezomid in combination with cyclophosphamide and dexamethasone has also shown promise as a treatment for AL amyloidosis. Other drugs used to treat myeloma such as lenalidomide have shown promise in treating AL amyloidosis.[134]
Chemotherapy drugs are also used in conditioning regimens prior to bone marow transplant (hematopoietic stem cell transplant). Conditioning regimens are used to suppress the recipient's immune system in order to allow a transplant to engraft. Cyclophosphamide is a common cytotoxic drug used in this manner, and is often used in conjunction with total body irradiation. Chemotherapeutic drugs may be used at high doses to permanently remove the recipient's bone marrow cells (myeloablative conditioning) or at lower doses that will prevent permanent bone marrow loss (non-myeloablative and reduced intensity conditioning).[135] When used in non-cancer setting, the treatment is still called Chemotherapy, and is often done in the same treatment center as cancer patients.
Occupational precautions
Healthcare workers exposed to antineoplastic agents take precautions to keep their exposure to a minimum. There is a limitation in cytotoxics dissolution in Australia and the United States to 20 dissolutions per pharmacist/nurse,[來源請求] since pharmacists who prepare these drugs or nurses who may prepare or administer them are the two occupational groups with the highest potential exposure to antineoplastic agents. In addition, physicians and operating room personnel may also be exposed through the treatment of patients. Hospital staff, such as shipping and receiving personnel, custodial workers, laundry workers, and waste handlers, all have potential exposure to these drugs during the course of their work. The increased use of antineoplastic agents in veterinary oncology also puts these workers at risk for exposure to these drugs.[136][137] Routes of entry into the worker's body are skin absorption, inhalation, and ingestion via hand-to-mouth.[137] The long-term effects of exposure include chromosomal abnormalities and infertility.[138]
Available agents
There is an extensive list of antineoplastic agents. Several classification schemes have been used to subdivide the medicines used for cancer into several different types.[來源請求]
History

The first use of small-molecule drugs to treat cancer was in the early 20th century, although the specific chemicals first used were not originally intended for that purpose. Mustard gas was used as a chemical warfare agent during World War I and was discovered to be a potent suppressor of hematopoiesis (blood production).[139] A similar family of compounds known as nitrogen mustards were studied further during World War II at the Yale School of Medicine.[140] It was reasoned that an agent that damaged the rapidly growing white blood cells might have a similar effect on cancer.[140] Therefore, in December 1942, several patients with advanced lymphomas (cancers of the lymphatic system and lymph nodes) were given the drug by vein, rather than by breathing the irritating gas.[140] Their improvement, although temporary, was remarkable.[141] Concurrently, during a military operation in World War II, following a German air raid on the Italian harbour of Bari, several hundred people were accidentally exposed to mustard gas, which had been transported there by the Allied forces to prepare for possible retaliation in the event of German use of chemical warfare. The survivors were later found to have very low white blood cell counts.[142] After WWII was over and the reports declassified, the experiences converged and led researchers to look for other substances that might have similar effects against cancer. The first chemotherapy drug to be developed from this line of research was mustine. Since then, many other drugs have been developed to treat cancer, and drug development has exploded into a multibillion-dollar industry, although the principles and limitations of chemotherapy discovered by the early researchers still apply.[143]
The term chemotherapy
The word chemotherapy without a modifier usually refers to cancer treatment, but its historical meaning was broader. The term was coined in the early 1900s by Paul Ehrlich as meaning any use of chemicals to treat any disease (chemo- + -therapy), such as the use of antibiotics (antibacterial chemotherapy).[144] Ehrlich was not optimistic that effective chemotherapy drugs would be found for the treatment of cancer.[144] The first modern chemotherapeutic agent was arsphenamine, an arsenic compound discovered in 1907 and used to treat syphilis.[145] This was later followed by sulfonamides (sulfa drugs) and penicillin. In today's usage, the sense "any treatment of disease with drugs" is often expressed with the word pharmacotherapy.
Sales
Many of the most commonly used chemotherapy agents, such as cisplatin/carboplatin, docetaxel, gemcitabine, paclitaxel, vinorelbine and pemetrexed are off-patent, so they don't cost billions of dollars. The top 10 best-selling (in terms of revenue) cancer drugs of 2013:[146]
| No. | 2013 Global Sales | INN | Trade names | Companies | Indications |
|---|---|---|---|---|---|
| 1 | $7.78 billion | Rituximab | Rituxan/MabThera | Roche, Pharmstandard | non-Hodgkin's lymphoma, CLL |
| 2 | $6.75 billion | Bevacizumab | Avastin | Roche | Colorectal, lung, ovarian and brain cancer |
| 3 | $6.56 billion | Trastuzumab | Herceptin | Roche | Breast, esophagus and stomach cancer |
| 4 | $4.69 billion | Imatinib | Gleevec | Novartis | Leukemia, GI cancer |
| 5 | $1.09 billion | Lenalidomide | Revlimid | Celgene, Pharmstandard | Multiple myeloma, mantle cell lymphoma |
| 6 | $2.7 billion | Pemetrexed | Alimta | Eli Lilly | Lung cancer |
| 7 | $2.6 billion | Bortezomib | Velcade | Johnson & Johnson, Takeda, Pharmstandard | Multiple myeloma |
| 8 | $1.87 billion | Cetuximab | Erbitux | Merck KGaA, Bristol-Myers Squibb | Colon and head and neck cancer |
| 9 | $1.73 billion | Leuprorelin | Lupron, Eligard | AbbVie and Takeda; Sanofi and Astellas Pharma | Prostate and ovarian cancer |
| 10 | $1.7 billion | Abiraterone | Zytiga | Johnson & Johnson | Prostate cancer |
Research

Targeted therapies
Specially targeted delivery vehicles aim to increase effective levels of chemotherapy for tumor cells while reducing effective levels for other cells. This should result in an increased tumor kill and/or reduced toxicity.[147]
Antibody-drug conjugates
Antibody-drug conjugates (ADCs) comprise an antibody, drug and a linker between them. The antibody will be targeted at a preferentially expressed protein in the tumour cells (known as a tumor antigen) or on cells that the tumor can utilise, such as blood vessel endothelial cells. They bind to the tumor antigen and are internalised, where the linker releases the drug into the cell. These specially targeted delivery vehicles vary in their stability, selectivity, and choice of target, but, in essence, they all aim to increase the maximum effective dose that can be delivered to the tumor cells.[148] Reduced systemic toxicity means that they can also be used in sicker patients, and that they can carry new chemotherapeutic agents that would have been far too toxic to deliver via traditional systemic approaches.[來源請求]
The first approved drug of this type was gemtuzumab ozogamicin (Mylotarg), released by Wyeth (now Pfizer). The drug was approved to treat acute myeloid leukemia, but has now been withdrawn from the market because the drug did not meet efficacy targets in further clinical trials.[149][150] Two other drugs, trastuzumab emtansine and brentuximab vedotin, are both in late clinical trials, and the latter has been granted accelerated approval for the treatment of refractory Hodgkin's lymphoma and systemic anaplastic large cell lymphoma.[148]
Nanoparticles
Nanoparticles are 1-1000 nanometer (nm) sized particles that can promote tumor selectivity and aid in delivering low-solubility drugs. Nanoparticles can be targeted passively or actively. Passive targeting exploits the difference between tumor blood vessels and normal blood vessels. Blood vessels in tumors are "leaky" because they have gaps from 200-2000 nm, which allow nanoparticles to escape into the tumor. Active targeting uses biological molecules (antibodies, proteins, DNA and receptor ligands) to preferentially target the nanoparticles to the tumor cells. There are many types of nanoparticle delivery systems, such as silica, polymers, liposomes and magnetic particles. Nanoparticles made of magnetic material can also be used to concentrate agents at tumor sites using an externally applied magnetic field.[147] They have emerged as a useful vehicle in magnetic drug delivery for poorly soluble agents such as paclitaxel.[151]
Electrochemotherapy
Electrochemotherapy is the combined treatment in which injection of a chemotherapeutic drug is followed by application of high-voltage electric pulses locally to the tumor. The treatment enables the chemotherapeutic drugs, which otherwise cannot or hardly go through the membrane of cells (such as bleomycin and cisplatin), to enter the cancer cells. Hence, greater effectiveness of antitumor treatment is achieved.
