胃癌:修订间差异
无编辑摘要 |
无编辑摘要 |
||
| 第1行: | 第1行: | ||
{{translating|time=2017-05-16T20:00:04+00:00}} |
|||
{{medical}} |
{{medical}} |
||
{{Infobox medical condition |
{{Infobox medical condition |
||
| 第40行: | 第41行: | ||
<!--This is believed to be due to the eating of less salted and pickled foods as a result of the development of [[refrigeration]] as a method of keeping food fresh.<ref>{{cite book|last1=Moore|first1=edited by Rhonda J.|last2=Spiegel|first2=David|title=Cancer, culture, and communication|date=2004|publisher=Kluwer Academic|location=New York|isbn=9780306478857|page=139|url=https://books.google.com/books?id=kHLlOePrWgYC&pg=PA139}}</ref> Stomach cancer occurs most commonly in [[East Asia]] and [[Eastern Europe]].<!-- <ref name=WCR2014/> --><!--It occurs twice as often in males as in females.<ref name=WCR2014>{{cite book|title=World Cancer Report 2014|date=2014|publisher=World Health Organization|isbn=9283204298|pages=Chapter 5.4}}</ref>--> |
<!--This is believed to be due to the eating of less salted and pickled foods as a result of the development of [[refrigeration]] as a method of keeping food fresh.<ref>{{cite book|last1=Moore|first1=edited by Rhonda J.|last2=Spiegel|first2=David|title=Cancer, culture, and communication|date=2004|publisher=Kluwer Academic|location=New York|isbn=9780306478857|page=139|url=https://books.google.com/books?id=kHLlOePrWgYC&pg=PA139}}</ref> Stomach cancer occurs most commonly in [[East Asia]] and [[Eastern Europe]].<!-- <ref name=WCR2014/> --><!--It occurs twice as often in males as in females.<ref name=WCR2014>{{cite book|title=World Cancer Report 2014|date=2014|publisher=World Health Organization|isbn=9283204298|pages=Chapter 5.4}}</ref>--> |
||
==前兆與症狀(Signs and symptoms)== |
|||
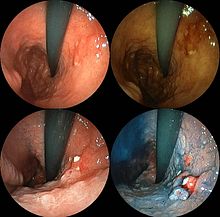
[[File:Linitis plastica 2.jpg|thumb|right|Endoscopic image of [[linitis plastica]], a type of stomach cancer where the entire [[stomach]] is invaded, leading to a leather bottle-like appearance with [[bleeding|blood]] coming out of it.]] |
|||
[[File:Por-sig.jpg|thumb|right|Endoscopic images of the stomach cancer in early stage. Its histology was poorly differentiated [[adenocarcinoma]] with [[signet ring cells]]. Left above: normal, right above: FICE, left low: acetate stained, right low: AIM stained]] |
|||
Stomach cancer is often either [[asymptomatic]] (producing no noticeable symptoms) or it may cause only [[nonspecific symptoms]] (symptoms that are specific to stomach cancer and to other related or unrelated disorders) in its early stages. By the time symptoms occur, the cancer has often reached an advanced stage (see below) and may have metastasized (spread to other, perhaps distant, parts of the body), which is one of the main reasons for its relatively poor prognosis.<ref name="SAOGC">{{cite web |url=http://www.cancerresearchuk.org/cancer-help/type/stomach-cancer/treatment/statistics-and-outlook-for-stomach-cancer|title=Statistics and outlook for stomach cancer|publisher=Cancer Research UK |accessdate=19 February 2014}}</ref> Stomach cancer can cause the following signs and symptoms: |
|||
Early cancers may be associated with [[indigestion]] or a burning sensation ([[heartburn]]). However, less than 1 in every 50 people referred for endoscopy due to indigestion has cancer.<ref>{{cite web|url=http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4080278.pdf |title=Guidance on Commissioning Cancer Services Improving Outcomes in Upper Gastro-intestinal Cancers |publisher=NHS|date=Jan 2001}}</ref> [[Abdominal pain|Abdominal discomfort]] and [[loss of appetite]], especially for meat, can occur. |
|||
Gastric cancers that have enlarged and invaded normal tissue can cause [[weakness]], [[fatigue (physical)|fatigue]], [[bloating]] of the stomach after meals, [[abdominal pain]] in the upper abdomen, [[nausea]] and occasional [[vomiting]], [[diarrhea]] or [[constipation]]. Further enlargement may cause [[weight loss]] or [[bleeding]] with [[vomiting blood]] or having [[blood in the stool]], the latter apparent as black discolouration ([[melena]]) and sometimes leading to [[anemia]]. [[Dysphagia]] suggests a tumour in the [[cardia]] or extension of the gastric tumour into the [[esophagus]]. |
|||
These can be symptoms of other problems such as a [[stomach virus]], [[gastric ulcer]], or [[tropical sprue]]. |
|||
== 簡介 == |
== 簡介 == |
||
大多數的胃部腫瘤都是腺癌大約佔99%,大致上又可再分為[[淋巴瘤]]與[[間充質|間質]]瘤。大多時候胃癌會經年累月地持續惡化<ref name=WCR2014/>。根據[[世界衛生組織]]估計,胃癌是全世界排名第四個最普遍被診斷的癌症,而且是所有癌症死亡率排名第二高,被視為國際間重要的健康危機<!--。在2006年統計中顯示接近有950,000個案例發生,而且大約將近700,000位病人死於這一種疾病-->。胃癌的高發生率包括[[東亞]]、[[南美洲]]和[[東歐]]國家。在[[台灣]]地區,胃癌發生率尤其偏高,每100,000人口約有8.52人至9.68人,胃癌名列2006年癌症死亡原因第5位,約有2500人死於胃癌,每100,000人口死亡率為11.4% ,但胃癌若是極早期僅在表面型的五年存活率幾乎接近95%以上,而一旦擴散存活率會急降是其特性。 |
大多數的胃部腫瘤都是腺癌大約佔99%,大致上又可再分為[[淋巴瘤]]與[[間充質|間質]]瘤。大多時候胃癌會經年累月地持續惡化<ref name=WCR2014/>。根據[[世界衛生組織]]估計,胃癌是全世界排名第四個最普遍被診斷的癌症,而且是所有癌症死亡率排名第二高,被視為國際間重要的健康危機<!--。在2006年統計中顯示接近有950,000個案例發生,而且大約將近700,000位病人死於這一種疾病-->。胃癌的高發生率包括[[東亞]]、[[南美洲]]和[[東歐]]國家。在[[台灣]]地區,胃癌發生率尤其偏高,每100,000人口約有8.52人至9.68人,胃癌名列2006年癌症死亡原因第5位,約有2500人死於胃癌,每100,000人口死亡率為11.4% ,但胃癌若是極早期僅在表面型的五年存活率幾乎接近95%以上,而一旦擴散存活率會急降是其特性。 |
||
| 第54行: | 第65行: | ||
另有一種普通非癌的胃手術後20年左右可能產生的[[殘胃癌]]現象。 |
另有一種普通非癌的胃手術後20年左右可能產生的[[殘胃癌]]現象。 |
||
== 引發原因 == |
== 引發原因 (Causes)== |
||
一般醫學上所謂的「危險因子」是指任何會增加得到某疾病的機會的「事物」。雖然大多數癌症的形成原因,至今仍不十分明瞭,它可能是由許多因子,經過許多過程逐步轉變而來的,對不同癌症而言,則也有不同「事物」會增加其癌變發生的機會。譬如吸煙的人較容易得到肺癌,咽喉癌較大。 |
一般醫學上所謂的「危險因子」是指任何會增加得到某疾病的機會的「事物」。雖然大多數癌症的形成原因,至今仍不十分明瞭,它可能是由許多因子,經過許多過程逐步轉變而來的,對不同癌症而言,則也有不同「事物」會增加其癌變發生的機會。譬如吸煙的人較容易得到肺癌,咽喉癌較大。 |
||
| 第86行: | 第97行: | ||
[[煙草]]和[[酒精]]濫用:這些生活習慣也都會增加胃癌發生機會。 |
[[煙草]]和[[酒精]]濫用:這些生活習慣也都會增加胃癌發生機會。 |
||
Gastric cancer occurs as a result of many factors.<ref>{{cite journal |vauthors=Lee YY, Derakhshan MH |date=Jun 2013 | title = Environmental and lifestyle risk factors of gastric cancer | url = | journal = Arch. Iran. Med. | volume = 16 | issue = 6| pages = 358–65 | pmid = 23725070 }}</ref> It occurs twice as common in males as females. [[Estrogen]] may protect women against the development of this cancer form.<ref>{{cite journal | author = Chandanos E, Lagergren J | date = Nov 2008 | title = Oestrogen and the enigmatic male predominance of gastric cancer | url = | journal = Eur J Cancer | volume = 44 | issue = 16| pages = 2397–403 | doi=10.1016/j.ejca.2008.07.031}}</ref><ref>{{cite journal | author = Qin J, Liu M, Ding Q, Ji X, Hao Y, Wu X, Xiong J | date = Oct 2014 | title = The direct effect of estrogen on cell viability and apoptosis in human gastric cancer cells | url = | journal = Mol Cell Biochem | volume = 395 | issue = 1–2| pages = 99–107 | doi=10.1007/s11010-014-2115-2}}</ref> |
|||
===Infections=== |
|||
''[[Helicobacter pylori]]'' infection is an essential risk factor in 65–80% of gastric cancers, but only 2% of people with Helicobacter infections develop stomach cancer.<ref name="GVRF-4">{{cite web|url=http://www.who.int/vaccine_research/documents/en/gvrf2003.pdf |title=Proceedings of the fourth Global Vaccine Research Forum |date=April 2004 |work=Initiative for Vaccine Research team of the Department of Immunization, Vaccines and Biologicals |publisher=WHO |quote=Epidemiology of ''Helicobacter pylori'' and gastric cancer… |accessdate=2009-05-11}}</ref><ref name="pmid24011243">{{cite journal| author= González CA, Sala N, Rokkas T | title=Gastric cancer: epidemiologic aspects| journal=Helicobacter| year=2013 | volume=18 | issue=Supplement 1 | pages=34–38 | pmid=24011243 | doi=10.1111/hel.12082| last2=Sala| last3=Rokkas}}</ref> The mechanism by which ''H. pylori'' induces stomach cancer potentially involves chronic inflammation, or the action of ''H. pylori'' virulence factors such as [[CagA]].<ref name="pmid16367902">{{cite journal | author = Hatakeyama, M. & Higashi, H | title = Helicobacter pylori CagA: a new paradigm for bacterial carcinogenesis | journal = Cancer Science | volume = 96 | issue = 12| pages = 835–843 | year = 2005 | pmid = 16367902 | doi = 10.1111/j.1349-7006.2005.00130.x | last2 = Higashi }}</ref> It was estimated that [[Epstein–Barr virus]] is responsible for 84,000 cases per year.<ref>{{cite web|url=http://www.cancerresearchuk.org/about-us/cancer-news/press-release/2014-03-24-developing-a-vaccine-for-the-epstein-barr-virus-could-prevent-up-to-200000-cancers-globally-say |title=Developing a vaccine for the Epstein-Barr Virus could prevent up to 200,000 cancers globally say experts |website=Cancer Research UK |date= |accessdate=2017-03-17}}</ref> [[AIDS]] is also associated with elevated risk.<ref name="pmid24011243"/>===Smoking=== |
|||
Smoking increases the risk of developing gastric cancer significantly, from 40% increased risk for current smokers to 82% increase for heavy smokers. Gastric cancers due to smoking mostly occur in the upper part of the stomach near the [[esophagus]].<ref name=ACS_Risk/><ref>{{cite journal | author = Nomura A, Grove JS, Stemmermann GN, Severson RK | title = Cigarette smoking and stomach cancer | journal = Cancer Research | volume = 50 | issue = 21 | page = 7084 | year = 1990 | pmid = 2208177 | doi = | url = http://cancerres.aacrjournals.org/cgi/pmidlookup?view=long&pmid=2208177 | last2 = Grove | last3 = Stemmermann | last4 = Severson }}</ref><ref>{{cite journal | author = Trédaniel J, Boffetta P, Buiatti E, Saracci R, Hirsch A | title = Tobacco smoking and gastric cancer: Review and meta-analysis | journal = International Journal of Cancer | volume = 72 | issue = 4 | pages = 565–73 |date=August 1997 | pmid = 9259392 | doi = 10.1002/(SICI)1097-0215(19970807)72:4<565::AID-IJC3>3.0.CO;2-O | last2 = Boffetta | last3 = Buiatti | last4 = Saracci | last5 = Hirsch }}</ref> Some studies show increased risk with alcohol consumption as well.<ref name="pmid24011243"/><ref name="pmid24191271">{{cite journal | author =Thrumurthy SG, Chaudry MA, Hochhauser D, Ferrier K, Mughal M | title = The diagnosis and management of gastric cancer| journal = British Medical Journal | volume = 347 | issue = 16| pages = 1695–6 | year = 2013 | pmid =24191271 | doi =10.1136/bmj.f6367 | last2 = Chaudry| last3 = Hochhauser| last4 = Mughal}}</ref> |
|||
===Diet=== |
|||
[[File:Sequence of 123-iodide total body human scintiscans.jpg|thumb|Sequence of 123-iodine human scintiscans after an intravenous injection: (from left) after 30 minutes, 20 hours and 48 hours. A high and rapid concentration of radio-iodine is evident in gastric mucosa of the stomach, in salivary glands, oral mucosa and in the periencephalic and cerebrospinal fluid (left). In the thyroid gland, I-concentration is more progressive, also in the reservoir (from 1% after 30 minutes to 5.8 % after 48 hours, of the total injected dose).<ref>{{cite journal |pages=727–9 |doi=10.1089/10507250050137851 |title=Environmental Iodine Deficiency: A Challenge to the Evolution of Terrestrial Life? |year=2000 |last1=Venturi |first1=S. |last2=Donati |first2=F.M. |last3=Venturi |first3=A. |last4=Venturi |first4=M. |journal=Thyroid |volume=10 |issue=8 |pmid=11014322}}</ref>]] |
|||
Dietary factors are not proven causes,<ref name="Merck-1">{{MerckManual|02|021|d||Tumors of the GI Tract}}</ref> but some foods including smoked foods,<ref name="pmid16865769">{{cite journal| author=Jakszyn P, González CA | title=Nitrosamine and related food intake and gastric and oesophageal cancer risk: A systematic review of the epidemiological evidence| journal=World J Gastroenterol| year=2006 | volume=12 | issue=27 | pages=4296–4303 | pmid=16865769| pmc=4087738| url = http://www.wjgnet.com/1007-9327/pdf/v12/i27/4296.pdf| last2=Gonzalez | doi=10.3748/wjg.v12.i27.4296}}</ref> salt and salt-rich foods, red meat, [[processed meat]], pickled vegetables,<ref name="pmid24011243"/> and [[bracken]]<ref>{{cite journal | author = Alonso-Amelot ME, Avendaño M | title = Human carcinogenesis and bracken fern: a review of the evidence | journal = Current Medicinal Chemistry | volume = 9 | issue = 6 | pages = 675–86 |date=March 2002| pmid = 11945131 | doi = 10.2174/0929867023370743| url = http://www.benthamdirect.org/pages/content.php?CMC/2002/00000009/00000006/0004C.SGM | last2 = Avendaño }}</ref> are [[association (statistics)|associated]] with a higher risk of stomach cancer. Nitrates and nitrites in cured meats can be converted by certain bacteria, including ''H. pylori'', into compounds that have been found to cause stomach cancer in animals. |
|||
