2型糖尿病:修订间差异
小 bot: 清理跨語言連結自體免疫成為內部連結:編輯摘要的red link經繁簡轉換後存在 |
无编辑摘要 |
||
| 第43行: | 第43行: | ||
===併发症=== |
===併发症=== |
||
2型糖尿病是慢性疾病,患者的预期寿命可减少長達10年<ref name=Will2011/>。导致预期寿命减少的部分原因是相关的并发症,包括:患上[[心血管疾病]]的风险是健康人群的二至四倍,其中包括[[冠狀動脈疾病|缺血性心脏病]]及[[中风]]等等。下肢[[截肢]]率會增加20倍,住院率亦相对增高<ref name=Will2011/>。在发达国家及越来越多的其他地区里,2型糖尿病是导致非创伤性[[失明]]及[[慢性肾病|肾衰竭]]的首要原因<ref name=AFP09/>。在发病过程中,患者罹患{{tsl|en|cognitive dysfunction|认知功能障碍}}及[[失智症]]风险也会增高,如[[阿兹海默病]]及[[血管性痴呆]]等等<ref>{{cite journal|last=Pasquier|first=F|title=Diabetes and cognitive impairment: how to evaluate the cognitive status?|journal=Diabetes & Metabolism|date=October 2010|volume=36 Suppl 3|pages=S100–5|doi=10.1016/S1262-3636(10)70475-4|pmid=21211730}}</ref>。其他并发症還包括[[黑棘皮症]]、[[性功能障碍]],以及容易发生感染<ref name=Vij2010/>。 |
2型糖尿病是慢性疾病,患者的预期寿命可减少長達10年<ref name=Will2011/>。导致预期寿命减少的部分原因是相关的并发症,包括:患上[[心血管疾病]]的风险是健康人群的二至四倍,其中包括[[冠狀動脈疾病|缺血性心脏病]]及[[中风]]等等。下肢[[截肢]]率會增加20倍,住院率亦相对增高<ref name=Will2011/>。在发达国家及越来越多的其他地区里,2型糖尿病是导致非创伤性[[失明]]及[[慢性肾病|肾衰竭]]的首要原因<ref name=AFP09/>。在发病过程中,患者罹患{{tsl|en|cognitive dysfunction|认知功能障碍}}及[[失智症]]风险也会增高,如[[阿兹海默病]]及[[血管性痴呆]]等等<ref>{{cite journal|last=Pasquier|first=F|title=Diabetes and cognitive impairment: how to evaluate the cognitive status?|journal=Diabetes & Metabolism|date=October 2010|volume=36 Suppl 3|pages=S100–5|doi=10.1016/S1262-3636(10)70475-4|pmid=21211730}}</ref>。其他并发症還包括[[黑棘皮症]]、[[性功能障碍]],以及容易发生感染<ref name=Vij2010/>。 |
||
糖尿病患相較於正常族群會增加2到4倍的心血管疾病風險,約32%的糖友合併有心血管疾病。<ref>{{Cite journal|title=Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017|url=https://cardiab.biomedcentral.com/articles/10.1186/s12933-018-0728-6|last=Einarson|first=Thomas R.|last2=Acs|first2=Annabel|date=2018-12|journal=Cardiovascular Diabetology|issue=1|doi=10.1186/s12933-018-0728-6|volume=17|pages=83|language=en|issn=1475-2840|pmc=PMC5994068|pmid=29884191|last3=Ludwig|first3=Craig|last4=Panton|first4=Ulrik H.}}</ref>心血管疾病是全世界糖尿病患者最重要的併發症及主要死因,近6成的糖尿病患者死於心血管疾病。<ref>{{Cite journal|title=Diabetes Mellitus, Fasting Glucose, and Risk of Cause-Specific Death|url=http://dx.doi.org/10.1056/nejmoa1008862|date=2011-03-03|journal=New England Journal of Medicine|issue=9|doi=10.1056/nejmoa1008862|volume=364|pages=829–841|issn=0028-4793}}</ref> |
|||
糖化血色素(HbA1c)每增加1%會增加16%心衰竭發生率<ref>{{Cite journal|title=Why are we doing cardiovascular outcome trials in type 2 diabetes?|url=http://dx.doi.org/10.3949/ccjm.81gr.14005|last=MENON|first=V.|last2=AGGARWAL|first2=B.|date=2014-11-01|journal=Cleveland Clinic Journal of Medicine|issue=11|doi=10.3949/ccjm.81gr.14005|volume=81|pages=665–671|issn=0891-1150}}</ref>,近15%的糖友合併有心衰竭<ref>{{Cite journal|title=Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017|url=https://cardiab.biomedcentral.com/articles/10.1186/s12933-018-0728-6|last=Einarson|first=Thomas R.|last2=Acs|first2=Annabel|date=2018-12|journal=Cardiovascular Diabetology|issue=1|doi=10.1186/s12933-018-0728-6|volume=17|pages=83|language=en|issn=1475-2840|pmc=PMC5994068|pmid=29884191|last3=Ludwig|first3=Craig|last4=Panton|first4=Ulrik H.}}</ref>,增加60-80%心血管死亡風險。<ref>{{Cite web|title=Supplementary file 8. Summary of published reports of LFY function in a range of angiosperm species.|url=http://dx.doi.org/10.7554/elife.39625.034|accessdate=2020-02-26|work=dx.doi.org}}</ref>男性心衰竭比例高2.5倍,女性心衰竭比例高4.1倍<ref>{{Cite journal|title=Risk of heart failure in a population with type 2 diabetes versus a population without diabetes with and without coronary heart disease|url=http://dx.doi.org/10.1111/dom.13493|last=Chen|first=Hua-Fen|last2=Ho|first2=Ching-An|date=2018-09-04|journal=Diabetes, Obesity and Metabolism|issue=1|doi=10.1111/dom.13493|volume=21|pages=112–119|issn=1462-8902|last3=Li|first3=Chung-Yi}}</ref>,30%-50%心衰竭患者有糖尿病<ref>{{Cite journal|title=Oxygenation of frog gastric mucosa in vitro|url=https://www.ncbi.nlm.nih.gov/pubmed/2018|last=Kidder|first=G. W.