Clinical electrochemotherapy has been successfully used for treatment of cutaneous and subcutaneous tumors irrespective of their histological origin.[152][153][154][155][156][157] The method has been reported as safe, simple and highly effective in all reports on clinical use of electrochemotherapy. According to the ESOPE project (European Standard Operating Procedures of Electrochemotherapy), the Standard Operating Procedures (SOP) for electrochemotherapy were prepared, based on the experience of the leading European cancer centres on electrochemotherapy.[154][158] Recently, new electrochemotherapy modalities have been developed for treatment of internal tumors using surgical procedures, endoscopic routes or percutaneous approaches to gain access to the treatment area.[159][160]
Hyperthermia therapy
Hyperthermia therapy is heat treatment for cancer that can be a powerful tool when used in combination with chemotherapy (thermochemotherapy) or radiation for the control of a variety of cancers. The heat can be applied locally to the tumor site, which will dilate blood vessels to the tumor, allowing more chemotherapeutic medication to enter the tumor. Additionally, the bi-lipid layer of the tumor cell membrane will become more porous, further allowing more of the chemotherapeutic medicine to enter the tumor cell.
Hyperthermia has also been shown to help prevent or reverse "chemo-resistance." Chemotherapy resistance sometimes develops over time as the tumors adapt and can overcome the toxicity of the chemo medication. "Overcoming chemoresistance has been extensively studied within the past, especially using CDDP-resistant cells. In regard to the potential benefit that drug-resistant cells can be recruited for effective therapy by combining chemotherapy with hyperthermia, it was important to show that chemoresistance against several anticancer drugs (e.g. mitomycin C, anthracyclines, BCNU, melphalan) including CDDP could be reversed at least partially by the addition of heat.[161]
Other animals
Chemotherapy is used in veterinary medicine similar to how it is used in human medicine.[162]
參見
参考文献
- ^ 1.0 1.1 1.2 1.3 1.4 1.5 Corrie PG, Pippa G. Cytotoxic chemotherapy: clinical aspects. Medicine. 2008, 36 (1): 24–28. doi:10.1016/j.mpmed.2007.10.012.
- ^ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Airley, pp. 55-59
- ^ Wood, pp. 17-18
- ^ Perry, p. 42
- ^ Epstein RJ. Maintenance therapy to suppress micrometastasis: the new challenge for adjuvant cancer treatment. Clinical Cancer Research. Aug 2005, 11 (15): 5337–41. PMID 16061845. doi:10.1158/1078-0432.CCR-05-0437.
- ^ Skeel RT. Handbook of Cancer Chemotherapy (paperback) 6th. Lippincott Williams & Wilkins. 2003. ISBN 0-7817-3629-3.
- ^ Chabner B, Longo DL. Cancer Chemotherapy and Biotherapy: Principles and Practice 4th. Philadelphia: Lippincott Willians & Wilkins. 2005. ISBN 0-7817-5628-6.
- ^ Nastoupil LJ, Rose AC, Flowers CR. Diffuse large B-cell lymphoma: current treatment approaches. Oncology. May 2012, 26 (5): 488–95. PMID 22730604.
- ^ Freedman A. Follicular lymphoma: 2012 update on diagnosis and management. American Journal of Hematology. Oct 2012, 87 (10): 988–95. PMID 23001911. doi:10.1002/ajh.23313.
- ^ Rampling R, James A, Papanastassiou V. The present and future management of malignant brain tumours: surgery, radiotherapy, chemotherapy. Journal of Neurology, Neurosurgery, and Psychiatry. Jun 2004,. 75 Suppl 2 (Suppl 2): ii24–30. PMC 1765659
 . PMID 15146036. doi:10.1136/jnnp.2004.040535.
. PMID 15146036. doi:10.1136/jnnp.2004.040535.
- ^ Madan V, Lear JT, Szeimies RM. Non-melanoma skin cancer. Lancet. Feb 2010, 375 (9715): 673–85. PMID 20171403. doi:10.1016/S0140-6736(09)61196-X.
- ^ Du Bois D; Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916.. Archives Internal Medicine: 303–11.
- ^ 13.0 13.1 13.2 Felici A.; J. Verweij; A. Sparreboom. Dosing strategies for anticancer drugs: the good, the bad and body-surface area. Eur J Cancer. 2002, 38 (13): 1677–84. doi:10.1016/s0959-8049(02)00151-x.
- ^ 14.0 14.1 14.2 Kaestner SA, Sewell GJ. Chemotherapy dosing part I: scientific basis for current practice and use of body surface area. Clinical Oncology. Feb 2007, 19 (1): 23–37. PMID 17305252. doi:10.1016/j.clon.2006.10.010.
- ^ Donald Pinkel. The Use of Body Surface Area as a Criterion of Drug Dosage in Cancer Chemotherapy. Cancer Res. August 1958, 18 (7): 853–6.
- ^ 16.0 16.1 Gurney H. How to calculate the dose of chemotherapy. British Journal of Cancer. Apr 2002, 86 (8): 1297–302. PMC 2375356
 . PMID 11953888. doi:10.1038/sj.bjc.6600139.