Fresh fruit and vegetable intake, citrus fruit intake, and [[antioxidant]] intake are associated with a lower risk of stomach cancer.<ref name="pmid24011243"/><ref name=ACS_Risk>{{cite web|url=http://www.cancer.org/cancer/stomachcancer/detailedguide/stomach-cancer-risk-factors|title=What Are The Risk Factors For Stomach Cancer(Website)|publisher=American Cancer Society|accessdate=2010-03-31}}</ref> A Mediterranean diet is associated with lower rates of stomach cancer,<ref name="American Journal of Clinical Nutrition">{{cite journal | author = Buckland G, Agudo A, Lujan L, Jakszyn P, Bueno-De-Mesquita HB, Palli D, Boeing H, Carneiro F, Krogh V | title = Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study | journal = American Journal of Clinical Nutrition | volume = 91 | issue = 2 | pages = 381–90 | year = 2009 | pmid = 20007304 | doi = 10.3945/ajcn.2009.28209 | last2 = Agudo | last3 = Luján | last4 = Jakszyn | last5 = Bueno-De-Mesquita | last6 = Palli | last7 = Boeing | last8 = Carneiro | last9 = Krogh | last10 = Sacerdote | last11 = Tumino | last12 = Panico | last13 = Nesi | last14 = Manjer | last15 = Regnér | last16 = Johansson | last17 = Stenling | last18 = Sanchez | last19 = Dorronsoro | last20 = Barricarte | last21 = Navarro | last22 = Quirós | last23 = Allen | last24 = Key | last25 = Bingham | last26 = Kaaks | last27 = Overvad | last28 = Jensen | last29 = Olsen | last30 = Tjønneland | display-authors = 29 }}</ref> as is regular [[aspirin]] use.<ref name="pmid24011243"/> |
|||
Obesity is a physical risk factor that has been found to increase the risk of gastric adenocarcinoma by contributing to the development of [[gastroesophageal reflux disease]] (GERD).<ref name="crew">{{cite journal |vauthors=Crew K, Neugut A | title = Epidemiology of gastric cancer | journal = World Journal of Gastroenterology | volume = 12 | issue = 3 | pages = 354–62 |date=January 2006|PMC=4066052|pmid=16489633|doi=10.3748/wjg.v12.i3.354}}</ref> The exact mechanism by which obesity causes GERD is not completely known. Studies hypothesize that increased dietary fat leading to increased pressure on the stomach and the lower esophageal sphincter, due to excess adipose tissue, could play a role, yet no statistically significant data has been collected.<ref name="hamp">{{cite journal |author1=Hampel Howard |author2=Abraham Neena S. |author3=El-Serag Hashem B. | title = Meta-Analysis: obesity and the risk for gastroesophageal reflux disease and its complications | journal = Annals of Internal Medicine | volume = 143 | issue = 3 | pages = 199–211 |date=August 2005 | doi=10.7326/0003-4819-143-3-200508020-00006}}</ref> However, the risk of gastric cardia adenocarcinoma, with GERD present, has been found to increase more than 2 times for an obese person.<ref name="crew"/> There is a correlation between [[iodine deficiency]] and gastric cancer.<ref>{{Cite book|last=Josefssson |first=M. |last2=Ekblad |first2=E. |year=2009 |pages=215–220|chapter=22. Sodium Iodide Symporter (NIS) in Gastric Mucosa: Gastric Iodide Secretion |title=Comprehensive Handbook of Iodine: Nutritional, Biochemical, Pathological and Therapeutic Aspects |editor-first=Victor R. |editor-last=Preedy |editor2-first=Gerard N. |editor2-last=Burrow |editor3-first=Ronald |editor3-last=Watson|isbn=978-0-12-374135-6 |publisher=Elsevier}}</ref><ref>{{Cite journal|author=Venturi, Sebastiano|title=Evolutionary Significance of Iodine|journal=Current Chemical Biology-|volume=5|year=2011|issue=3 |pages=155–162 |issn=1872-3136|doi=10.2174/187231311796765012}}</ref><ref name="stod1">{{cite journal|last = Venturi II|first = S.|author2 =Donati, F.M.; Venturi, A.; Venturi, M.;|url=http://www.medsci.org/v05p0189.htm|title= Role of iodine in evolution and carcinogenesis of thyroid, breast and stomach.|journal= Adv Clin Path|year = 2000|volume = 4| pmid = 10936894 |issue = 1|pages = 11–17|last3 = Venturi|first3 = A|last4 = Venturi|first4 = M|last5 = Grossi|first5 = L|last6 = Guidi|first6 = A}}</ref> |
|||
===Genetics=== |
|||
About 10% of cases run in families and between 1% and 3% of cases are due to [[genetic syndrome]]s [[Heredity|inherited]] from a person's parents such as [[hereditary diffuse gastric cancer]].<ref name=WCR2014/> |
|||
A genetic risk factor for gastric cancer is a genetic defect of the [[CDH1 (gene)|CDH1 gene]] known as [[hereditary diffuse gastric cancer]] (HDGC). The CDH1 gene, which codes for E-cadherin, lies on the 16th chromosome.<ref name="chel"/> When the gene experiences a particular mutation, gastric cancer develops through a mechanism that is not fully understood.<ref name="chel">{{cite web |url=http://www.nostomachforcancer.org/gastric-cancer/hereditary-diffuse-gastric-cancer|title=Hereditary Diffuse Cancer|website= No Stomach for Cancer|accessdate=21 Oct 2014}}</ref> This mutation is considered autosomal dominant meaning that half of a carrier’s children will likely experience the same mutation.<ref name="chel"/> Diagnosis of hereditary diffuse gastric cancer usually takes place when at least two cases involving a family member, such as a parent or grandparent, are diagnosed, with at least one diagnosed before the age of 50.<ref name="chel"/> The diagnosis can also be made if there are at least three cases in the family, in which case age is not considered.<ref name="chel"/> |
|||
The [[International Cancer Genome Consortium]] is leading efforts to identify [[genome|genomic]] changes involved in stomach cancer.<ref name="ICGC-USA">{{cite web |url=http://www.icgc.org/icgc/cgp/69/509/70268|title=Gastric Cancer — Adenocarcinoma |publisher=International Cancer Genome Consortium|accessdate=24 February 2014}}</ref><ref name="ICGC-China">{{cite web |url=http://www.icgc.org/icgc/cgp/69/371/811|title=Gastric Cancer — Intestinal- and diffuse-type |publisher=International Cancer Genome Consortium|accessdate=24 February 2014}}</ref> A very small percentage of diffuse-type gastric cancers (see Histopathology below) arise from an [[heredity|inherited]] abnormal ''[[CDH1 (gene)|CDH1]]'' [[gene]]. Genetic testing and treatment options are available for families at risk.<ref name="pmid15235021">{{cite journal | author = Brooks-Wilson AR, Kaurah P, Suriano G, Leach S, Senz J, Grehan N, Butterfield YS, Jeyes J, Schinas J | title = Germline E-cadherin mutations in hereditary diffuse gastric cancer: assessment of 42 new families and review of genetic screening criteria | journal = Journal of Medical Genetics | volume = 41 | issue = 7 | pages = 508–17 | year = 2004 | pmid = 15235021 | pmc = 1735838 | doi = 10.1136/jmg.2004.018275 | last2 = Kaurah | last3 = Suriano | last4 = Leach | last5 = Senz | last6 = Grehan | last7 = Butterfield | last8 = Jeyes | last9 = Schinas | last10 = Bacani | last11 = Kelsey | last12 = Ferreira | last13 = MacGillivray | last14 = MacLeod | last15 = Micek | last16 = Ford | last17 = Foulkes | last18 = Australie | last19 = Greenberg | last20 = Lapointe | last21 = Gilpin | last22 = Nikkel | last23 = Gilchrist | last24 = Hughes | last25 = Jackson | last26 = Monaghan | last27 = Oliveira | last28 = Seruca | last29 = Gallinger | last30 = Caldas | display-authors = 29 }}</ref> |
|||
===Other=== |
|||
Other risks include [[diabetes]],<ref name="pmid24587649">{{cite journal | author = Tseng C-H, Tseng F-H| title = Diabetes and gastric cancer: The potential links | journal = World J Gastroenterol| volume = 20 | issue = 7 | pages = 1701–11 | year = 2014 | pmid = 24587649 | pmc = 3930970 | doi = 10.3748/wjg.v20.i7.1701 | last2 = Tseng }}</ref> |
|||
[[pernicious anemia]],<ref name="pmid24191271"/> chronic atrophic gastritis,<ref name="pmid230756525">{{cite journal | author = Crosby DA, Donohoe CL, Fitzgerald L, Muldoon C, Hayes B, O’Toole D, Reynolds JV | title = Gastric Neuroendocrine Tumours | journal = Digestive Surgery | volume = 29 | issue = 4 | pages = 331–348 | year = 2004 | pmid = 23075625 | doi = 10.1159/000342988 | last2 = Donohoe | last3 = Fitzgerald | last4 = Muldoon | last5 = Hayes | last6 = O'Toole | last7 = Reynolds }}</ref> [[Menetrier's disease]] (hyperplastic, hypersecretory gastropathy),<ref name="pmid15227748">{{cite journal | author = Kim J, Cheong JH, Chen J, Hyung WJ, Choi SH, Noh SH| title = Menetrier's Disease in Korea: Report of Two Cases and Review of Cases in a Gastric Cancer Prevalent Region | journal = Yonsei Medical Journal | volume = 45 | issue = 3 | pages = 555–560 | year = 2004 | pmid = 15227748| url = http://www.eymj.org/Synapse/Data/PDFData/0069YMJ/ymj-45-555.pdf | last2 = Cheong | last3 = Chen | last4 = Hyung | last5 = Choi | last6 = Noh | doi=10.3349/ymj.2004.45.3.555}}</ref> |
|||
and [[intestinal metaplasia]].<ref name="pmid16952033">{{cite journal | author = Tsukamoto T, Mizoshita T, Tatematsu M| title =Gastric-and-intestinal mixed-type intestinal metaplasia: aberrant expression of transcription factors and stem cell intestinalization| journal = Gastric Cancer | volume = 9 | issue = 3 | pages = 156–166 | year = 2006 | pmid = 16952033 |
|||
| doi = 10.1007/s10120-006-0375-6| last2 =Mizoshita| last3 =Tatematsu}}</ref> |
|||
==Diagnosis== |
|||
To find the cause of symptoms, the doctor asks about the patient's medical history, does a physical exam, and may order laboratory studies. The patient may also have one or all of the following exams: |
|||
* [[Gastroscopic exam]] is the diagnostic method of choice. This involves insertion of a [[fibre optic]] camera into the stomach to visualise it.<ref name="pmid24191271"/> |
|||
* [[Upper GI series]] (may be called barium roentgenogram). |
|||
* [[Computed tomography]] or CT scanning of the abdomen may reveal gastric cancer. It is more useful to determine invasion into adjacent tissues or the presence of spread to local lymph nodes. Wall thickening of more than 1 cm that is focal, eccentric and enhancing favours malignancy.<ref>{{cite journal|pmid=22935192|pmc=3458788|year=2012|last1=Virmani|first1=V|last2=Khandelwal|first2=A|last3=Sethi|first3=V|last4=Fraser-Hill|first4=M|last5=Fasih|first5=N|last6=Kielar|first6=A|title=Neoplastic stomach lesions and their mimickers: Spectrum of imaging manifestations|volume=12|pages=269–78|doi=10.1102/1470-7330.2012.0031|journal=Cancer Imaging}}</ref> |
|||
In 2013, Chinese and Israeli scientists reported a successful [[pilot study]] of a [[breathalyzer]]-style breath test intended to diagnose stomach cancer by analyzing exhaled chemicals without the need for an intrusive [[endoscopy]].<ref>{{cite journal |vauthors=Xu ZQ, Broza YY, Ionsecu R |title=A nanomaterial-based breath test for distinguishing gastric cancer from benign gastric conditions |journal=Br. J. Cancer |volume=108 |issue=4 |pages=941–50 |date=March 2013 |pmid=23462808 |pmc=3590679 |doi= 10.1038/bjc.2013.44 |url= http://dx.doi.org/10.1038/bjc.2013.44 |laysummary= http://www.medicalnewstoday.com/articles/257245.php |laysource=Medical News Today {{noitalics|("Breath Test Could Detect and Diagnose Stomach Cancer")}} |laydate=6 March 2013 |display-authors=etal}}</ref> A larger-scale [[clinical trial]] of this technology was completed in 2014.<ref>{{cite journal|title=Detection of precancerous gastric lesions and gastric cancer through exhaled breath|journal=Gut|date=13 April 2015|doi=10.1136/gutjnl-2014-308536|pmid=25869737|volume=65|author=Amal H, Leja M, Funka K, Skapars R, Sivins A, Ancans G, Liepniece-Karele I, Kikuste I, Lasina I, Haick H|pages=400–7}}</ref> |
|||
Abnormal tissue seen in a gastroscope examination will be [[biopsy|biopsied]] by the [[surgery|surgeon]] or [[gastroenterologist]]. This tissue is then sent to a [[pathology|pathologist]] for [[histology|histological]] examination under a microscope to check for the presence of cancerous cells. A biopsy, with subsequent histological analysis, is the only sure way to confirm the presence of cancer cells.<ref name="pmid24191271"/> |
|||
Various gastroscopic modalities have been developed to increase yield of detected mucosa with a dye that accentuates the cell structure and can identify areas of dysplasia. ''Endocytoscopy'' involves ultra-high magnification to visualise cellular structure to better determine areas of dysplasia. Other gastroscopic modalities such as [[optical coherence tomography]] are being tested investigationally for similar applications.<ref>{{cite journal | author = Inoue H, Kudo S-, Shiokawa A | title = Technology Insight: laser-scanning confocal microscopy and endocytoscopy for cellular observation of the gastrointestinal tract | journal = Nature Clinical Practice Gastroenterology & Hepatology | volume = 2 | issue = 1 | pages = 31–7 | year = 2005 | pmid = 16265098 | doi = 10.1038/ncpgasthep0072 | last2 = Kudo | last3 = Shiokawa }}</ref> |