. PMID 11953888. doi:10.1038/sj.bjc.6600139.
- ^ 17.0 17.1 Beumer JH, Chu E, Salamone SJ. Body-surface area-based chemotherapy dosing: appropriate in the 21st century?. Journal of Clinical Oncology. Nov 2012, 30 (31): 3896–7. PMID 22965963. doi:10.1200/JCO.2012.44.2863.
- ^ 18.0 18.1 Baker SD; Verweij J; Rowinsky EK; Donehower RC; Schellens JH; Grochow LB; Sparreboom A. Role of body surface area in dosing of investigational anticancer agents in adults, 1991–2001. J Natl Cancer Inst. 2002, 94 (24): 1883–8. doi:10.1093/jnci/94.24.1883.
- ^ 19.00 19.01 19.02 19.03 19.04 19.05 19.06 19.07 19.08 19.09 Gamelin EC; Delva R; Jacob J; Merrouche Y; Raoul JL; Pezet D; Dorval E; Piot G; Morel A; Boisdron-Celle M. Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: Results of a multicenter randomized trial of patients with metastatic colorectal cancer. J Clin Oncol. 2008, 26 (13): 2099–2105. PMID 18445839. doi:10.1200/jco.2007.13.3934.
- ^ Saam J; Critchfield GC; Hamilton SA; Roa BB; Wenstrup RJ; Kaldate RR. Body Surface Area-based Dosing of 5-Fluorouracil Results in Extensive Interindividual Variability in 5-Fluorouracil Exposure in Colorectal Cancer Patients on FOLFOX Regimens. Clin Colorectal Cancer. 2011, 10 (3): 203–206. doi:10.1016/j.clcc.2011.03.015.
- ^ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 Capitain O; Asevoaia A; Boisdron-Celle M; Poirier AL; Morel A; Gamelin E. Individual Fluorouracil Dose Adjustment in FOLFOX Based on Pharmacokinetic Follow-Up Compared With Conventional Body-Area-Surface Dosing: A Phase II, Proof-of-Concept Study. Clin Colorectal Cancer. 2012, 11 (4): 263–267. doi:10.1016/j.clcc.2012.05.004.
- ^ Kaldate RR; Haregewoin A; Grier CE; Hamilton SA; McLeod HL. Modeling the 5-fluorouracil area under the curve versus dose relationship to develop a pharmacokinetic dosing algorithm for colorectal cancer patients receiving FOLFOX6. Oncologist: 296–302. doi:10.1634/theoncologist.2011-0357.
- ^ 23.0 23.1 23.2 Hunter RJ, Navo MA, Thaker PH, Bodurka DC, Wolf JK, Smith JA. Dosing chemotherapy in obese patients: actual versus assigned body surface area (BSA). Cancer Treat Rev. Feb 2009, 35 (1): 69–78. PMID 18922643. doi:10.1016/j.ctrv.2008.07.005.
- ^ Macbeth, p. 4
- ^ Buffery, PJ; Allen, KM; Chin, PKL; Moore, GA; Barclay, ML; Begg, EJ. Thirteen Years' Experience of Pharmacokinetic Monitoring and Dosing of Busulfan: Can the Strategy Be Improved?. Ther Drug Monit. 2014, 36 (1): 86–92.
- ^ Bartelink IH; Bredius RG; Belitser SV; Suttorp MM; Bierings M; Knibbe CA; Egeler M; Lankester AC; Egberts AC; Zwaveling J; Boelens JJ. Association Between Busulfan Exposure and Outcome in Children Receiving Intravenous Busulfan Before Hematopoietic Stem Cell Transplantation. Ther Drug Monit: 93–99.
- ^ ARK™ Methotrexate Assay. Ark Diagnostics.
- ^ Customizing Chemotherapy for Better Cancer Care. My Care Diagnostics.
- ^ A Brief History of BSA Dosing. My Care Diagnostics.
- ^ 30.0 30.1 Siddik ZH. Mechanisms of Action of Cancer Chemotherapeutic Agents: DNA-Interactive Alkylating Agents and Antitumour Platinum-Based Drugs. John Wiley & Sons, Ltd. 2005. doi:10.1002/0470025077.chap84b.
- ^ 31.0 31.1 31.2 31.3 31.4 31.5 Lind M.J., M.J. Principles of cytotoxic chemotherapy. Medicine. 2008, 36 (1): 19–23. doi:10.1016/j.mpmed.2007.10.003.
- ^ 32.0 32.1 32.2 Damia G, D'Incalci M. Mechanisms of resistance to alkylating agents. Cytotechnology. Sep 1998, 27 (1–3): 165–73. PMC 3449574
 . PMID 19002790. doi:10.1023/A:1008060720608.
. PMID 19002790. doi:10.1023/A:1008060720608.
- ^ 33.0 33.1 33.2 33.3 Malhotra V, Perry MC. Classical chemotherapy: mechanisms, toxicities and the therapeutic window. Cancer Biology & Therapy. 2003, 2 (4 Suppl 1): S2–4. PMID 14508075. doi:10.4161/cbt.199.
- ^ Giorgi-Renault S.; Renault J.; Baron M.; Gebel-Servolles P.; Delic J.; Cros S.; Paoletti C. Heterocyclic quinones XIII. Dimerization in the series of 5,8-quinazolinediones: Synthesis and anti tumor effects of bis(4-amino-5,8-quinazolinediones). Chem. Pharm. Bull. 1988, 36 (10): 3933–3947. doi:10.1248/cpb.36.3933.
- ^ Takimoto CH, Calvo E."Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ^ 36.0 36.1 36.2 Parker WB. Enzymology of purine and pyrimidine antimetabolites used in the treatment of cancer. Chemical Reviews. Jul 2009, 109 (7): 2880–93. PMC 2827868
 . PMID 19476376. doi:10.1021/cr900028p.
. PMID 19476376. doi:10.1021/cr900028p.
- ^ 37.0 37.1 Wood, p. 11
- ^ Adjei AA. Pemetrexed (ALIMTA), a novel multitargeted antineoplastic agent. Clinical Cancer Research. Jun 2004, 10 (12 Pt 2): 4276s–4280s. PMID 15217974. doi:10.1158/1078-0432.CCR-040010.
- ^ Wagstaff AJ, Ibbotson T, Goa KL. Capecitabine: a review of its pharmacology and therapeutic efficacy in the management of advanced breast cancer. Drugs. 2003, 63 (2): 217–36. PMID 12515569. doi:10.2165/00003495-200363020-00009.
- ^ Rowinsky EK, Donehower RC. The clinical pharmacology and use of antimicrotubule agents in cancer chemotherapeutics. Pharmacology & Therapeutics. Oct 1991, 52 (1): 35–84. PMID 1687171. doi:10.1016/0163-7258(91)90086-2.
- ^ 41.0 41.1 41.2 41.3 Yue QX, Liu X, Guo DA. Microtubule-binding natural products for cancer therapy. Planta Medica. Aug 2010, 76 (11): 1037–43. PMID 20577942. doi:10.1055/s-0030-1250073.
- ^ Damayanthi Y, Lown JW. Podophyllotoxins: current status and recent developments. Current Medicinal Chemistry. Jun 1998, 5 (3): 205–52. PMID 9562603.
- ^ Liu YQ, Yang L, Tian X, Cong; Zhang, Wei; Qian, Zhengnan; Hua, Zhong; Zhao, Qibo; Sui, Yu; Su, Wenhui; Zhang, Ming; Liu, Zhuhong; Liu, Guodong; Wu, Guangheng. Podophyllotoxin: current perspectives. Curr Bioactive Compounds. 2007, 3 (1): 37–66. doi:10.1016/j.jallcom.2006.06.070.
- ^ Lodish H, Berk A, Zipursky SL, et al. Molecular Cell Biology. 4th edition. The Role of Topoisomerases in DNA Replication. New York: W. H. Freeman. 2000.
- ^ Goodsell DS. The molecular perspective: DNA topoisomerases. Stem Cells. 2002, 20 (5): 470–1. PMID 12351817. doi:10.1634/stemcells.20-5-470.
- ^ Nitiss JL. Targeting DNA topoisomerase II in cancer chemotherapy. Nature Reviews. Cancer. May 2009, 9 (5): 338–50. PMC 2748742
 . PMID 19377506. doi:10.1038/nrc2607.
. PMID 19377506. doi:10.1038/nrc2607.
- ^ Antineoplastic Agents in Encyclopedia of Molecular Pharmacology, 2nd Edition, Volume 1. Eds. Offermanns S and Rosenthal W. Springer, 2008. ISBN 9783540389163 P 155
- ^ MInotti G et al. Anthracyclines in Encyclopedia of Molecular Pharmacology, 2nd Edition, Volume 1. Eds. Offermanns S and Rosenthal W. Springer, 2008. ISBN 9783540389163 P 91ff
- ^ Minotti G, Menna P, Salvatorelli E, Cairo G, Gianni L. Anthracyclines: molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacological Reviews. Jun 2004, 56 (2): 185–229. PMID 15169927. doi:10.1124/pr.56.2.6.
- ^ Sobell HM. Actinomycin and DNA transcription. Proceedings of the National Academy of Sciences of the United States of America. Aug 1985, 82 (16): 5328–31. Bibcode:1985PNAS...82.5328S. PMC 390561
 . PMID 2410919. doi:10.1073/pnas.82.16.5328.
. PMID 2410919. doi:10.1073/pnas.82.16.5328.
- ^ Dorr RT. Bleomycin pharmacology: mechanism of action and resistance, and clinical pharmacokinetics. Seminars in Oncology. Apr 1992, 19 (2 Suppl 5): 3–8. PMID 1384141.
- ^ Airley, p. 87
- ^ Verweij J, Pinedo HM. Mitomycin C: mechanism of action, usefulness and limitations. Anti-Cancer Drugs. Oct 1990, 1 (1): 5–13. PMID 2131038. doi:10.1097/00001813-199010000-00002.
- ^ Wood, Miriam, David Brighton. The Royal Marsden Hospital handbook of cancer chemotherapy: a guide for the multidisciplinary team. St. Louis, Mo: Elsevier Churchill Livingstone. 2005: 93–94. ISBN 0-443-07101-2.
- ^ Wood, pp. 113-118
- ^ Moreno-Ramirez D, de la Cruz-Merino L, Ferrandiz L, Villegas-Portero R, Nieto-Garcia A. Isolated limb perfusion for malignant melanoma: systematic review on effectiveness and safety. The Oncologist. 2010, 15 (4): 416–27. PMC 3227960
 . PMID 20348274. doi:10.1634/theoncologist.2009-0325.
. PMID 20348274. doi:10.1634/theoncologist.2009-0325.
- ^ Verhoef C, de Wilt JH, ten Hagen TL, Eggermont AM. Isolated hepatic perfusion for the treatment of liver tumors: sunset or sunrise?. Surgical Oncology Clinics of North America. Oct 2008, 17 (4): 877–94, xi. PMID 18722924. doi:10.1016/j.soc.2008.04.007.
- ^ Hendriks JM, Van Schil PE. Isolated lung perfusion for the treatment of pulmonary metastases. Surgical Oncology. 1998, 7 (1–2): 59–63. PMID 10421507. doi:10.1016/S0960-7404(98)00028-0.
- ^ Chitwood K, Etzkorn J, Cohen G. Topical and intralesional treatment of nonmelanoma skin cancer: efficacy and cost comparisons. Dermatologic Surgery. Sep 2013, 39 (9): 1306–16. PMID 23915332. doi:10.1111/dsu.12300.
- ^ Airley, p. 265
- ^ Huang, p. 130
- ^ Elad S, Zadik Y, Hewson I, Hovan A, Correa ME, Logan R, Elting LS, Spijkervet FK, Brennan MT. A systematic review of viral infections associated with oral involvement in cancer patients: a spotlight on Herpesviridea. Supportive Care in Cancer. Aug 2010, 18 (8): 993–1006. PMID 20544224. doi:10.1007/s00520-010-0900-3.
- ^ 63.0 63.1 Gafter-Gvili, Anat; Fraser, Abigail; Paul, Mical; Vidal, Liat; Lawrie, Theresa A.; van de Wetering, Marianne D.; Kremer, Leontien C. M.; Leibovici, Leonard. Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy. The Cochrane Database of Systematic Reviews. 2012-01-18, 1: CD004386. ISSN 1469-493X. PMC 4170789
 . PMID 22258955. doi:10.1002/14651858.CD004386.pub3.
. PMID 22258955. doi:10.1002/14651858.CD004386.pub3.
- ^ Coriolus Versicolor. Cancer.org. 2008-06-10 [7 August 2012].
- ^ Davila ML. Neutropenic enterocolitis. Current Opinion in Gastroenterology. Jan 2006, 22 (1): 44–7. PMID 16319675.
- ^ 66.0 66.1 Keidan RD, Fanning J, Gatenby RA, Weese JL. Recurrent typhlitis. A disease resulting from aggressive chemotherapy. Diseases of the Colon and Rectum. Mar 1989, 32 (3): 206–9. PMID 2920627. doi:10.1007/BF02554529.