|||
A number of [[cutaneous condition]]s are associated with gastric cancer. A condition of darkened [[hyperplasia]] of the skin, frequently of the [[axilla]] and groin, known as [[acanthosis nigricans]], is associated with intra-abdominal cancers such as gastric cancer. Other cutaneous manifestations of gastric cancer include ''tripe palms'' (a similar darkening hyperplasia of the skin of the palms) and the [[Leser-Trelat sign]], which is the rapid development of skin lesions known as [[seborrheic keratosis|seborrheic keratoses]].<ref name="pmid15230897">{{cite journal | author = Pentenero M, Carrozzo M, Pagano M, Gandolfo S | title = Oral acanthosis nigricans, tripe palms and sign of leser-trelat in a patient with gastric adenocarcinoma | journal = International Journal of Dermatology | volume = 43 | issue = 7 | pages = 530–2 | year = 2004 | pmid = 15230897 | doi = 10.1111/j.1365-4632.2004.02159.x | last2 = Carrozzo | last3 = Pagano | last4 = Gandolfo }}</ref> |
|||
Various blood tests may be done including a [[Complete Blood Count|complete blood count]] (CBC) to check for anaemia, and a [[Fecal occult blood|fecal occult blood test]] to check for blood in the stool. |
|||
===Histopathology=== |
|||
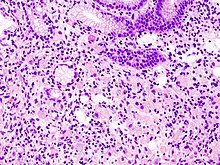
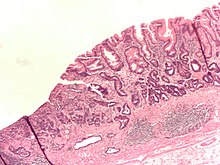
[[File:Adenocarcinoma low differentiated (stomach) H&E magn 400x.jpg|right|thumb|Poor to moderately differentiated adenocarcinoma of the stomach. [[H&E stain]].]] |
|||
[[File:Gastric signet ring cell carcinoma histopatholgy (1).jpg|right|thumb|Gastric signet ring cell carcinoma. [[H&E stain]].]] |
|||
[[File:Gastric adenocarcinoma.jpg|right|thumb|Adenocarcinoma of the stomach and [[intestinal metaplasia]]. [[H&E stain]].]] |
|||
*''Gastric [[adenocarcinoma]]'' is a malignant epithelial tumour, originating from glandular epithelium of the gastric mucosa. Stomach cancers are overwhelmingly [[adenocarcinomas]] (90%).<ref>{{cite book |last=Kumar |title=Pathologic Basis of Disease |edition=8th |page=784 |publisher=Saunders Elsevier |year=2010 |isbn=978-1-4160-3121-5 |ref=harv|display-authors=etal}}</ref> Histologically, there are two major types of gastric adenocarcinoma (Lauren classification): intestinal type or diffuse type. Adenocarcinomas tend to aggressively invade the gastric wall, infiltrating the [[muscularis mucosae]], the submucosa and thence the muscularis propria. Intestinal type adenocarcinoma tumour cells describe irregular tubular structures, harbouring pluristratification, multiple lumens, reduced stroma ("back to back" aspect). Often, it associates intestinal metaplasia in neighbouring mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiated. [[Linitis plastica|Diffuse type]] adenocarcinoma (mucinous, colloid, linitis plastica, leather-bottle stomach) tumour cells are discohesive and secrete mucus, which is delivered in the interstitium, producing large pools of mucus/colloid (optically "empty" spaces). It is poorly differentiated. If the mucus remains inside the tumour cell, it pushes the nucleus to the periphery: "''[[signet-ring cell]]''". |
|||
* Around 5% of gastric malignancies are [[lymphomas]] (MALTomas, or [[MALT lymphoma]]).<ref>{{harvnb|Kumar|2010|p=786}}</ref> |
|||
* [[Carcinoid]] and stromal tumors may occur. |
|||
===Staging=== |
|||
[[File:Diagram showing the T stages of stomach cancer CRUK 374.svg|thumb|left|T stages of stomach cancer]] |
|||
If cancer cells are found in the tissue sample, the next step is to [[cancer staging|stage]], or find out the extent of the disease. Various tests determine whether the cancer has spread and, if so, what parts of the body are affected. Because stomach cancer can spread to the liver, the pancreas, and other organs near the stomach as well as to the lungs, the doctor may order a [[CT scan]], a [[PET scan]],<ref name="pmid16418249">{{cite journal | author =Lim JS, Yun MJ, Kim MJ, Hyung WJ, Park MS, Choi JY, Kim TS, Lee JD, Noh SH, Kim KW| title = CT and PET in stomach cancer: preoperative staging and monitoring of response to therapy | journal = Radiographics | volume = 26 | issue = 1| pages = 143–156 | year = 2006 | pmid = 16418249 | doi = 10.1148/rg.261055078 | last2 = Yun | last3 = Kim | last4 = Hyung | last5 = Park | last6 = Choi | last7 = Kim | last8 = Lee | last9 = Noh | last10 = Kim }}</ref> an [[endoscopic ultrasound]] exam, or other tests to check these areas. Blood tests for [[tumor marker]]s, such as [[carcinoembryonic antigen]] (CEA) and carbohydrate antigen (CA) may be ordered, as their levels correlate to extent of metastasis, especially to the liver, and the cure rate. |
|||
Staging may not be complete until after surgery. The surgeon removes nearby lymph nodes and possibly samples of tissue from other areas in the abdomen for examination by a pathologist. |
|||
The clinical stages of stomach cancer are:<ref>{{cite web|url=http://www.cancer.org/docroot/cri/content/cri_2_4_4x_treatment_choices_by_type_and_stage_of_stomach_cancer_40.asp|title=Detailed Guide: Stomach Cancer Treatment Choices by Type and Stage of Stomach Cancer|date=2009-11-03|publisher=American Cancer Society}}</ref><ref>{{cite web|url=http://www.ehealthmd.com/library/stomachcancer/STC_stages.html|title=What Are The Stages Of Stomach Cancer?|author=Guy Slowik|date=October 2009|publisher=ehealthmd.com}}</ref> |
|||
* '''Stage 0.''' Limited to the inner lining of the stomach. Treatable by endoscopic mucosal resection when found very early (in routine screenings); otherwise by [[gastrectomy]] and [[lymphadenectomy]] without need for chemotherapy or radiation. |
|||
* '''Stage I.''' Penetration to the second or third layers of the stomach '''(Stage 1A)''' or to the second layer and nearby [[lymph nodes]] '''(Stage 1B)'''. Stage 1A is treated by surgery, including removal of the [[Greater omentum|omentum]]. Stage 1B may be treated with chemotherapy ([[5-fluorouracil]]) and radiation therapy. |
|||
* '''Stage II.''' Penetration to the second layer and more distant lymph nodes, or the third layer and only nearby lymph nodes, or all four layers but not the lymph nodes. Treated as for Stage I, sometimes with additional [[Adjuvant chemotherapy#Neoadjuvant therapy|neoadjuvant chemotherapy]]. |
|||
* '''Stage III.''' Penetration to the third layer and more distant lymph nodes, or penetration to the fourth layer and either nearby tissues or nearby or more distant lymph nodes. Treated as for Stage II; a cure is still possible in some cases. |
|||
* '''Stage IV.''' Cancer has spread to nearby tissues and more distant lymph nodes, or has [[metastasize]]d to other organs. A cure is very rarely possible at this stage. Some other techniques to prolong life or improve symptoms are used, including laser treatment, surgery, and/or stents to keep the digestive tract open, and chemotherapy by drugs such as 5-fluorouracil, [[cisplatin]], [[epirubicin]], [[etoposide]], [[docetaxel]], [[oxaliplatin]], [[capecitabine]] or [[irinotecan]]. |
|||
[[File:Diagram showing secondary stomach cancer in the lungs CRUK 186.svg|thumb|right|Stomach cancer metastasized to the lungs]] |
|||
The [[TNM staging system]] is also used.<ref>{{cite web|url=http://www.cancer.org/docroot/CRI/content/CRI_2_4_3X_How_is_stomach_cancer_staged_40.asp?sitearea=|title=Detailed Guide: Stomach Cancer: How Is Stomach Cancer Staged?|publisher=American Cancer Society}}</ref> |
|||
In a study of open-access endoscopy in [[Scotland]], patients were diagnosed 7% in Stage I 17% in Stage II, and 28% in Stage III.<ref>{{cite journal | author = Paterson HM, McCole D, Auld CD | title = Impact of open-access endoscopy on detection of early oesophageal and gastric cancer 1994–2003: population-based study | journal = Endoscopy | volume = 38 | issue = 5 | pages = 503–7 | year = 2006 | pmid = 16767587 | doi = 10.1055/s-2006-925124 | last2 = McCole | last3 = Auld }}</ref> A Minnesota population was diagnosed 10% in Stage I, 13% in Stage II, and 18% in Stage III.<ref>{{cite journal | author = Crane SJ, Locke GR, Harmsen WS, Zinsmeister AR, Romero Y, Talley NJ | title = Survival Trends in Patients With Gastric and Esophageal Adenocarcinomas: A Population-Based Study | journal = Mayo Clinic Proceedings | volume = 83 | issue = 10 | pages = 1087–94 | year = 2008 | pmid = 18828967 | pmc = 2597541 | doi = 10.4065/83.10.1087 | last2 = Locke Gr | last3 = Harmsen | last4 = Zinsmeister | last5 = Romero | last6 = Talley }}</ref> However, in a high-risk population in the [[Valdivia Province]] of southern [[Chile]], only 5% of patients were diagnosed in the first two stages and 10% in stage III.<ref name=Valdivia>{{cite journal | author = Heise K, Bertran E, Andia ME, Ferreccio C | title = Incidence and survival of stomach cancer in a high-risk population of Chile | journal = World Journal of Gastroenterology | volume = 15 | issue = 15 | pages = 1854–62 | year = 2009 | pmid = 19370783 | pmc = 2670413 | doi = 10.3748/wjg.15.1854 | last2 = Bertran | last3 = Andia | last4 = Ferreccio }}</ref> |
|||
==Prevention== |
|||
Getting rid of ''[[H. pylori]]'' in those who are infected decreases the risk of stomach cancer, at least in those who are Asian.<ref>{{cite journal|last=Ford|first=AC|author2=Forman, D |author3=Hunt, RH |author4=Yuan, Y |author5= Moayyedi, P |title=Helicobacter pylori eradication therapy to prevent gastric cancer in healthy asymptomatic infected individuals: systematic review and meta-analysis of randomised controlled trials.|journal=BMJ |date=20 May 2014|volume=348|pages=g3174|pmid=24846275 |pmc=4027797 |doi=10.1136/bmj.g3174}}</ref> A 2014 meta-analysis of observational studies found that a diet high in [[fruit]]s, [[Edible mushroom|mushrooms]], [[garlic]], [[soybean]]s, and [[green onion]]s was associated with a lower risk of stomach cancer in the Korean population.<ref name=Woo2014>{{cite journal|vauthors=Woo HD, Park S, Oh K, Kim HJ, Shin HR, Moon HK, Kim J |title=Diet and cancer risk in the Korean population: a meta- analysis|journal=Asian Pacific Journal of Cancer Prevention |volume=15|issue=19|pages=8509–19|date=2014|pmid=25339056|url=http://www.apocpcontrol.org/paper_file/issue_abs/Volume15_No19/8509-8519%208.13%20Hae%20Dong%20Woo%20RKFH3.pdf|doi=10.7314/apjcp.2014.15.19.8509}}</ref> Low doses of [[vitamin]]s, especially from a [[healthy diet]], decrease the risk of stomach cancer.<ref>{{cite journal|last1=Kong|first1=P|last2=Cai|first2=Q|last3=Geng|first3=Q|last4=Wang|first4=J|last5=Lan|first5=Y|last6=Zhan|first6=Y|last7=Xu|first7=D|title=Vitamin intake reduce the risk of gastric cancer: meta-analysis and systematic review of randomized and observational studies.|journal=PLOS ONE|date=2014|volume=9|issue=12|pages=e116060|doi=10.1371/journal.pone.0116060|pmid=25549091|pmc=4280145}}</ref> A previous review of [[antioxidant]] supplementation did not find supporting evidence and possibly worse outcomes.<ref>{{cite journal|last1=Bjelakovic|first1=G|last2=Nikolova|first2=D|last3=Simonetti|first3=RG|last4=Gluud|first4=C|title=Antioxidant supplements for preventing gastrointestinal cancers.|journal=Cochrane Database of Systematic Reviews|date=16 July 2008|issue=3|pages=CD004183|pmid=18677777|doi=10.1002/14651858.CD004183.pub3}}</ref><ref>{{cite journal|last1=Bjelakovic|first1=G|last2=Nikolova|first2=D|last3=Gluud|first3=LL|last4=Simonetti|first4=RG|last5=Gluud|first5=C|title=Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases.|journal=Cochrane Database of Systematic Reviews|date=14 March 2012|volume=3|pages=CD007176|pmid=22419320|doi=10.1002/14651858.CD007176.pub2}}</ref> |
|||
==Management== |
|||
Cancer of the stomach is difficult to cure unless it is found at an early stage (before it has begun to spread). Unfortunately, because early stomach cancer causes few symptoms, the disease is usually advanced when the diagnosis is made.<ref name="pmid23639645">{{cite journal| author=Roopma Wadhwa, Takashi Taketa, Kazuki Sudo, Mariela A. Blum, Jaffer A. Ajani| title=Modern Oncological Approaches to Gastric Adenocarcinoma | journal=Gastroenterology Clinics of North America| year= 2013 | volume= 42 | issue= 2 | pages= 359–369 | pmid=23639645 | doi=10.1016/j.gtc.2013.01.011| last2=Taketa | last3=Sudo | last4=Blum | last5=Ajani }}</ref> |
|||