- ^ Gibson RJ, Keefe DM. Cancer chemotherapy-induced diarrhoea and constipation: mechanisms of damage and prevention strategies. Supportive Care in Cancer. Sep 2006, 14 (9): 890–900. PMID 16604351. doi:10.1007/s00520-006-0040-y.
- ^ Groopman JE, Itri LM. Chemotherapy-induced anemia in adults: incidence and treatment. Journal of the National Cancer Institute. Oct 1999, 91 (19): 1616–34. PMID 10511589. doi:10.1093/jnci/91.19.1616.
- ^ Henry DH. The role of intravenous iron in cancer-related anemia. Oncology. Jul 2006, 20 (8 Suppl 6): 21–4. PMID 16925107.
- ^ Rodgers GM, Becker PS, Bennett CL, Cella D, Chanan-Khan A, Chesney C, Cleeland C, Coccia PF, Djulbegovic B, Garst JL, Gilreath JA, Kraut EH, Lin WC, Matulonis U, Millenson M, Reinke D, Rosenthal J, Sabbatini P, Schwartz RN, Stein RS, Vij R. Cancer- and chemotherapy-induced anemia. Journal of the National Comprehensive Cancer Network. Jul 2008, 6 (6): 536–64. PMID 18597709.
- ^ Vadhan-Raj S. Management of chemotherapy-induced thrombocytopenia: current status of thrombopoietic agents. Seminars in Hematology. Jan 2009, 46 (1 Suppl 2): S26–32. PMID 19245931. doi:10.1053/j.seminhematol.2008.12.007.
- ^ Sekhon SS, Roy V. Thrombocytopenia in adults: A practical approach to evaluation and management. Southern Medical Journal. May 2006, 99 (5): 491–8; quiz 499–500, 533. PMID 16711312. doi:10.1097/01.smj.0000209275.75045.d4.
- ^ Berger AM, Abernethy AP, Atkinson A, Barsevick AM, Breitbart WS, Cella D, Cimprich B, Cleeland C, Eisenberger MA, Escalante CP, Jacobsen PB, Kaldor P, Ligibel JA, Murphy BA, O'Connor T, Pirl WF, Rodler E, Rugo HS, Thomas J, Wagner LI. Cancer-related fatigue. Journal of the National Comprehensive Cancer Network. Aug 2010, 8 (8): 904–31. PMID 20870636.
- ^ Franklin DJ, Packel L. Cancer-related fatigue. Archives of Physical Medicine and Rehabilitation. Mar 2006, 87 (3 Suppl 1): S91–3; quiz S94–5. PMID 16500197. doi:10.1016/j.apmr.2005.12.015.
- ^ Cramp F, Byron-Daniel J. Cramp, Fiona , 编. Exercise for the management of cancer-related fatigue in adults. The Cochrane Database of Systematic Reviews. 2012, 11: CD006145. PMID 23152233. doi:10.1002/14651858.CD006145.pub3.
- ^ Gill, Paula; Grothey, Axel; Loprinzi, Charles. Nausea and Vomiting in the Cancer Patient. Oncology. 2006: 1482–1496 [2 September 2011]. ISBN 978-0-387-24291-0. doi:10.1007/0-387-31056-8_83.
Nausea and vomiting are two of the most feared cancer treatment-related side effects for cancer patients and their families.
- ^ Chadha V, Shenoi SD. Hair loss in cancer chemotherapeutic patients. Indian Journal of Dermatology, Venereology and Leprology. 2003, 69 (2): 131–132. PMID 17642856.
- ^ Lemieux J. Reducing chemotherapy-induced alopecia with scalp cooling. Clinical Advances in Hematology & Oncology. Oct 2012, 10 (10): 681–682. PMID 23187775.
- ^ Shapiro J, Price VH. Hair regrowth. Therapeutic agents. Dermatologic Clinics. Apr 1998, 16 (2): 341–356. PMID 9589208. doi:10.1016/S0733-8635(05)70017-6.
- ^ Al-Mohanna H, Al-Khenaizan S. Permanent alopecia following cranial irradiation in a child. Journal of Cutaneous Medicine and Surgery. 2010, 14 (3): 141–143. PMID 20487675. doi:10.2310/7750.2010.09014.
- ^ Can G, Demir M, Erol O, Aydiner A. A comparison of men and women's experiences of chemotherapy-induced alopecia. European Journal of Oncology Nursing. Jun 2013, 17 (3): 255–60. PMID 22901547. doi:10.1016/j.ejon.2012.06.003.
- ^ Trüeb RM. Chemotherapy-induced alopecia. Seminars in Cutaneous Medicine and Surgery. Mar 2009, 28 (1): 11–4. PMID 19341937. doi:10.1016/j.sder.2008.12.001.
- ^ Chon SY, Champion RW, Geddes ER, Rashid RM. Chemotherapy-induced alopecia. Journal of the American Academy of Dermatology. Jul 2012, 67 (1): e37–47. PMID 22178150. doi:10.1016/j.jaad.2011.02.026.
- ^ U. Rüther, C. Nunnensiek, H.-J. Schmoll,Secondary Neoplasias following Chemotherapy, Radiotherapy, and Immunosuppression, Contributions to Oncology (Beiträge zur Onkologie); Vol 55, 2000, ISBN 3-8055-7116-X
- ^ Hijiya N, Hudson MM, Lensing S, Zacher M, Onciu M, Behm FG, Razzouk BI, Ribeiro RC, Rubnitz JE, Sandlund JT, Rivera GK, Evans WE, Relling MV, Pui CH. Cumulative incidence of secondary neoplasms as a first event after childhood acute lymphoblastic leukemia. JAMA. Mar 2007, 297 (11): 1207–1215. PMID 17374815. doi:10.1001/jama.297.11.1207.
- ^ 86.0 86.1 86.2 86.3 Brydøy M, Fosså SD, Dahl O, Bjøro T. Gonadal dysfunction and fertility problems in cancer survivors. Acta Oncologica. 2007, 46 (4): 480–9. PMID 17497315. doi:10.1080/02841860601166958.
- ^ 87.0 87.1 Morgan S, Anderson RA, Gourley C, Wallace WH, Spears N. How do chemotherapeutic agents damage the ovary?. Human Reproduction Update. 2012, 18 (5): 525–35. PMID 22647504. doi:10.1093/humupd/dms022.
- ^ Gurgan T, Salman C, Demirol A. Pregnancy and assisted reproduction techniques in men and women after cancer treatment. Placenta. Oct 2008,. 29 Suppl B: 152–9. PMID 18790328. doi:10.1016/j.placenta.2008.07.007.
- ^ Courbiere B, Decanter C, Bringer-Deutsch S, Rives N, Mirallié S, Pech JC, De Ziegler D, Carré-Pigeon F, May-Panloup P, Sifer C, Amice V, Schweitzer T, Porcu-Buisson G, Poirot C. Emergency IVF for embryo freezing to preserve female fertility: a French multicentre cohort study. Human Reproduction. Sep 2013, 28 (9): 2381–8. PMID 23832792. doi:10.1093/humrep/det268.
- ^ Roness H, Kalich-Philosoph L, Meirow D. Prevention of chemotherapy-induced ovarian damage: possible roles for hormonal and non-hormonal attenuating agents. Human Reproduction Update. 2014, 20 (5): 759–774. PMID 24833728. doi:10.1093/humupd/dmu019.
- ^ Tichelli A, Rovó A. Fertility issues following hematopoietic stem cell transplantation. Expert Review of Hematology. Aug 2013, 6 (4): 375–388. PMID 23991924. doi:10.1586/17474086.2013.816507.
In turn citing: Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ, Doney K, Storb R, Sullivan K, Witherspoon R, Appelbaum FR. Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood. Apr 1996, 87 (7): 3045–3052. PMID 8639928. - ^ 92.0 92.1 92.2 92.3 92.4 92.5 Arnon J, Meirow D, Lewis-Roness H, Ornoy A. Genetic and teratogenic effects of cancer treatments on gametes and embryos. Human Reproduction Update. 2001, 7 (4): 394–403. PMID 11476352. doi:10.1093/humupd/7.4.394. [1]
- ^ 93.0 93.1 del Pino BM. Chemotherapy-induced Peripheral Neuropathy. NCI Cancer Bulletin. Feb 23, 2010;7(4):6.
- ^ Grisold W, Oberndorfer S, Windebank AJ. Chemotherapy and polyneuropathies. European Association of Neurooncology Magazine. 2012;12(1).
- ^ http://www.ehealthme.com/ds/herceptin/peripheral%20sensory%20neuropathy
- ^ Beijers AJM, Jongen, JLM & Vreugdenhil1 G. [2]. The Netherlands journal of medicine. January 2012 [archived 3 December 2013];70(1). PMID 22271810.
- ^ 97.0 97.1 Windebank AJ & Grisold W. Chemotherapy-induced neuropathy. Journal of the Peripheral Nervous System. 2008 Mar;13(1):27–46. doi:10.1111/j.1529-8027.2008.00156.x. PMID 18346229.
- ^ Savage L. Chemotherapy-induced pain puzzles scientists. Journal of the National Cancer Institute. 2007;99(14):1070–1071. doi:10.1093/jnci/djm072. PMID 17623791.
- ^ Tannock IF, Ahles TA, Ganz PA, Van Dam FS. Cognitive impairment associated with chemotherapy for cancer: report of a workshop. Journal of Clinical Oncology. Jun 2004, 22 (11): 2233–9. PMID 15169812. doi:10.1200/JCO.2004.08.094.
- ^ Wood, p. 202
- ^ Shaikh AY, Shih JA. Chemotherapy-induced cardiotoxicity. Current Heart Failure Reports. Jun 2012, 9 (2): 117–27. PMID 22382639. doi:10.1007/s11897-012-0083-y.
- ^ Thatishetty AV, Agresti N, O'Brien CB. Chemotherapy-induced hepatotoxicity. Clinics in Liver Disease. Nov 2013, 17 (4): 671–86, ix–x. PMID 24099024. doi:10.1016/j.cld.2013.07.010.
- ^ King PD, Perry MC. Hepatotoxicity of chemotherapy. The Oncologist. 2001, 6 (2): 162–76. PMID 11306728. doi:10.1634/theoncologist.6-2-162.
- ^ de Jonge MJ, Verweij J. Renal toxicities of chemotherapy. Seminars in Oncology. Feb 2006, 33 (1): 68–73. PMID 16473645. doi:10.1053/j.seminoncol.2005.11.011.
- ^ Humphreys BD, Soiffer RJ, Magee CC. Renal failure associated with cancer and its treatment: an update. Journal of the American Society of Nephrology. Jan 2005, 16 (1): 151–61. PMID 15574506. doi:10.1681/ASN.2004100843.
- ^ Brock PR, Knight KR, Freyer DR, Campbell KC, Steyger PS, Blakley BW, Rassekh SR, Chang KW, Fligor BJ, Rajput K, Sullivan M, Neuwelt EA. Platinum-induced ototoxicity in children: a consensus review on mechanisms, predisposition, and protection, including a new International Society of Pediatric Oncology Boston ototoxicity scale. Journal of Clinical Oncology. Jul 2012, 30 (19): 2408–17. PMC 3675696
 . PMID 22547603. doi:10.1200/JCO.2011.39.1110.
. PMID 22547603. doi:10.1200/JCO.2011.39.1110.
- ^ Rybak LP, Mukherjea D, Jajoo S, Ramkumar V. Cisplatin ototoxicity and protection: clinical and experimental studies. The Tohoku Journal of Experimental Medicine. Nov 2009, 219 (3): 177–86. PMC 2927105
 . PMID 19851045. doi:10.1620/tjem.219.177.
. PMID 19851045. doi:10.1620/tjem.219.177.
- ^ Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, Schrag D. Patients' expectations about effects of chemotherapy for advanced cancer. The New England Journal of Medicine. Oct 2012, 367 (17): 1616–25. PMC 3613151
 . PMID 23094723. doi:10.1056/NEJMoa1204410.
. PMID 23094723. doi:10.1056/NEJMoa1204410.
- ^ Deeken JF, Löscher W. The blood-brain barrier and cancer: transporters, treatment, and Trojan horses. Clinical Cancer Research. Mar 2007, 13 (6): 1663–74. PMID 17363519. doi:10.1158/1078-0432.CCR-06-2854.
- ^ Agarwala SS, Kirkwood JM. Temozolomide, a novel alkylating agent with activity in the central nervous system, may improve the treatment of advanced metastatic melanoma. The Oncologist. 2000, 5 (2): 144–51. PMID 10794805. doi:10.1634/theoncologist.5-2-144.
- ^ Gerstner ER, Fine RL. Increased permeability of the blood-brain barrier to chemotherapy in metastatic brain tumors: establishing a treatment paradigm. Journal of Clinical Oncology. Jun 2007, 25 (16): 2306–12. PMID 17538177. doi:10.1200/JCO.2006.10.0677.
- ^ Minchinton AI, Tannock IF. Drug penetration in solid tumours. Nature Reviews. Cancer. Aug 2006, 6 (8): 583–92. PMID 16862189. doi:10.1038/nrc1893.
- ^ Goldman B. Multidrug resistance: can new drugs help chemotherapy score against cancer?. Journal of the National Cancer Institute. Feb 2003, 95 (4): 255–7. PMID 12591977. doi:10.1093/jnci/95.4.255.