Treatment for stomach cancer may include surgery,<ref name="pmid23983442">{{cite journal| author=Ke Chen, Xiao-Wu Xu, Ren-Chao Zhang, Yu Pan, Di Wu, Yi-Ping Mou| title=Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer| journal=World J Gastroenterol| year= 2013 | volume= 19 | issue= 32 | pages= 5365–76 | pmid=23983442 | pmc=3752573| doi=10.3748/wjg.v19.i32.5365| last2=Xu| last3=Zhang| last4=Pan| last5=Wu| last6=Mou}}</ref> [[chemotherapy]], and/or [[radiation therapy]].<ref name="pmid23622077">{{cite journal| author=Jennifer L. Pretz, Jennifer Y. Wo, Harvey J. Mamon, Lisa A. Kachnic, Theodore S. Hong| title=Chemoradiation Therapy: Localized Esophageal, Gastric, and Pancreatic Cancer | journal=Surgical Oncology Clinics of North America | year= 2011 | volume= 22 | issue= 3 | pages= 511–524 | pmid=23622077 | doi=10.1016/j.soc.2013.02.005| last2=Wo | last3=Mamon | last4=Kachnic | last5=Hong }}</ref> New treatment approaches such as [[biological therapy]] and improved ways of using current methods are being studied in clinical trials.<ref name="pmid21556317">{{cite journal| author=Judith Meza-Junco, Heather-Jane Au, Michael B Sawyer| title=Critical appraisal of trastuzumab in treatment of advanced stomach cancer | journal=Cancer Management and Research | year= 2011 | volume= 3 | pages= 57–64 | pmid=21556317 | pmc=3085240 | doi=10.2147/CMAR.S12698| last2=Au | last3=Sawyer }}</ref> |
|||
===Surgery=== |
|||
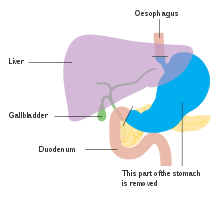
[[File:Diagam showing the anatomy before Roux-en-y surgery for stomach cancer CRUK 002.svg|thumb|right|Anatomy before Roux-en-y surgery to resect stomach cancer.]] |
|||
Surgery remains the only curative therapy for stomach cancer.<ref name = WJG14/> Of the different surgical techniques, [[endoscopic mucosal resection]] (EMR) is a treatment for early gastric cancer (tumor only involves the [[mucosa]]) that was pioneered in Japan and is available in the United States at some centers.<ref name = WJG14/> In this procedure, the tumor, together with the inner lining of stomach (mucosa), is removed from the wall of the stomach using an electrical wire loop through the endoscope. The advantage is that it is a much smaller operation than removing the stomach.<ref name = WJG14/> [[endoscopy|Endoscopic submucosal dissection]] (ESD) is a similar technique pioneered in Japan, used to resect a large area of mucosa in one piece.<ref name = WJG14/> If the pathologic examination of the resected specimen shows incomplete resection or deep invasion by tumor, the patient would need a formal stomach resection.<ref name = WJG14/> A 2016 [[Cochrane review]] found low quality evidence of no difference in short-term mortality between laparoscopic and open gastrectomy (removal of stomach), and that benefits or harms of laparoscopic gastrectomy cannot be ruled out.<ref>{{cite journal|last1=Best|first1=LM|last2=Mughal|first2=M|last3=Gurusamy|first3=KS|title=Laparoscopic versus open gastrectomy for gastric cancer.|journal=The Cochrane database of systematic reviews|date=31 March 2016|volume=3|pages=CD011389|doi=10.1002/14651858.CD011389.pub2|pmid=27030300|url=http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011389.pub2/full|accessdate=5 April 2016}}</ref> |
|||
Those with metastatic disease at the time of presentation may receive palliative surgery and while it remains controversial, due to the possibility of complications from the surgery itself and the fact that it may delay chemotherapy the data so far is mostly positive, with improved survival rates being seen in those treated with this approach.<ref name = WJG14/><ref>{{cite journal|last=Sun|first=J|author2=Song, Y |author3=Wang, Z |author4=Chen, X |author5=Gao, P |author6=Xu, Y |author7=Zhou, B |author8= Xu, H |title=Clinical significance of palliative gastrectomy on the survival of patients with incurable advanced gastric cancer: a systematic review and meta-analysis.|journal=BMC Cancer|date=December 2013|volume=13|page=577|doi=10.1186/1471-2407-13-577|pmid=24304886|url=http://www.biomedcentral.com/content/pdf/1471-2407-13-577.pdf|format=PDF |issue=1}}</ref> |
|||
===Chemotherapy=== |
|||
The use of [[chemotherapy]] to treat stomach cancer has no firmly established [[standard of care]]. Unfortunately, stomach cancer has not been particularly sensitive to these drugs, and chemotherapy, if used, has usually served to palliatively reduce the size of the tumor, relieve symptoms of the disease and increase survival time. Some drugs used in stomach cancer treatment have included: [[5-FU]] (fluorouracil) or its analog [[capecitabine]], BCNU ([[carmustine]]), methyl-CCNU ([[semustine]]) and [[doxorubicin]] (Adriamycin), as well as [[mitomycin C]], and more recently [[cisplatin]] and [[taxotere]], often using drugs in various combinations. The relative benefits of these different drugs, alone and in combination, are unclear.<ref name="pmid17425475">{{cite journal | author = Scartozzi M, Galizia E, Verdecchia L, Berardi R, Antognoli S, Chiorrini S, Cascinu S | title = Chemotherapy for advanced gastric cancer: across the years for a standard of care | journal = Expert Opinion on Pharmacotherapy | volume = 8 | issue = 6 | pages = 797–808 | year = 2007 | pmid = 17425475 | doi = 10.1517/14656566.8.6.797 | last2 = Galizia | last3 = Verdecchia | last4 = Berardi | last5 = Antognoli | last6 = Chiorrini | last7 = Cascinu }}</ref> Clinical researchers are exploring the benefits of giving chemotherapy before surgery to shrink the tumor, or as adjuvant therapy after surgery to destroy remaining cancer cells.<ref name = WJG14/> |
|||
===Targeted therapy=== |
|||
Recently, treatment with [[HER2/neu|human epidermal growth factor receptor 2 (''HER2'')]] inhibitor, [[trastuzumab]], has been demonstrated to increase [[Overall survival rate|overall survival]] in inoperable locally advanced or metastatic gastric carcinoma over-expressing the [[HER2/neu]] gene.<ref name="WJG14" /> In particular, ''[[HER2/neu|HER2]]'' is overexpressed in 13-22% of patients with gastric cancer.<ref name="pmid21556317" /><ref name=":0">{{Cite journal|url = http://www.nature.com/modpathol/journal/v26/n6/full/modpathol2012228a.html|title = HER2 in gastric cancer: a digital image analysis in pre-neoplastic, primary and metastatic lesions|vauthors=Fusco N, Rocco EG, Del Conte C, Pellegrini C, Bulfamante G, Di Nuovo F, Romagnoli S, Bosari S |date = Jun 2013|journal = Mod Pathol|doi = 10.1038/modpathol.2012.228|pmid = 23348899|access-date = |volume = 26|issue = 6|pages = 816–24}}</ref> Of note, ''HER2'' overexpression in gastric neoplasia is heterogeneous and comprises a minority of tumor cells (less than 10% of gastric cancers overexpress ''HER2'' in more than 5% of tumor cells). Hence, this heterogeneous expression should be taken into account for ''HER2'' testing, particularly in small samples such as biopsies, requiring the evaluation of more than one bioptic sample.<ref name=":0" /> |
|||
===Radiation=== |
|||
[[Radiation therapy]] (also called radiotherapy) may be used to treat stomach cancer, often as an adjuvant to chemotherapy and/or surgery.<ref name = WJG14/> |
|||
==Prognosis== |
|||
The prognosis of stomach cancer is generally poor, due to the fact the tumour has often metastasised by the time of discovery and the fact that most people with the condition are elderly (median age is between 70 and 75 years) at presentation.<ref name = MSR>{{cite web|title=Gastric Cancer|work=Medscape Reference|publisher=WebMD|accessdate=4 April 2014|url=http://emedicine.medscape.com/article/278744-overview#showall|author1=Cabebe, EC |author2=Mehta, VK |author3=Fisher, G, Jr |editor1=Talavera, F |editor2=Movsas, M |editor3=McKenna, R |editor4=Harris, JE |date=21 January 2014}}</ref> The five-year survival rate for stomach cancer is reported to be less than 10 percent.<ref name = WJG14/> |
|||
==Epidemiology== |
|||
[[File:Stomach cancer world map-Deaths per million persons-WHO2012.svg|thumb|upright=1.3|Stomach cancer deaths per million persons in 2012 |
|||
{{refbegin|3}}{{legend|#ffff20|0–11}}{{legend|#ffe820|12–16}}{{legend|#ffd820|17–24}}{{legend|#ffc020|25–33}}{{legend|#ffa020|34–51}}{{legend|#ff9a20|52–76}}{{legend|#f08015|77–102}}{{legend|#e06815|103–128}}{{legend|#d85010|129–175}}{{legend|#d02010|176–400}}{{refend}}]] |
|||
Worldwide, stomach cancer is the fifth most common cancer with 952,000 cases diagnosed in 2012.<ref name=WCR2014Epi/> It is more common in men and in developing countries.<ref name="Parkin">{{cite journal | author = Parkin DM, Bray F, Ferlay J, Pisani P | title = Global Cancer Statistics, 2002 | journal = CA: A Cancer Journal for Clinicians | volume = 55 | issue = 2 | pages = 74–108 | year = 2005 | pmid = 15761078 | doi = 10.3322/canjclin.55.2.74 | last2 = Bray | last3 = Ferlay | last4 = Pisani }}</ref><ref name="WHO-QA15">{{cite web|url=http://www.who.int/features/qa/15/en/index.html |title=Are the number of cancer cases increasing or decreasing in the world? |date=1 April 2008 |work=WHO Online Q&A |publisher=WHO |accessdate=2009-05-11}}</ref> In 2012, it represented 8.5% of cancer cases in men, making it the fourth most common cancer in men.<ref>{{cite book |title = World Cancer Report 2014 |publisher = International Agency for Research on Cancer, World Health Organization |date = 2014 |isbn = 978-92-832-0432-9}}</ref> In 2012 number of deaths were 700,000 having decreased slightly from 774,000 in 1990 making it the third leading cause of cancer death after [[lung cancer]] and [[liver cancer]].<ref name=Loz2012>{{cite journal|last=Lozano|first=R|title=Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010|journal=Lancet|date=15 December 2012|volume=380|issue=9859|pages=2095–128|pmid=23245604|doi=10.1016/S0140-6736(12)61728-0|first2=M|last3=Foreman|first3=K|last4=Lim|first4=S|last5=Shibuya|first5=K|last6=Aboyans|first6=V|last7=Abraham|first7=J|last8=Adair|first8=T|last9=Aggarwal|first9=R|last10=Ahn|first10=SY|last11=Alvarado|first11=M|last12=Anderson|first12=HR|last13=Anderson|first13=LM|last14=Andrews|first14=KG|last15=Atkinson|first15=C|last16=Baddour|first16=LM|last17=Barker-Collo|first17=S|last18=Bartels|first18=DH|last19=Bell|first19=ML|last20=Benjamin|first20=EJ|last21=Bennett|first21=D|last22=Bhalla|first22=K|last23=Bikbov|first23=B|last24=Bin Abdulhak|first24=A|last25=Birbeck|first25=G|last26=Blyth|first26=F|last27=Bolliger|first27=I|last28=Boufous|first28=S|last29=Bucello|first29=C|last30=Burch|first30=M|last2=Naghavi|display-authors=29}}</ref><ref>{{cite web|title=PRESS RELEASE N° 224 Global battle against cancer won’t be won with treatment alone: Effective prevention measures urgently needed to prevent cancer crisis|url=http://www.iarc.fr/en/media-centre/pr/2014/pdfs/pr224_E.pdf|work=World Health Organization|accessdate=14 March 2014|date=3 February 2014}}</ref> |
|||
Less than 5% of stomach cancers occur in people under 40 years of age with 81.1% of that 5% in the age-group of 30 to 39 and 18.9% in the age-group of 20 to 29.<ref>{{cite journal | title = Gastric Cancer in Young Adults | journal = Revista Brasileira de Cancerologia | volume = 46 | issue = 3 | pages = |date=Jul 2000 | pmid = | doi = | url = http://www.inca.gov.br/rbc/n_46/v03/english/article6.html }}</ref> |
|||
In 2014, stomach cancer accounted for 0.61% of deaths (13,303 cases) in the United States.<ref>{{cite web |url=http://www.worldlifeexpectancy.com/country-health-profile/united-states|title=Health profile: United States|publisher=Le Duc Media |accessdate=31 Jan 2016}}</ref> In China, stomach cancer accounted for 3.56% of all deaths (324,439 cases).<ref>{{cite web |url=http://www.worldlifeexpectancy.com/country-health-profile/china|title=Health profile: China|publisher=Le Duc Media |accessdate=31 Jan 2016}}</ref> The highest rate of stomach cancer was in [[Mongolia]], at 28 cases per 100,000 people.<ref>{{cite web |url=http://www.worldlifeexpectancy.com/cause-of-death/stomach-cancer/by-country/|title=Stomach Cancer: Death Rate Per 100,000 |publisher=Le Duc Media |accessdate=13 March 2014}}</ref> |
|||
In the United Kingdom, stomach cancer is the fifteenth most common cancer (around 7,100 people were diagnosed with stomach cancer in 2011), and it is the tenth most common cause of cancer death (around 4,800 people died in 2012).<ref>{{cite web|title=Stomach cancer statistics|url=http://www.cancerresearchuk.org/cancer-info/cancerstats/types/stomach/|website=Cancer Research UK|accessdate=28 October 2014}}</ref> |
|||
Incidence and mortality rates of gastric cancer vary greatly in Africa. The GLOBOCAN system is currently the most widely used method to compare these rates between countries, but African incidence and mortality rates are seen to differ among countries possibly due to the lack of universal access to a registry system for all countries.<ref name="asom">{{cite journal |author1=Asombang Akwi W |author2=Rahman Rubayat |author3=Ibdah Jamal A | title = Gastric cancer in Africa: Current management and outcomes | journal = World Journal of Gastroenterology | volume = 20 | pages = 3875–79 |date=2014 | doi=10.3748/wjg.v20.i14.3875 | pmid=24833842 | pmc=3983443}}</ref> Variation as drastic as estimated rates from 0.3/100000 in Botswana to 20.3/100000 in Mali have been observed.<ref name="asom"/> In Uganda, the incidence of gastric cancer has increased from the 1960s measurement of 0.8/100000 to 5.6/100000.<ref name="asom"/> Gastric cancer, though present, is relatively low when compared to countries with high incidence like Japan or China. One suspected cause of the variation within Africa and between other countries is due to different strains of the Helicobacter pylori bacteria. The trend commonly seen is that H. pylori infection increases the risk for gastric cancer, however this is not the case in Africa giving this phenomenon the name the “African enigma.”<ref name="louw">{{cite journal |author1=Louw J. A. |author2=Kidd M. S. G. |author3=Kummer A. F. |author4=Taylor K. |author5=Kotze U. |author6=Hanslo D. | title = The relationship between helicobacter pylori infection, the virulence genotypes of the infecting strain and gastric cancer in the African setting | journal = Helicobacter | volume = 6 | issue = 4 | pages = 268–73 |date= November 2001 | doi=10.1046/j.1523-5378.2001.00044.x}}</ref> Although this bacteria is found in Africa, evidence has supported that different strains with mutations in the bacterial genotype may contribute to the difference in cancer development between African countries and others outside of the continent.<ref name="louw"/> However, increasing access to health care and treatment measures have been commonly associated with the rising incidence, particularly in Uganda.<ref name="asom"/> |
|||
==Other animals== |
|||
The [[stomach]] is a muscular organ of the [[gastrointestinal]] tract that holds food and begins the digestive process by secreting gastric juice. The most common cancers of the stomach are [[adenocarcinomas]] but other histological types have been reported. Signs vary but may include vomiting (especially if blood is present), weight loss, anemia, and lack of appetite. Bowel movements may be dark and tarry in nature. In order to determine whether cancer is present in the stomach, special X-rays and/or abdominal ultrasound may be performed. [[Gastroscopy]], a test using an instrument called endoscope to examine the stomach, is a useful diagnostic tool that can also take samples of the suspected mass for histopathological analysis to confirm or rule out cancer. The most definitive method of cancer diagnosis is through open surgical biopsy.<ref name=MacEwan_2001>{{cite book|veditors=Withrow SJ, MacEwen EG |title=Small Animal Clinical Oncology|edition=3rd|publisher=W.B. Saunders |year=2001}}</ref> Most stomach tumors are malignant with evidence of spread to lymph nodes or liver, making treatment difficult. Except for lymphoma, surgery is the most frequent treatment option for stomach cancers but it is associated with significant risks. |
|||
== 參考資料 == |
== 參考資料 == |
||
| 第101行: | 第229行: | ||
{{消化系统肿瘤}} |
{{消化系统肿瘤}} |
||
{{Gram-negative proteobacterial diseases}} |
{{Gram-negative proteobacterial diseases}} |
||
{{Digestive system neoplasia}} |
|||
{{Use dmy dates|date=September 2010}} |
|||
{{DEFAULTSORT:Stomach Cancer}} |
|||
[[Category:Stomach cancer| ]] |
|||
[[Category:Abdomen]] |
|||
[[Category:Epstein–Barr virus-associated diseases]] |
|||
[[Category:Infectious causes of cancer]] |
|||
[[Category:RTT]] |
|||
{{Authority control}} |
{{Authority control}} |
||
[[Category:癌症]] |
[[Category:癌症]] |
||
2017年5月16日 (二) 20:00的版本
此條目目前正依照其他维基百科上的内容进行翻译。 (2017年5月16日) |
| 胃癌(Stomach cancer) | |
|---|---|
 | |
| 一個經切片檢體檢查後確認為癌症的胃潰瘍部位(切除後)(A stomach ulcer that was diagnosed as cancer on biopsy and surgically removed.) | |
| 类型 | 胃腸癌、stomach neoplasm[*]、胃部疾病[*]、疾病 |
| 分类和外部资源 | |
| 醫學專科 | Oncology |
| ICD-11 | 2B72 |
| ICD-10 | C16 |
| ICD-9-CM | 151 |
| OMIM | 137215 |
| DiseasesDB | 12445 |
| MedlinePlus | 000223 |
| eMedicine | med/845 |
| MeSH | D013274 |
| GeneReviews | |
| Orphanet | 63443 |
胃癌(Stomach cancer、gastric cancer)是發生在胃部黏膜的癌症[1]。 Early symptoms may include heartburn, upper abdominal pain, nausea and loss of appetite. Later signs and symptoms may include weight loss, yellowing of the skin and whites of the eyes, vomiting, difficulty swallowing, and blood in the stool among others.[2] The cancer may spread from the stomach to other parts of the body, particularly the liver, lungs, bones, lining of the abdomen and lymph nodes.[3] The most common cause is infection by the bacterium Helicobacter pylori, which accounts for more than 60% of cases.[4][5][6] Certain types of H. pylori have greater risks than others. Other common causes include eating pickled vegetables and smoking. About 10% of cases run in families and between 1% and 3% of cases are due to genetic syndromes inherited from a person's parents such as hereditary diffuse gastric cancer. Most cases of stomach cancers are gastric carcinomas. This type can be divided into a number of subtypes. Lymphomas and mesenchymal tumors may also develop in the stomach. Most of the time, stomach cancer develops in stages over years.[5] Diagnosis is usually by biopsy done during endoscopy. This is followed by medical imaging to determine if the disease has spread to other parts of the body.[2] Japan and South Korea, two countries that have high rates of the disease, screen for stomach cancer.[5] 地中海式飲食和戒煙都能降低罹患胃癌的風險。有研究顯示,治療胃幽門桿菌也有可能可以降低未來罹患胃癌的風險 There is tentative evidence that treating H. pylori decreases the future risk.[5][7] 如果胃癌能夠早期治療,多數能夠痊癒[5]。 治療方式包括:外科手術、化學治療、放射線治療以及標靶治療[2]。 若到了疾病的末期,則可以考慮緩和療法[5]。 胃癌的治療成效不佳,全球平均的五年存活率在10%以下。這主要是因為多數患者都在疾病已相當嚴重時才發現罹癌[8]。 在美國,五年存活率為28%[9],而在南韓五年存活率可達65%,致力於胃癌篩檢可能是存活率較高的原因之一[5]。 全世界中,胃癌是癌症致病原因第五名,並且在癌症致死率排名中為第三名,分別占7%與9%的個案數[10]。 在2012年中,有 950,000人發病,且723,000 人死亡[10]。在1930年代以前,胃癌是世界許多地區(包含美國和英國)最常見的癌症死因[11][12][13] ,但後來各個地區的胃癌死亡率皆已下降[5] 一般認為和發明冰箱,因此人們使用鹽漬法來保存食物的比例降低有關[14]。胃癌最普遍發生於東亞以及東歐地區,並且男性發病的機率是女性的兩倍[5]。
前兆與症狀(Signs and symptoms)

Stomach cancer is often either asymptomatic (producing no noticeable symptoms) or it may cause only nonspecific symptoms (symptoms that are specific to stomach cancer and to other related or unrelated disorders) in its early stages. By the time symptoms occur, the cancer has often reached an advanced stage (see below) and may have metastasized (spread to other, perhaps distant, parts of the body), which is one of the main reasons for its relatively poor prognosis.[15] Stomach cancer can cause the following signs and symptoms:
Early cancers may be associated with indigestion or a burning sensation (heartburn). However, less than 1 in every 50 people referred for endoscopy due to indigestion has cancer.[16] Abdominal discomfort and loss of appetite, especially for meat, can occur.
Gastric cancers that have enlarged and invaded normal tissue can cause weakness, fatigue, bloating of the stomach after meals, abdominal pain in the upper abdomen, nausea and occasional vomiting, diarrhea or constipation. Further enlargement may cause weight loss or bleeding with vomiting blood or having blood in the stool, the latter apparent as black discolouration (melena) and sometimes leading to anemia. Dysphagia suggests a tumour in the cardia or extension of the gastric tumour into the esophagus.
These can be symptoms of other problems such as a stomach virus, gastric ulcer, or tropical sprue.
簡介
大多數的胃部腫瘤都是腺癌大約佔99%,大致上又可再分為淋巴瘤與間質瘤。大多時候胃癌會經年累月地持續惡化[5]。根據世界衛生組織估計,胃癌是全世界排名第四個最普遍被診斷的癌症,而且是所有癌症死亡率排名第二高,被視為國際間重要的健康危機。胃癌的高發生率包括東亞、南美洲和東歐國家。在台灣地區,胃癌發生率尤其偏高,每100,000人口約有8.52人至9.68人,胃癌名列2006年癌症死亡原因第5位,約有2500人死於胃癌,每100,000人口死亡率為11.4% ,但胃癌若是極早期僅在表面型的五年存活率幾乎接近95%以上,而一旦擴散存活率會急降是其特性。
食用醃漬蔬菜、黴變、煙燻、油炸食物與抽菸公認是主要強因素。最常見的輔助原因是因為感染幽門螺旋桿菌,將近六成的胃部腫瘤患者都檢查出感染這種細菌[17][5]但並非唯一因素只是相關因素,某些種的幽門螺旋桿菌較為其他種來的危險。另大約有10%的病例與家族遺傳有關,大概有1%~3%的的案例是因為源自雙親的基因性疾病,像是遺傳性瀰漫性胃癌。大多經由胃鏡採檢樣本來做診斷,確診後才會再經由醫學影像,確認是否轉移到其他地方[2]。日本與南韓兩國胃癌的比率較高,會進行胃癌篩檢來發現疾病[5]。
早期的症狀包括胃灼熱,上腹疼痛,惡心及食慾不振。症狀與消化性潰瘍類似,是導致延誤就醫與高死亡率的原因,但其痛感與潰瘍還是有些許差異,胃潰瘍是食後痛而十二指腸潰瘍是空腹痛,但胃癌通常不受進食的明顯規律影響,且其痛感是一種咬合性疼痛並且制酸劑不能解除痛感,然而還是有較少數胃癌痛感會受進食有些許影響並且制酸劑能稍微緩解,導致診斷更難,所以說胃鏡還是唯一有效直接的診斷方法。而胃鏡中有一明顯區別方法就是十二指腸潰瘍的病灶極不可能是胃癌,因其成因是胃酸過強,反而有助殺滅很多產生亞硝酸類的細菌所以極少癌變,同時臨床上極稀少胃癌蔓延至十二指腸區域。但是胃潰瘍和胃癌就較難分辨很多時候只能靠切片,同時經驗較少的醫生也有誤判可能,而胃潰瘍成因是為胃酸過少和黏膜防禦力弱造成亞硝酸類的細菌孳生,這也可以視為一種有邏輯關係的癌前因子。
晚期的症狀包括體重減輕,黃疸,嘔吐,難以吞嚥,糞便中有血等症狀[2]。癌細胞會擴散到其他部位,特別是肝,肺,腹膜及淋巴結等部位[18]。
分類
胃癌的分類可分為早期胃癌及進行性胃癌,臨床表現症狀則是模糊且不具特異性。大部份診斷出胃癌的病人被發現時都已經是進行性疾病來呈現。統計發現超過50%的病人會進行手術,但是手術之後,大約60-70%的病人發生轉移。轉移性的胃癌仍然是一種無法治癒的疾病。一般而言,胃癌病人平均五年的存活率大約22%左右,而晚期胃癌患者的五年的存活率更小於5%以下。化學療法已經成為胃癌治療不可缺少的方法之一,緩和的化學療法已經被證明能提高存活率或末期生活品質。
另有一種普通非癌的胃手術後20年左右可能產生的殘胃癌現象。
引發原因 (Causes)
一般醫學上所謂的「危險因子」是指任何會增加得到某疾病的機會的「事物」。雖然大多數癌症的形成原因,至今仍不十分明瞭,它可能是由許多因子,經過許多過程逐步轉變而來的,對不同癌症而言,則也有不同「事物」會增加其癌變發生的機會。譬如吸煙的人較容易得到肺癌,咽喉癌較大。
目前所知的胃癌危險因子主要與生活環境、飲食習慣、遺傳與免疫因素以及慢性胃病...等有關。例如環境中的致癌因子經年累月後可能導致胃黏膜變性而造成癌,或者個人對環境的致癌物敏感度較低有關。常見的胃癌「危險因子」如下:
遺傳:胃癌的家庭歷史,家族內有血親罹患胃癌,則其它人得胃癌的機會比一般人多2-3倍。但仍有疑義,因這些人增加胃癌機會可能是由於有較相似的生活環境與飲食習慣。
性別:已知男性發生胃癌的機會是女性的兩倍。但到底是性別本身的關係,還是由於男性抽煙喝酒較多所致?仍在等待更多的研究。
老化:胃癌在50歲之後急速增加,年紀的變化扮演相當角色,研究指出或許與萎縮性胃炎在老年人發生率較高有關。
血型:早在1953年就有學者指出血型與胃癌的發生有關,A型的的人較其他它血型的人,得胃癌的機會多1/5。雖然已知血型是紅血球細胞上的抗原,與免疫系統有關,但為何A型血型的人有較高胃癌的發生率並不清楚。近年也有一些文獻不同意這種說法。
幽門螺旋桿菌:胃的長期的感染這細菌可引起慢性萎縮性胃炎,及一些免疫發炎反應。自1990初起就有許多研究報告指出,這細菌的感染與胃裡淋巴癌的產生有相當密切的關係,但對胃裡的腺癌則一爭議。目前有些證據顯示此幽門桿菌感染與胃體和胃竇部位的腺癌有關。但是胃腺癌也發生在一些未感染幽門桿菌的人身上,譬如在美國,少於1%的感染幽門桿菌病患會產生胃癌,而且目前也無確切的證據顯示預防或治療幽門桿菌感染可以降低胃癌發生的危險性。所以說暴露幽門螺旋桿菌的感染,似乎會增加得到胃癌的機會。1990年代Martin J. Blaser博士發現特定菌株類的幽門菌能產生一種毒液讓胃表面產生液泡[19],這種菌株稱為m1和s1基因種,有的人先天體質有促發炎基因如果同時遇到感染m1和s1基因種幽門菌,則胃癌機率會大升,但其他基因種幽門菌則沒有毒液能力,這可以算解答為何有些感染者並不導致胃癌率上升。
食物:流行病學的研究發現飲食的習慣與其內容與胃癌的發生有相當關係,據統計喜吃醺烤的食物、燒烤的肉類,醬菜鹹魚等鹽漬物者,胃癌的發生率較高。也有研究指出胃癌的發生率與鹽的消耗成正比。抽煙、喝酒也較容易促進胃癌的發生。在另一方面,吃新鮮水果和蔬菜,食用牛奶和維他命C則相對胃有保護作用,較少發生胃癌。
硝酸鹽和亞硝酸鹽:食物的保存及調理方式與胃癌的發生有密切的關係,硝酸鹽存在於一些蔬菜,某些飲用水,但也使用於肉類的燻製,它也可使鹽漬的肉類看起來較鮮紅。食物內的硝酸鹽,經腸胃內細菌還原成亞硝酸鹽,諸如幽門螺旋桿菌(Helicobacter pylori),與其他胺類再形成硝酸胺、亞硝酸胺。動物實驗已證實亞硝酸胺為頗強的致癌物,可引起胃裡細胞的癌變。另外有一點須特別注意是胃酸溶度太低,容易使細菌在胃裡滋生,增加了硝酸胺類的物質在胃裡的生成。低溫會抑制硝酸鹽轉變成亞硝酸鹽,也有學者指出這或許也是在美國胃癌發生率下降的原因之一,因為本世紀中期後冰箱才在北美洲變成必備的家電用品。
慢性萎縮性胃炎與黏膜腸上皮化生:萎縮性胃炎其胃酸分泌較低,胃黏膜也易形成腸上皮化生,胃癌的機會增加。年齡愈大,慢性萎縮性胃炎與黏膜腸上皮化生的比率也愈高。至於腸上皮化生在病理化驗有可分成三種亞型,以分化不完整的第三種亞型產生癌變的機會最高。
惡性貧血:惡性貧血是指因為胃無法生產一種物質,使得維他命B12吸收發生問題,缺乏導致的結果。這些人有1至12%會發生胃癌。
殘胃癌:雖然仍有爭議,但一些流行病學研究指出曾經接受胃部切除手術的人,較一般人患胃癌的比率為高,估計約2-5%到5-16%不等。此種殘餘胃發生癌變的時間,由前次手術算起約在15-30年後。這或許是因為胃切除手術後,胃酸較低,產生亞硝酸鹽細菌增多。所以接受過胃部切除手術的人,尤其是採Billrith-II吻合術的,10幾年後,若有任何上消化道症狀,都應接受內視鏡檢查。
Menetrier's疾病:這疾病也叫做肥厚性胃病變,胃皺摺不正常增厚,胃酸很低,發生胃癌機會較高。但這疾病十分少見。
癌症家族症候群:遺傳性非息肉大腸癌或家族性多發性息肉症,除發生直腸大腸癌的機會較大外,產生胃癌的機率亦較高。
胃息肉:息肉是小的瘤或黏膜長出香菇狀的贅物,絕大多數的胃息肉都不會有惡性病變,但是若胃腺性息肉大於2公分以上,其中30-40%會有惡性變化。
Gastric cancer occurs as a result of many factors.[20] It occurs twice as common in males as females. Estrogen may protect women against the development of this cancer form.[21][22]
Infections
Helicobacter pylori infection is an essential risk factor in 65–80% of gastric cancers, but only 2% of people with Helicobacter infections develop stomach cancer.[23][24] The mechanism by which H. pylori induces stomach cancer potentially involves chronic inflammation, or the action of H. pylori virulence factors such as CagA.[25] It was estimated that Epstein–Barr virus is responsible for 84,000 cases per year.[26] AIDS is also associated with elevated risk.[24]===Smoking=== Smoking increases the risk of developing gastric cancer significantly, from 40% increased risk for current smokers to 82% increase for heavy smokers. Gastric cancers due to smoking mostly occur in the upper part of the stomach near the esophagus.[27][28][29] Some studies show increased risk with alcohol consumption as well.[24][30]
Diet

Dietary factors are not proven causes,[32] but some foods including smoked foods,[33] salt and salt-rich foods, red meat, processed meat, pickled vegetables,[24] and bracken[34] are associated with a higher risk of stomach cancer. Nitrates and nitrites in cured meats can be converted by certain bacteria, including H. pylori, into compounds that have been found to cause stomach cancer in animals.