- ^ E. Crowley, CA. McDevitt, R. Callaghan. Multidrug Resistance in Cancer. Generating Inhibitors of P-Glycoprotein: Where to, Now?. Springer Protocols. 2009: 405–432.
- ^ Luqmani YA. Mechanisms of drug resistance in cancer chemotherapy. Medical Principles and Practice. 2005,. 14 Suppl 1: 35–48. PMID 16103712. doi:10.1159/000086183.
- ^ Moschovi, Maria. Drugs acting on homeostasis: challenging cancer cell adaptation.. Expert Rev Anticancer Ther. 2015, 15 (12): 1405–17. PMID 26523494. doi:10.1586/14737140.2015.1095095.
- ^ Gerber DE. Targeted therapies: a new generation of cancer treatments. American Family Physician. Feb 2008, 77 (3): 311–9. PMID 18297955.
- ^ Allen TM. Ligand-targeted therapeutics in anticancer therapy. Nature Reviews. Cancer. Oct 2002, 2 (10): 750–63. PMID 12360278. doi:10.1038/nrc903.
- ^ Chen HX, Cleck JN. Adverse effects of anticancer agents that target the VEGF pathway. Nature Reviews. Clinical Oncology. Aug 2009, 6 (8): 465–77. PMID 19581909. doi:10.1038/nrclinonc.2009.94.
- ^ Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nature Reviews. Cancer. Jan 2009, 9 (1): 28–39. PMID 19104514. doi:10.1038/nrc2559.
- ^ Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. Jan 2000, 100 (1): 57–70. PMID 10647931. doi:10.1016/S0092-8674(00)81683-9.
- ^ Hodgson S. Mechanisms of inherited cancer susceptibility. Journal of Zhejiang University. Science. B. Jan 2008, 9 (1): 1–4. PMC 2170461
 . PMID 18196605. doi:10.1631/jzus.B073001.
. PMID 18196605. doi:10.1631/jzus.B073001.
- ^ Perera FP. Environment and cancer: who are susceptible?. Science. Nov 1997, 278 (5340): 1068–73. Bibcode:1997Sci...278.1068P. PMID 9353182. doi:10.1126/science.278.5340.1068.
- ^ Randall, pp, 93-94
- ^ Kehe K, Balszuweit F, Steinritz D, Thiermann H. Molecular toxicology of sulfur mustard-induced cutaneous inflammation and blistering. Toxicology. Sep 2009, 263 (1): 12–9. PMID 19651324. doi:10.1016/j.tox.2009.01.019.
- ^ Makin G, Hickman JA. Apoptosis and cancer chemotherapy. Cell and Tissue Research. Jul 2000, 301 (1): 143–52. Bibcode:1994RSPTB.345..319H. PMID 10928287. doi:10.1007/s004419900160.
- ^ 127.0 127.1 Ben-Ari ET. Dual purpose: some cancer therapies used to treat autoimmune diseases. Journal of the National Cancer Institute. Apr 2004, 96 (8): 577–9. PMID 15100330. doi:10.1093/jnci/96.8.577.
- ^ 128.0 128.1 Cutolo M, Sulli A, Pizzorni C, Seriolo B, Straub RH. Anti-inflammatory mechanisms of methotrexate in rheumatoid arthritis. Annals of the Rheumatic Diseases. Aug 2001, 60 (8): 729–35. PMC 1753808
 . PMID 11454634. doi:10.1136/ard.60.8.729.
. PMID 11454634. doi:10.1136/ard.60.8.729.
- ^ Montaudié H, Sbidian E, Paul C, Maza A, Gallini A, Aractingi S, Aubin F, Bachelez H, Cribier B, Joly P, Jullien D, Le Maître M, Misery L, Richard MA, Ortonne JP. Methotrexate in psoriasis: a systematic review of treatment modalities, incidence, risk factors and monitoring of liver toxicity. Journal of the European Academy of Dermatology and Venereology. May 2011,. 25 Suppl 2: 12–8. PMID 21388454. doi:10.1111/j.1468-3083.2011.03991.x.
- ^ 130.0 130.1 Chen J, Veras MM, Liu C, Lin J. Chen, Junmin , 编. Methotrexate for ankylosing spondylitis. The Cochrane Database of Systematic Reviews. 2013, 2: CD004524. PMID 23450553. doi:10.1002/14651858.CD004524.pub4.
- ^ 131.0 131.1 Gray O, McDonnell GV, Forbes RB. Gray, Orla , 编. Methotrexate for multiple sclerosis. The Cochrane Database of Systematic Reviews. 2004, (2): CD003208. PMID 15106195. doi:10.1002/14651858.CD003208.pub2.
- ^ 132.0 132.1 Gray OM, McDonnell GV, Forbes RB. A systematic review of oral methotrexate for multiple sclerosis. Multiple Sclerosis. Aug 2006, 12 (4): 507–10. PMID 16900766. doi:10.1191/1352458506ms1299oa.
- ^ Ntali S, Bertsias G, Boumpas DT. Cyclophosphamide and lupus nephritis: when, how, for how long?. Clinical Reviews in Allergy & Immunology. Jun 2011, 40 (3): 181–91. PMID 20107927. doi:10.1007/s12016-009-8196-0.
- ^ NCCN Guidelines: Systemic Light Chain Amyloidosis (PDF). National Comprehensive Cancer Network.
- ^ Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, Apperley J, Slavin S, Pasquini M, Sandmaier BM, Barrett J, Blaise D, Lowski R, Horowitz M. Defining the intensity of conditioning regimens: working definitions. Biology of Blood and Marrow Transplantation. Dec 2009, 15 (12): 1628–33. PMC 2861656
 . PMID 19896087. doi:10.1016/j.bbmt.2009.07.004.
. PMID 19896087. doi:10.1016/j.bbmt.2009.07.004.
- ^ NIOSH Occupational Exposure to Antineoplastic Agents. United States National Institute for Occupational Safety and Health. [10 October 2007].
- ^ 137.0 137.1 Connor, Thomas H. Hazardous Drugs in Healthcare. NIOSH: Workplace Safety and Health. Medscape & NIOSH. March 7, 2011.
- ^ Wood, p. 38.
- ^ Krumbhaar EB. Role of the blood and the bone marrow in certain forms of gas poisoning. JAMA. 1919, 72: 39–41. doi:10.1001/jama.1919.26110010018009f.
- ^ 140.0 140.1 140.2 Fenn JE, Udelsman R. First use of intravenous chemotherapy cancer treatment: rectifying the record. Journal of the American College of Surgeons. Mar 2011, 212 (3): 413–417. PMID 21247779. doi:10.1016/j.jamcollsurg.2010.10.018.