Fresh fruit and vegetable intake, citrus fruit intake, and antioxidant intake are associated with a lower risk of stomach cancer.[24][27] A Mediterranean diet is associated with lower rates of stomach cancer,[35] as is regular aspirin use.[24]
Obesity is a physical risk factor that has been found to increase the risk of gastric adenocarcinoma by contributing to the development of gastroesophageal reflux disease (GERD).[36] The exact mechanism by which obesity causes GERD is not completely known. Studies hypothesize that increased dietary fat leading to increased pressure on the stomach and the lower esophageal sphincter, due to excess adipose tissue, could play a role, yet no statistically significant data has been collected.[37] However, the risk of gastric cardia adenocarcinoma, with GERD present, has been found to increase more than 2 times for an obese person.[36] There is a correlation between iodine deficiency and gastric cancer.[38][39][40]
Genetics
About 10% of cases run in families and between 1% and 3% of cases are due to genetic syndromes inherited from a person's parents such as hereditary diffuse gastric cancer.[5]
A genetic risk factor for gastric cancer is a genetic defect of the CDH1 gene known as hereditary diffuse gastric cancer (HDGC). The CDH1 gene, which codes for E-cadherin, lies on the 16th chromosome.[41] When the gene experiences a particular mutation, gastric cancer develops through a mechanism that is not fully understood.[41] This mutation is considered autosomal dominant meaning that half of a carrier’s children will likely experience the same mutation.[41] Diagnosis of hereditary diffuse gastric cancer usually takes place when at least two cases involving a family member, such as a parent or grandparent, are diagnosed, with at least one diagnosed before the age of 50.[41] The diagnosis can also be made if there are at least three cases in the family, in which case age is not considered.[41]
The International Cancer Genome Consortium is leading efforts to identify genomic changes involved in stomach cancer.[42][43] A very small percentage of diffuse-type gastric cancers (see Histopathology below) arise from an inherited abnormal CDH1 gene. Genetic testing and treatment options are available for families at risk.[44]
Other
Other risks include diabetes,[45] pernicious anemia,[30] chronic atrophic gastritis,[46] Menetrier's disease (hyperplastic, hypersecretory gastropathy),[47] and intestinal metaplasia.[48]
Diagnosis
To find the cause of symptoms, the doctor asks about the patient's medical history, does a physical exam, and may order laboratory studies. The patient may also have one or all of the following exams:
- Gastroscopic exam is the diagnostic method of choice. This involves insertion of a fibre optic camera into the stomach to visualise it.[30]
- Upper GI series (may be called barium roentgenogram).
- Computed tomography or CT scanning of the abdomen may reveal gastric cancer. It is more useful to determine invasion into adjacent tissues or the presence of spread to local lymph nodes. Wall thickening of more than 1 cm that is focal, eccentric and enhancing favours malignancy.[49]
In 2013, Chinese and Israeli scientists reported a successful pilot study of a breathalyzer-style breath test intended to diagnose stomach cancer by analyzing exhaled chemicals without the need for an intrusive endoscopy.[50] A larger-scale clinical trial of this technology was completed in 2014.[51]
Abnormal tissue seen in a gastroscope examination will be biopsied by the surgeon or gastroenterologist. This tissue is then sent to a pathologist for histological examination under a microscope to check for the presence of cancerous cells. A biopsy, with subsequent histological analysis, is the only sure way to confirm the presence of cancer cells.[30]
Various gastroscopic modalities have been developed to increase yield of detected mucosa with a dye that accentuates the cell structure and can identify areas of dysplasia. Endocytoscopy involves ultra-high magnification to visualise cellular structure to better determine areas of dysplasia. Other gastroscopic modalities such as optical coherence tomography are being tested investigationally for similar applications.[52]
A number of cutaneous conditions are associated with gastric cancer. A condition of darkened hyperplasia of the skin, frequently of the axilla and groin, known as acanthosis nigricans, is associated with intra-abdominal cancers such as gastric cancer. Other cutaneous manifestations of gastric cancer include tripe palms (a similar darkening hyperplasia of the skin of the palms) and the Leser-Trelat sign, which is the rapid development of skin lesions known as seborrheic keratoses.[53]
Various blood tests may be done including a complete blood count (CBC) to check for anaemia, and a fecal occult blood test to check for blood in the stool.
Histopathology

- Gastric adenocarcinoma is a malignant epithelial tumour, originating from glandular epithelium of the gastric mucosa. Stomach cancers are overwhelmingly adenocarcinomas (90%).[54] Histologically, there are two major types of gastric adenocarcinoma (Lauren classification): intestinal type or diffuse type. Adenocarcinomas tend to aggressively invade the gastric wall, infiltrating the muscularis mucosae, the submucosa and thence the muscularis propria. Intestinal type adenocarcinoma tumour cells describe irregular tubular structures, harbouring pluristratification, multiple lumens, reduced stroma ("back to back" aspect). Often, it associates intestinal metaplasia in neighbouring mucosa. Depending on glandular architecture, cellular pleomorphism and mucosecretion, adenocarcinoma may present 3 degrees of differentiation: well, moderate and poorly differentiated. Diffuse type adenocarcinoma (mucinous, colloid, linitis plastica, leather-bottle stomach) tumour cells are discohesive and secrete mucus, which is delivered in the interstitium, producing large pools of mucus/colloid (optically "empty" spaces). It is poorly differentiated. If the mucus remains inside the tumour cell, it pushes the nucleus to the periphery: "signet-ring cell".
- Around 5% of gastric malignancies are lymphomas (MALTomas, or MALT lymphoma).[55]
- Carcinoid and stromal tumors may occur.
Staging

If cancer cells are found in the tissue sample, the next step is to stage, or find out the extent of the disease. Various tests determine whether the cancer has spread and, if so, what parts of the body are affected. Because stomach cancer can spread to the liver, the pancreas, and other organs near the stomach as well as to the lungs, the doctor may order a CT scan, a PET scan,[56] an endoscopic ultrasound exam, or other tests to check these areas. Blood tests for tumor markers, such as carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) may be ordered, as their levels correlate to extent of metastasis, especially to the liver, and the cure rate.
Staging may not be complete until after surgery. The surgeon removes nearby lymph nodes and possibly samples of tissue from other areas in the abdomen for examination by a pathologist.
The clinical stages of stomach cancer are:[57][58]
- Stage 0. Limited to the inner lining of the stomach. Treatable by endoscopic mucosal resection when found very early (in routine screenings); otherwise by gastrectomy and lymphadenectomy without need for chemotherapy or radiation.
- Stage I. Penetration to the second or third layers of the stomach (Stage 1A) or to the second layer and nearby lymph nodes (Stage 1B). Stage 1A is treated by surgery, including removal of the omentum. Stage 1B may be treated with chemotherapy (5-fluorouracil) and radiation therapy.
- Stage II. Penetration to the second layer and more distant lymph nodes, or the third layer and only nearby lymph nodes, or all four layers but not the lymph nodes. Treated as for Stage I, sometimes with additional neoadjuvant chemotherapy.
- Stage III. Penetration to the third layer and more distant lymph nodes, or penetration to the fourth layer and either nearby tissues or nearby or more distant lymph nodes. Treated as for Stage II; a cure is still possible in some cases.
- Stage IV. Cancer has spread to nearby tissues and more distant lymph nodes, or has metastasized to other organs. A cure is very rarely possible at this stage. Some other techniques to prolong life or improve symptoms are used, including laser treatment, surgery, and/or stents to keep the digestive tract open, and chemotherapy by drugs such as 5-fluorouracil, cisplatin, epirubicin, etoposide, docetaxel, oxaliplatin, capecitabine or irinotecan.

The TNM staging system is also used.[59]
In a study of open-access endoscopy in Scotland, patients were diagnosed 7% in Stage I 17% in Stage II, and 28% in Stage III.[60] A Minnesota population was diagnosed 10% in Stage I, 13% in Stage II, and 18% in Stage III.[61] However, in a high-risk population in the Valdivia Province of southern Chile, only 5% of patients were diagnosed in the first two stages and 10% in stage III.[62]
Prevention
Getting rid of H. pylori in those who are infected decreases the risk of stomach cancer, at least in those who are Asian.[63] A 2014 meta-analysis of observational studies found that a diet high in fruits, mushrooms, garlic, soybeans, and green onions was associated with a lower risk of stomach cancer in the Korean population.[64] Low doses of vitamins, especially from a healthy diet, decrease the risk of stomach cancer.[65] A previous review of antioxidant supplementation did not find supporting evidence and possibly worse outcomes.[66][67]
Management
Cancer of the stomach is difficult to cure unless it is found at an early stage (before it has begun to spread). Unfortunately, because early stomach cancer causes few symptoms, the disease is usually advanced when the diagnosis is made.[68]
Treatment for stomach cancer may include surgery,[69] chemotherapy, and/or radiation therapy.[70] New treatment approaches such as biological therapy and improved ways of using current methods are being studied in clinical trials.[71]
Surgery
Surgery remains the only curative therapy for stomach cancer.[8] Of the different surgical techniques, endoscopic mucosal resection (EMR) is a treatment for early gastric cancer (tumor only involves the mucosa) that was pioneered in Japan and is available in the United States at some centers.[8] In this procedure, the tumor, together with the inner lining of stomach (mucosa), is removed from the wall of the stomach using an electrical wire loop through the endoscope. The advantage is that it is a much smaller operation than removing the stomach.[8] Endoscopic submucosal dissection (ESD) is a similar technique pioneered in Japan, used to resect a large area of mucosa in one piece.[8] If the pathologic examination of the resected specimen shows incomplete resection or deep invasion by tumor, the patient would need a formal stomach resection.[8] A 2016 Cochrane review found low quality evidence of no difference in short-term mortality between laparoscopic and open gastrectomy (removal of stomach), and that benefits or harms of laparoscopic gastrectomy cannot be ruled out.[72]
Those with metastatic disease at the time of presentation may receive palliative surgery and while it remains controversial, due to the possibility of complications from the surgery itself and the fact that it may delay chemotherapy the data so far is mostly positive, with improved survival rates being seen in those treated with this approach.[8][73]
Chemotherapy
The use of chemotherapy to treat stomach cancer has no firmly established standard of care. Unfortunately, stomach cancer has not been particularly sensitive to these drugs, and chemotherapy, if used, has usually served to palliatively reduce the size of the tumor, relieve symptoms of the disease and increase survival time. Some drugs used in stomach cancer treatment have included: 5-FU (fluorouracil) or its analog capecitabine, BCNU (carmustine), methyl-CCNU (semustine) and doxorubicin (Adriamycin), as well as mitomycin C, and more recently cisplatin and taxotere, often using drugs in various combinations. The relative benefits of these different drugs, alone and in combination, are unclear.[74] Clinical researchers are exploring the benefits of giving chemotherapy before surgery to shrink the tumor, or as adjuvant therapy after surgery to destroy remaining cancer cells.[8]
Targeted therapy
Recently, treatment with human epidermal growth factor receptor 2 (HER2) inhibitor, trastuzumab, has been demonstrated to increase overall survival in inoperable locally advanced or metastatic gastric carcinoma over-expressing the HER2/neu gene.[8] In particular, HER2 is overexpressed in 13-22% of patients with gastric cancer.[71][75] Of note, HER2 overexpression in gastric neoplasia is heterogeneous and comprises a minority of tumor cells (less than 10% of gastric cancers overexpress HER2 in more than 5% of tumor cells). Hence, this heterogeneous expression should be taken into account for HER2 testing, particularly in small samples such as biopsies, requiring the evaluation of more than one bioptic sample.[75]
Radiation
Radiation therapy (also called radiotherapy) may be used to treat stomach cancer, often as an adjuvant to chemotherapy and/or surgery.[8]
Prognosis
The prognosis of stomach cancer is generally poor, due to the fact the tumour has often metastasised by the time of discovery and the fact that most people with the condition are elderly (median age is between 70 and 75 years) at presentation.[76] The five-year survival rate for stomach cancer is reported to be less than 10 percent.[8]
Epidemiology

Worldwide, stomach cancer is the fifth most common cancer with 952,000 cases diagnosed in 2012.[10] It is more common in men and in developing countries.[77][78] In 2012, it represented 8.5% of cancer cases in men, making it the fourth most common cancer in men.[79] In 2012 number of deaths were 700,000 having decreased slightly from 774,000 in 1990 making it the third leading cause of cancer death after lung cancer and liver cancer.[80][81]
Less than 5% of stomach cancers occur in people under 40 years of age with 81.1% of that 5% in the age-group of 30 to 39 and 18.9% in the age-group of 20 to 29.[82]
In 2014, stomach cancer accounted for 0.61% of deaths (13,303 cases) in the United States.[83] In China, stomach cancer accounted for 3.56% of all deaths (324,439 cases).[84] The highest rate of stomach cancer was in Mongolia, at 28 cases per 100,000 people.[85]
In the United Kingdom, stomach cancer is the fifteenth most common cancer (around 7,100 people were diagnosed with stomach cancer in 2011), and it is the tenth most common cause of cancer death (around 4,800 people died in 2012).[86]
Incidence and mortality rates of gastric cancer vary greatly in Africa. The GLOBOCAN system is currently the most widely used method to compare these rates between countries, but African incidence and mortality rates are seen to differ among countries possibly due to the lack of universal access to a registry system for all countries.[87] Variation as drastic as estimated rates from 0.3/100000 in Botswana to 20.3/100000 in Mali have been observed.[87] In Uganda, the incidence of gastric cancer has increased from the 1960s measurement of 0.8/100000 to 5.6/100000.[87] Gastric cancer, though present, is relatively low when compared to countries with high incidence like Japan or China. One suspected cause of the variation within Africa and between other countries is due to different strains of the Helicobacter pylori bacteria. The trend commonly seen is that H. pylori infection increases the risk for gastric cancer, however this is not the case in Africa giving this phenomenon the name the “African enigma.”[88] Although this bacteria is found in Africa, evidence has supported that different strains with mutations in the bacterial genotype may contribute to the difference in cancer development between African countries and others outside of the continent.[88] However, increasing access to health care and treatment measures have been commonly associated with the rising incidence, particularly in Uganda.[87]
Other animals
The stomach is a muscular organ of the gastrointestinal tract that holds food and begins the digestive process by secreting gastric juice. The most common cancers of the stomach are adenocarcinomas but other histological types have been reported. Signs vary but may include vomiting (especially if blood is present), weight loss, anemia, and lack of appetite. Bowel movements may be dark and tarry in nature. In order to determine whether cancer is present in the stomach, special X-rays and/or abdominal ultrasound may be performed. Gastroscopy, a test using an instrument called endoscope to examine the stomach, is a useful diagnostic tool that can also take samples of the suspected mass for histopathological analysis to confirm or rule out cancer. The most definitive method of cancer diagnosis is through open surgical biopsy.[89] Most stomach tumors are malignant with evidence of spread to lymph nodes or liver, making treatment difficult. Except for lymphoma, surgery is the most frequent treatment option for stomach cancers but it is associated with significant risks.
參考資料
- ^ Stomach (Gastric) Cancer. NCI. [1 July 2014].
- ^ 2.0 2.1 2.2 2.3 2.4 Gastric Cancer Treatment (PDQ®). NCI. 2014-04-17 [1 July 2014].
- ^ Ruddon, Raymond W. Cancer biology 4th. Oxford: Oxford University Press. 2007: 223. ISBN 9780195175431.
- ^ Sim, edited by Fiona; McKee, Martin. Issues in public health 2nd. Maidenhead: Open University Press. 2011: 74. ISBN 9780335244225.
- ^ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 World Cancer Report 2014. World Health Organization. 2014: Chapter 5.4. ISBN 9283204298.
- ^ Chang, A. H.; Parsonnet, J. Role of Bacteria in Oncogenesis. Clinical Microbiology Reviews. 2010, 23 (4): 837–857. ISSN 0893-8512. PMC 2952975
 . PMID 20930075. doi:10.1128/CMR.00012-10.
. PMID 20930075. doi:10.1128/CMR.00012-10.
- ^ Stomach (Gastric) Cancer Prevention (PDQ®). NCI. 2014-02-27 [1 July 2014].
- ^ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Orditura, M; Galizia, G; Sforza, V; Gambardella, V; Fabozzi, A; Laterza, MM; Andreozzi, F; Ventriglia, J; Savastano, B; Mabilia, A; Lieto, E; Ciardiello, F; De Vita, F. Treatment of gastric cancer. (PDF). World Journal of Gastroenterology. February 2014, 20 (7): 1635–49. PMC 3930964
 . PMID 24587643. doi:10.3748/wjg.v20.i7.1635.
. PMID 24587643. doi:10.3748/wjg.v20.i7.1635.
- ^ SEER Stat Fact Sheets: Stomach Cancer. NCI. [18 June 2014].
- ^ 10.0 10.1 10.2 Chapter 1.1. World Cancer Report 2014. World Health Organization. 2014. ISBN 9283204298.
- ^ Hochhauser, Jeffrey Tobias, Daniel. Cancer and its management 6th. Chichester, West Sussex, UK: Wiley-Blackwell. 2010: 259. ISBN 9781444306378.
- ^ Khleif, Edited by Roland T. Skeel, Samir N. Handbook of cancer chemotherapy 8th. Philadelphia: Wolter Kluwer. 2011: 127. ISBN 9781608317820.
- ^ Joseph A Knight. Human Longevity: The Major Determining Factors. Author House. 2010: 339. ISBN 9781452067223.
- ^ Moore, edited by Rhonda J.; Spiegel, David. Cancer, culture, and communication. New York: Kluwer Academic. 2004: 139. ISBN 9780306478857.
- ^ Statistics and outlook for stomach cancer. Cancer Research UK. [19 February 2014].
- ^ Guidance on Commissioning Cancer Services Improving Outcomes in Upper Gastro-intestinal Cancers (PDF). NHS. Jan 2001.
- ^ Sim, edited by Fiona; McKee, Martin. Issues in public health 2nd. Maidenhead: Open University Press. 2011: 74. ISBN 9780335244225.
- ^ Ruddon, Raymond W. Cancer biology 4th. Oxford: Oxford University Press. 2007: 223. ISBN 9780195175431.
- ^ 科學人-幽門螺旋菌與胃壁細胞的作用機制
- ^ Lee YY, Derakhshan MH. Environmental and lifestyle risk factors of gastric cancer. Arch. Iran. Med. Jun 2013, 16 (6): 358–65. PMID 23725070.
- ^ Chandanos E, Lagergren J. Oestrogen and the enigmatic male predominance of gastric cancer. Eur J Cancer. Nov 2008, 44 (16): 2397–403. doi:10.1016/j.ejca.2008.07.031.
- ^ Qin J, Liu M, Ding Q, Ji X, Hao Y, Wu X, Xiong J. The direct effect of estrogen on cell viability and apoptosis in human gastric cancer cells. Mol Cell Biochem. Oct 2014, 395 (1–2): 99–107. doi:10.1007/s11010-014-2115-2.
- ^ Proceedings of the fourth Global Vaccine Research Forum (PDF). Initiative for Vaccine Research team of the Department of Immunization, Vaccines and Biologicals. WHO. April 2004 [2009-05-11].
Epidemiology of Helicobacter pylori and gastric cancer…
- ^ 24.0 24.1 24.2 24.3 24.4 24.5 González CA, Sala N, Rokkas T; Sala; Rokkas. Gastric cancer: epidemiologic aspects. Helicobacter. 2013, 18 (Supplement 1): 34–38. PMID 24011243. doi:10.1111/hel.12082.
- ^ Hatakeyama, M. & Higashi, H; Higashi. Helicobacter pylori CagA: a new paradigm for bacterial carcinogenesis. Cancer Science. 2005, 96 (12): 835–843. PMID 16367902. doi:10.1111/j.1349-7006.2005.00130.x.
- ^ Developing a vaccine for the Epstein-Barr Virus could prevent up to 200,000 cancers globally say experts. Cancer Research UK. [2017-03-17].
- ^ 27.0 27.1 What Are The Risk Factors For Stomach Cancer(Website). American Cancer Society. [2010-03-31].
- ^ Nomura A, Grove JS, Stemmermann GN, Severson RK; Grove; Stemmermann; Severson. Cigarette smoking and stomach cancer. Cancer Research. 1990, 50 (21): 7084. PMID 2208177.
- ^ Trédaniel J, Boffetta P, Buiatti E, Saracci R, Hirsch A; Boffetta; Buiatti; Saracci; Hirsch. Tobacco smoking and gastric cancer: Review and meta-analysis. International Journal of Cancer. August 1997, 72 (4): 565–73. PMID 9259392. doi:10.1002/(SICI)1097-0215(19970807)72:4<565::AID-IJC3>3.0.CO;2-O.
- ^ 30.0 30.1 30.2 30.3 Thrumurthy SG, Chaudry MA, Hochhauser D, Ferrier K, Mughal M; Chaudry; Hochhauser; Mughal. The diagnosis and management of gastric cancer. British Medical Journal. 2013, 347 (16): 1695–6. PMID 24191271. doi:10.1136/bmj.f6367.
- ^ Venturi, S.; Donati, F.M.; Venturi, A.; Venturi, M. Environmental Iodine Deficiency: A Challenge to the Evolution of Terrestrial Life?. Thyroid. 2000, 10 (8): 727–9. PMID 11014322. doi:10.1089/10507250050137851.
- ^ Tumors of the GI Tract 来自默克诊疗手册专业版
- ^ Jakszyn P, González CA; Gonzalez. Nitrosamine and related food intake and gastric and oesophageal cancer risk: A systematic review of the epidemiological evidence (PDF). World J Gastroenterol. 2006, 12 (27): 4296–4303. PMC 4087738
 . PMID 16865769. doi:10.3748/wjg.v12.i27.4296.
. PMID 16865769. doi:10.3748/wjg.v12.i27.4296.
- ^ Alonso-Amelot ME, Avendaño M; Avendaño. Human carcinogenesis and bracken fern: a review of the evidence. Current Medicinal Chemistry. March 2002, 9 (6): 675–86. PMID 11945131. doi:10.2174/0929867023370743.
- ^ Buckland G, Agudo A, Lujan L, Jakszyn P, Bueno-De-Mesquita HB, Palli D, Boeing H, Carneiro F, Krogh V; Agudo; Luján; Jakszyn; Bueno-De-Mesquita; Palli; Boeing; Carneiro; Krogh; Sacerdote; Tumino; Panico; Nesi; Manjer; Regnér; Johansson; Stenling; Sanchez; Dorronsoro; Barricarte; Navarro; Quirós; Allen; Key; Bingham; Kaaks; Overvad; Jensen; Olsen; et al. Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. American Journal of Clinical Nutrition. 2009, 91 (2): 381–90. PMID 20007304. doi:10.3945/ajcn.2009.28209.
- ^ 36.0 36.1 Crew K, Neugut A. Epidemiology of gastric cancer. World Journal of Gastroenterology. January 2006, 12 (3): 354–62. PMC 4066052
 . PMID 16489633. doi:10.3748/wjg.v12.i3.354.
. PMID 16489633. doi:10.3748/wjg.v12.i3.354.
- ^ Hampel Howard; Abraham Neena S.; El-Serag Hashem B. Meta-Analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Annals of Internal Medicine. August 2005, 143 (3): 199–211. doi:10.7326/0003-4819-143-3-200508020-00006.
- ^ Josefssson, M.; Ekblad, E. 22. Sodium Iodide Symporter (NIS) in Gastric Mucosa: Gastric Iodide Secretion. Preedy, Victor R.; Burrow, Gerard N.; Watson, Ronald (编). Comprehensive Handbook of Iodine: Nutritional, Biochemical, Pathological and Therapeutic Aspects. Elsevier. 2009: 215–220. ISBN 978-0-12-374135-6.
- ^ Venturi, Sebastiano. Evolutionary Significance of Iodine. Current Chemical Biology-. 2011, 5 (3): 155–162. ISSN 1872-3136. doi:10.2174/187231311796765012.
- ^ Venturi II, S.; Donati, F.M.; Venturi, A.; Venturi, M.;; Venturi, A; Venturi, M; Grossi, L; Guidi, A. Role of iodine in evolution and carcinogenesis of thyroid, breast and stomach.. Adv Clin Path. 2000, 4 (1): 11–17. PMID 10936894.
- ^ 41.0 41.1 41.2 41.3 41.4 Hereditary Diffuse Cancer. No Stomach for Cancer. [21 Oct 2014].
- ^ Gastric Cancer — Adenocarcinoma. International Cancer Genome Consortium. [24 February 2014].
- ^ Gastric Cancer — Intestinal- and diffuse-type. International Cancer Genome Consortium. [24 February 2014].
- ^ Brooks-Wilson AR, Kaurah P, Suriano G, Leach S, Senz J, Grehan N, Butterfield YS, Jeyes J, Schinas J; Kaurah; Suriano; Leach; Senz; Grehan; Butterfield; Jeyes; Schinas; Bacani; Kelsey; Ferreira; MacGillivray; MacLeod; Micek; Ford; Foulkes; Australie; Greenberg; Lapointe; Gilpin; Nikkel; Gilchrist; Hughes; Jackson; Monaghan; Oliveira; Seruca; Gallinger; et al. Germline E-cadherin mutations in hereditary diffuse gastric cancer: assessment of 42 new families and review of genetic screening criteria. Journal of Medical Genetics. 2004, 41 (7): 508–17. PMC 1735838
 . PMID 15235021. doi:10.1136/jmg.2004.018275.