- ^ Goodman LS; Wintrobe MM; Dameshek W; Goodman MJ; Gilman A; McLennan MT. Nitrogen mustard therapy. Use of methyl-bis(beta-chloroethyl)amine hydrochloride and tris(beta-chloroethyl)amine hydrochloride for Hodgkin's disease, lymphosarcoma, leukemia and certain allied and miscellaneous disorders. JAMA. 1946, 132 (3): 126–132. doi:10.1001/jama.1946.02870380008004.
- ^ Faguet, p. 71
- ^ Joensuu H. Systemic chemotherapy for cancer: from weapon to treatment. The Lancet. Oncology. Mar 2008, 9 (3): 304. PMID 18308256. doi:10.1016/S1470-2045(08)70075-5.
- ^ 144.0 144.1 DeVita VT, Chu E. A history of cancer chemotherapy. Cancer Research. Nov 2008, 68 (21): 8643–53. PMID 18974103. doi:10.1158/0008-5472.CAN-07-6611.
- ^ Nichols HJ, Walker JE. EXPERIMENTAL OBSERVATIONS ON THE PROPHYLAXIS AND TREATMENT OF SYPHILIS. The Journal of Experimental Medicine. Mar 1923, 37 (4): 525–42. PMC 2128372
 . PMID 19868743. doi:10.1084/jem.37.4.525.
. PMID 19868743. doi:10.1084/jem.37.4.525.
- ^ Top 10 best-selling cancer drugs of 2013; May 29, 2014
- ^ 147.0 147.1 Chidambaram M, Manavalan R, Kathiresan K. Nanotherapeutics to overcome conventional cancer chemotherapy limitations. Journal of Pharmacy & Pharmaceutical Sciences. 2011, 14 (1): 67–77. PMID 21501554.
- ^ 148.0 148.1 Teicher BA, Chari RV. Antibody conjugate therapeutics: challenges and potential. Clinical Cancer Research. Oct 2011, 17 (20): 6389–97. PMID 22003066. doi:10.1158/1078-0432.CCR-11-1417.
- ^ Sievers EL, Linenberger M. Mylotarg: antibody-targeted chemotherapy comes of age. Current Opinion in Oncology. Nov 2001, 13 (6): 522–7. PMID 11673694. doi:10.1097/00001622-200111000-00016.
- ^ FDA. Mylotarg (gemtuzumab ozogamicin): Market Withdrawal. [18 August 2013].
- ^ Vines T, Faunce T. Assessing the safety and cost-effectiveness of early nanodrugs. Journal of Law and Medicine. May 2009, 16 (5): 822–45. PMID 19554862.
- ^ Heller R, Gilbert R, Jaroszeski MJ. Clinical applications of electrochemotherapy. Advanced Drug Delivery Reviews. Jan 1999, 35 (1): 119–129. PMID 10837693. doi:10.1016/S0169-409X(98)00067-2.
- ^ Larkin JO, Collins CG, Aarons S, Tangney M, Whelan M, O'Reily S, Breathnach O, Soden DM, O'Sullivan GC. Electrochemotherapy: aspects of preclinical development and early clinical experience. Annals of Surgery. Mar 2007, 245 (3): 469–479. PMC 1877027
 . PMID 17435555. doi:10.1097/01.sla.0000250419.36053.33.
. PMID 17435555. doi:10.1097/01.sla.0000250419.36053.33.
- ^ 154.0 154.1 Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, Billard V, Geertsen PF, Larkin JO, Miklavcic D, Pavlovic I, Paulin-Kosir SM, Cemazar M, Morsli N, Soden DM, Rudolf Z, Robert C, O'Sullivan GC, Mir LM. Electrochemotherapy – An easy, highly effective and safe treatment of cutaneous and subcutaneous metastases. Eur J Cancer Suppl. 2006, 4 (11): 3–13. doi:10.1016/j.ejcsup.2006.08.002.
- ^ Möller MG, Salwa S, Soden DM, O'Sullivan GC. Electrochemotherapy as an adjunct or alternative to other treatments for unresectable or in-transit melanoma. Expert Review of Anticancer Therapy. Nov 2009, 9 (11): 1611–1630. PMID 19895245. doi:10.1586/era.09.129.
- ^ Testori A, Tosti G, Martinoli C, Spadola G, Cataldo F, Verrecchia F, Baldini F, Mosconi M, Soteldo J, Tedeschi I, Passoni C, Pari C, Di Pietro A, Ferrucci PF. Electrochemotherapy for cutaneous and subcutaneous tumor lesions: a novel therapeutic approach. Dermatologic Therapy. 2010, 23 (6): 651–661. PMID 21054709. doi:10.1111/j.1529-8019.2010.01370.x.
- ^ Hampton T. Electric pulses help with chemotherapy, may open new paths for other agents. JAMA. Feb 2011, 305 (6): 549–551. PMID 21304073. doi:10.1001/jama.2011.92.
- ^ Mir LM, Gehl J, Sersa G, Collins CG, Garbay JR, Billard V, Geertsen PF, Rudolf Z, O'Sullivan GC, Marty M. Standard operating procedures of the electrochemotherapy: Instructions for the use of bleomycin or cisplatin administered either systemically or locally and electric pulses delivered by the CliniporatorTM by means of invasive or non-invasive electrodes. Eur J Cancer Suppl. 2006, 4 (11): 14–25. doi:10.1016/j.ejcsup.2006.08.003.
- ^ Soden DM, Larkin JO, Collins CG, Tangney M, Aarons S, Piggott J, Morrissey A, Dunne C, O'Sullivan GC. Successful application of targeted electrochemotherapy using novel flexible electrodes and low dose bleomycin to solid tumours. Cancer Letters. Feb 2006, 232 (2): 300–310. PMID 15964138. doi:10.1016/j.canlet.2005.03.057.
- ^ Miklavcic D, Snoj M, Zupanic A, Kos B, Cemazar M, Kropivnik M, Bracko M, Pecnik T, Gadzijev E, Sersa G. Towards treatment planning and treatment of deep-seated solid tumors by electrochemotherapy. BioMedical Engineering OnLine. 2010, 9 (1): 10. PMC 2843684
 . PMID 20178589. doi:10.1186/1475-925X-9-10.
. PMID 20178589. doi:10.1186/1475-925X-9-10.
- ^ Issels, R. Hyperthermia Combined with Chemotherapy – Biological Rationale, Clinical Application, and Treatment Results. Onkologie. 1999, 22 (5): 374–381. doi:10.1159/000026986.
- ^ McKnight JA. Principles of chemotherapy. Clinical Techniques in Small Animal Practice. May 2003, 18 (2): 67–72. PMID 12831063. doi:10.1053/svms.2003.36617.
外部連結
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||