. PMID 15235021. doi:10.1136/jmg.2004.018275.
- ^ Tseng C-H, Tseng F-H; Tseng. Diabetes and gastric cancer: The potential links. World J Gastroenterol. 2014, 20 (7): 1701–11. PMC 3930970
 . PMID 24587649. doi:10.3748/wjg.v20.i7.1701.
. PMID 24587649. doi:10.3748/wjg.v20.i7.1701.
- ^ Crosby DA, Donohoe CL, Fitzgerald L, Muldoon C, Hayes B, O’Toole D, Reynolds JV; Donohoe; Fitzgerald; Muldoon; Hayes; O'Toole; Reynolds. Gastric Neuroendocrine Tumours. Digestive Surgery. 2004, 29 (4): 331–348. PMID 23075625. doi:10.1159/000342988.
- ^ Kim J, Cheong JH, Chen J, Hyung WJ, Choi SH, Noh SH; Cheong; Chen; Hyung; Choi; Noh. Menetrier's Disease in Korea: Report of Two Cases and Review of Cases in a Gastric Cancer Prevalent Region (PDF). Yonsei Medical Journal. 2004, 45 (3): 555–560. PMID 15227748. doi:10.3349/ymj.2004.45.3.555.
- ^ Tsukamoto T, Mizoshita T, Tatematsu M; Mizoshita; Tatematsu. Gastric-and-intestinal mixed-type intestinal metaplasia: aberrant expression of transcription factors and stem cell intestinalization. Gastric Cancer. 2006, 9 (3): 156–166. PMID 16952033. doi:10.1007/s10120-006-0375-6.
- ^ Virmani, V; Khandelwal, A; Sethi, V; Fraser-Hill, M; Fasih, N; Kielar, A. Neoplastic stomach lesions and their mimickers: Spectrum of imaging manifestations. Cancer Imaging. 2012, 12: 269–78. PMC 3458788
 . PMID 22935192. doi:10.1102/1470-7330.2012.0031.
. PMID 22935192. doi:10.1102/1470-7330.2012.0031.
- ^ Xu ZQ, Broza YY, Ionsecu R, et al. A nanomaterial-based breath test for distinguishing gastric cancer from benign gastric conditions. Br. J. Cancer. March 2013, 108 (4): 941–50. PMC 3590679
 . PMID 23462808. doi:10.1038/bjc.2013.44. 简明摘要 – Medical News Today ("Breath Test Could Detect and Diagnose Stomach Cancer") (6 March 2013).
. PMID 23462808. doi:10.1038/bjc.2013.44. 简明摘要 – Medical News Today ("Breath Test Could Detect and Diagnose Stomach Cancer") (6 March 2013).
- ^ Amal H, Leja M, Funka K, Skapars R, Sivins A, Ancans G, Liepniece-Karele I, Kikuste I, Lasina I, Haick H. Detection of precancerous gastric lesions and gastric cancer through exhaled breath. Gut. 13 April 2015, 65: 400–7. PMID 25869737. doi:10.1136/gutjnl-2014-308536.
- ^ Inoue H, Kudo S-, Shiokawa A; Kudo; Shiokawa. Technology Insight: laser-scanning confocal microscopy and endocytoscopy for cellular observation of the gastrointestinal tract. Nature Clinical Practice Gastroenterology & Hepatology. 2005, 2 (1): 31–7. PMID 16265098. doi:10.1038/ncpgasthep0072.
- ^ Pentenero M, Carrozzo M, Pagano M, Gandolfo S; Carrozzo; Pagano; Gandolfo. Oral acanthosis nigricans, tripe palms and sign of leser-trelat in a patient with gastric adenocarcinoma. International Journal of Dermatology. 2004, 43 (7): 530–2. PMID 15230897. doi:10.1111/j.1365-4632.2004.02159.x.
- ^ Kumar; et al. Pathologic Basis of Disease 8th. Saunders Elsevier. 2010: 784. ISBN 978-1-4160-3121-5.
- ^ Kumar 2010,第786頁
- ^ Lim JS, Yun MJ, Kim MJ, Hyung WJ, Park MS, Choi JY, Kim TS, Lee JD, Noh SH, Kim KW; Yun; Kim; Hyung; Park; Choi; Kim; Lee; Noh; Kim. CT and PET in stomach cancer: preoperative staging and monitoring of response to therapy. Radiographics. 2006, 26 (1): 143–156. PMID 16418249. doi:10.1148/rg.261055078.
- ^ Detailed Guide: Stomach Cancer Treatment Choices by Type and Stage of Stomach Cancer. American Cancer Society. 2009-11-03.
- ^ Guy Slowik. What Are The Stages Of Stomach Cancer?. ehealthmd.com. October 2009.
- ^ Detailed Guide: Stomach Cancer: How Is Stomach Cancer Staged?. American Cancer Society.
- ^ Paterson HM, McCole D, Auld CD; McCole; Auld. Impact of open-access endoscopy on detection of early oesophageal and gastric cancer 1994–2003: population-based study. Endoscopy. 2006, 38 (5): 503–7. PMID 16767587. doi:10.1055/s-2006-925124.
- ^ Crane SJ, Locke GR, Harmsen WS, Zinsmeister AR, Romero Y, Talley NJ; Locke Gr; Harmsen; Zinsmeister; Romero; Talley. Survival Trends in Patients With Gastric and Esophageal Adenocarcinomas: A Population-Based Study. Mayo Clinic Proceedings. 2008, 83 (10): 1087–94. PMC 2597541
 . PMID 18828967. doi:10.4065/83.10.1087.
. PMID 18828967. doi:10.4065/83.10.1087.
- ^ Heise K, Bertran E, Andia ME, Ferreccio C; Bertran; Andia; Ferreccio. Incidence and survival of stomach cancer in a high-risk population of Chile. World Journal of Gastroenterology. 2009, 15 (15): 1854–62. PMC 2670413
 . PMID 19370783. doi:10.3748/wjg.15.1854.
. PMID 19370783. doi:10.3748/wjg.15.1854.
- ^ Ford, AC; Forman, D; Hunt, RH; Yuan, Y; Moayyedi, P. Helicobacter pylori eradication therapy to prevent gastric cancer in healthy asymptomatic infected individuals: systematic review and meta-analysis of randomised controlled trials.. BMJ. 20 May 2014, 348: g3174. PMC 4027797
 . PMID 24846275. doi:10.1136/bmj.g3174.
. PMID 24846275. doi:10.1136/bmj.g3174.
- ^ Woo HD, Park S, Oh K, Kim HJ, Shin HR, Moon HK, Kim J. Diet and cancer risk in the Korean population: a meta- analysis (PDF). Asian Pacific Journal of Cancer Prevention. 2014, 15 (19): 8509–19. PMID 25339056. doi:10.7314/apjcp.2014.15.19.8509.
- ^ Kong, P; Cai, Q; Geng, Q; Wang, J; Lan, Y; Zhan, Y; Xu, D. Vitamin intake reduce the risk of gastric cancer: meta-analysis and systematic review of randomized and observational studies.. PLOS ONE. 2014, 9 (12): e116060. PMC 4280145
 . PMID 25549091. doi:10.1371/journal.pone.0116060.
. PMID 25549091. doi:10.1371/journal.pone.0116060.
- ^ Bjelakovic, G; Nikolova, D; Simonetti, RG; Gluud, C. Antioxidant supplements for preventing gastrointestinal cancers.. Cochrane Database of Systematic Reviews. 16 July 2008, (3): CD004183. PMID 18677777. doi:10.1002/14651858.CD004183.pub3.
- ^ Bjelakovic, G; Nikolova, D; Gluud, LL; Simonetti, RG; Gluud, C. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases.. Cochrane Database of Systematic Reviews. 14 March 2012, 3: CD007176. PMID 22419320. doi:10.1002/14651858.CD007176.pub2.
- ^ Roopma Wadhwa, Takashi Taketa, Kazuki Sudo, Mariela A. Blum, Jaffer A. Ajani; Taketa; Sudo; Blum; Ajani. Modern Oncological Approaches to Gastric Adenocarcinoma. Gastroenterology Clinics of North America. 2013, 42 (2): 359–369. PMID 23639645. doi:10.1016/j.gtc.2013.01.011.
- ^ Ke Chen, Xiao-Wu Xu, Ren-Chao Zhang, Yu Pan, Di Wu, Yi-Ping Mou; Xu; Zhang; Pan; Wu; Mou. Systematic review and meta-analysis of laparoscopy-assisted and open total gastrectomy for gastric cancer. World J Gastroenterol. 2013, 19 (32): 5365–76. PMC 3752573
 . PMID 23983442. doi:10.3748/wjg.v19.i32.5365.
. PMID 23983442. doi:10.3748/wjg.v19.i32.5365.
- ^ Jennifer L. Pretz, Jennifer Y. Wo, Harvey J. Mamon, Lisa A. Kachnic, Theodore S. Hong; Wo; Mamon; Kachnic; Hong. Chemoradiation Therapy: Localized Esophageal, Gastric, and Pancreatic Cancer. Surgical Oncology Clinics of North America. 2011, 22 (3): 511–524. PMID 23622077. doi:10.1016/j.soc.2013.02.005.
- ^ 71.0 71.1 Judith Meza-Junco, Heather-Jane Au, Michael B Sawyer; Au; Sawyer. Critical appraisal of trastuzumab in treatment of advanced stomach cancer. Cancer Management and Research. 2011, 3: 57–64. PMC 3085240
 . PMID 21556317. doi:10.2147/CMAR.S12698.
. PMID 21556317. doi:10.2147/CMAR.S12698.
- ^ Best, LM; Mughal, M; Gurusamy, KS. Laparoscopic versus open gastrectomy for gastric cancer.. The Cochrane database of systematic reviews. 31 March 2016, 3: CD011389 [5 April 2016]. PMID 27030300. doi:10.1002/14651858.CD011389.pub2.
- ^ Sun, J; Song, Y; Wang, Z; Chen, X; Gao, P; Xu, Y; Zhou, B; Xu, H. Clinical significance of palliative gastrectomy on the survival of patients with incurable advanced gastric cancer: a systematic review and meta-analysis. (PDF). BMC Cancer. December 2013, 13 (1): 577. PMID 24304886. doi:10.1186/1471-2407-13-577.
- ^ Scartozzi M, Galizia E, Verdecchia L, Berardi R, Antognoli S, Chiorrini S, Cascinu S; Galizia; Verdecchia; Berardi; Antognoli; Chiorrini; Cascinu. Chemotherapy for advanced gastric cancer: across the years for a standard of care. Expert Opinion on Pharmacotherapy. 2007, 8 (6): 797–808. PMID 17425475. doi:10.1517/14656566.8.6.797.
- ^ 75.0 75.1 Fusco N, Rocco EG, Del Conte C, Pellegrini C, Bulfamante G, Di Nuovo F, Romagnoli S, Bosari S. HER2 in gastric cancer: a digital image analysis in pre-neoplastic, primary and metastatic lesions. Mod Pathol. Jun 2013, 26 (6): 816–24. PMID 23348899. doi:10.1038/modpathol.2012.228.
- ^ Cabebe, EC; Mehta, VK; Fisher, G, Jr. Talavera, F; Movsas, M; McKenna, R; Harris, JE , 编. Gastric Cancer. Medscape Reference. WebMD. 21 January 2014 [4 April 2014].
- ^ Parkin DM, Bray F, Ferlay J, Pisani P; Bray; Ferlay; Pisani. Global Cancer Statistics, 2002. CA: A Cancer Journal for Clinicians. 2005, 55 (2): 74–108. PMID 15761078. doi:10.3322/canjclin.55.2.74.
- ^ Are the number of cancer cases increasing or decreasing in the world?. WHO Online Q&A. WHO. 1 April 2008 [2009-05-11].
- ^ World Cancer Report 2014. International Agency for Research on Cancer, World Health Organization. 2014. ISBN 978-92-832-0432-9.
- ^ Lozano, R; Naghavi, M; Foreman, K; Lim, S; Shibuya, K; Aboyans, V; Abraham, J; Adair, T; Aggarwal, R; Ahn, SY; Alvarado, M; Anderson, HR; Anderson, LM; Andrews, KG; Atkinson, C; Baddour, LM; Barker-Collo, S; Bartels, DH; Bell, ML; Benjamin, EJ; Bennett, D; Bhalla, K; Bikbov, B; Bin Abdulhak, A; Birbeck, G; Blyth, F; Bolliger, I; Boufous, S; Bucello, C; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 15 December 2012, 380 (9859): 2095–128. PMID 23245604. doi:10.1016/S0140-6736(12)61728-0.
- ^ PRESS RELEASE N° 224 Global battle against cancer won’t be won with treatment alone: Effective prevention measures urgently needed to prevent cancer crisis (PDF). World Health Organization. 3 February 2014 [14 March 2014].
- ^ Gastric Cancer in Young Adults. Revista Brasileira de Cancerologia. Jul 2000, 46 (3).
- ^ Health profile: United States. Le Duc Media. [31 Jan 2016].
- ^ Health profile: China. Le Duc Media. [31 Jan 2016].
- ^ Stomach Cancer: Death Rate Per 100,000. Le Duc Media. [13 March 2014].
- ^ Stomach cancer statistics. Cancer Research UK. [28 October 2014].
- ^ 87.0 87.1 87.2 87.3 Asombang Akwi W; Rahman Rubayat; Ibdah Jamal A. Gastric cancer in Africa: Current management and outcomes. World Journal of Gastroenterology. 2014, 20: 3875–79. PMC 3983443
 . PMID 24833842. doi:10.3748/wjg.v20.i14.3875.
. PMID 24833842. doi:10.3748/wjg.v20.i14.3875.
- ^ 88.0 88.1 Louw J. A.; Kidd M. S. G.; Kummer A. F.; Taylor K.; Kotze U.; Hanslo D. The relationship between helicobacter pylori infection, the virulence genotypes of the infecting strain and gastric cancer in the African setting. Helicobacter. November 2001, 6 (4): 268–73. doi:10.1046/j.1523-5378.2001.00044.x.
- ^ Withrow SJ, MacEwen EG (编). Small Animal Clinical Oncology 3rd. W.B. Saunders. 2001.
參考文獻
外部連結
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