|last2=Montgomery|first2=C. W.|date=1975-12|journal=The American Journal of Physiology|issue=6|doi=10.1152/ajplegacy.1975.229.6.1510|volume=229|pages=1510–1513|issn=0002-9513|pmid=2018}}</ref>,五年存活率僅剩12.5%<ref>{{Cite web|title=Figure 2—source data 1. Quantification of RyR organization using 150 vs 100 nm CRU inclusion criteria.|url=http://dx.doi.org/10.7554/elife.39427.006|accessdate=2020-02-26|work=dx.doi.org}}</ref>。約10%的第二型糖尿病友會發生腎病變(約20萬人),40%末期腎臟疾病原因來自於糖尿病。<ref>{{Cite journal|title=Excerpts From the US Renal Data System 2009 Annual Data Report|url=http://dx.doi.org/10.1053/j.ajkd.2009.10.009|last=Collins|first=Allan J.|last2=Foley|first2=Robert N.|date=2010-01|journal=American Journal of Kidney Diseases|issue=1|doi=10.1053/j.ajkd.2009.10.009|volume=55|pages=A6–A7|issn=0272-6386|last3=Herzog|first3=Charles|last4=Chavers|first4=Blanche M.|last5=Gilbertson|first5=David|last6=Ishani|first6=Areef|last7=Kasiske|first7=Bertram L.|last8=Liu|first8=Jiannong|last9=Mau|first9=Lih-Wen}}</ref> |
|||
糖尿病血管併發症可分為小血管併發症 (microvascular complications) 及大血併發症 (macrovascular complications)且隨著併發症逐漸加重常會導致患的器官/身體功能的喪失。<ref>{{Cite journal|title=Management of Diabetes in the Elderly|url=http://dx.doi.org/10.1016/j.mcna.2014.11.008|last=Bansal|first=Nidhi|last2=Dhaliwal|first2=Ruban|date=2015-03|journal=Medical Clinics of North America|issue=2|doi=10.1016/j.mcna.2014.11.008|volume=99|pages=351–377|issn=0025-7125|last3=Weinstock|first3=Ruth S.}}</ref> |
|||
第二型糖尿病人的血脂異常特徵為,三酸甘油脂酯 (triglyceride, TG) 增高、高密度脂蛋白膽固醇 (high-densitylipoprotein cholesterol, HDL-C) 下降,低密度脂蛋白膽固醇 (low-density lipoproteincholesterol, LDL-C) 略上升<ref>{{Cite journal|title=Evidence-based diabetes care for older people with Type 2 diabetes: a critical review|url=http://dx.doi.org/10.1111/dme.13859|last=Sinclair|first=A. J.|last2=Abdelhafiz|first2=A. H.|date=2018-11-29|journal=Diabetic Medicine|issue=4|doi=10.1111/dme.13859|volume=36|pages=399–413|issn=0742-3071|last3=Forbes|first3=A.|last4=Munshi|first4=M.}}</ref>。HDL-C 下降,會增加糖尿病老年患者的心血管疾病及缺血性中風 (ischemic stroke) 風險<ref>{{Cite journal|title=Low HDL Cholesterol Is Associated With the Risk of Stroke in Elderly Diabetic Individuals: Changes in the risk for atherosclerotic diseases at various ages|url=http://dx.doi.org/10.2337/dc08-1677|last=Hayashi|first=T.|last2=Kawashima|first2=S.|date=2009-06-09|journal=Diabetes Care|issue=7|doi=10.2337/dc08-1677|volume=32|pages=1221–1223|issn=0149-5992|last3=Itoh|first3=H.|last4=Yamada|first4=N.|last5=Sone|first5=H.|last6=Watanabe|first6=H.|last7=Hattori|first7=Y.|last8=Ohrui|first8=T.|last9=Yokote|first9=K.}}</ref>。 |
|||
高血壓 (hypertension) 是在糖尿病很常見的共病症,相較於非糖尿病患者族群,糖尿病族群的高血壓發生率可高出1.5–3 倍之多。<ref>{{Cite journal|title=The Treatment of Hypertension in Adult Patients With Diabetes|url=http://dx.doi.org/10.2337/diacare.25.1.134|last=Arauz-Pacheco|first=C.|last2=Parrott|first2=M. A.|date=2002-01-01|journal=Diabetes Care|issue=1|doi=10.2337/diacare.25.1.134|volume=25|pages=134–147|issn=0149-5992|last3=Raskin|first3=P.}}</ref>約有 6–8 成的糖尿病患者死於心血管併發症,而這些心血管併發症的發生有高達 75% 可以歸咎於高血壓所造成<ref>{{Cite journal|title=Diabetes Mellitus and Associated Hypertension, Vascular Disease, and Nephropathy|url=http://dx.doi.org/10.1161/01.hyp.26.6.869|last=Sowers|first=James R.|last2=Epstein|first2=Murray|date=1995-12|journal=Hypertension|issue=6|doi=10.1161/01.hyp.26.6.869|volume=26|pages=869–879|issn=0194-911X}}</ref>。除了心血管併發症,與高血壓相關的糖尿病併發症還包括了腎臟病變、視網膜病變、中風等<ref>{{Cite journal|title=Evidence-based diabetes care for older people with Type 2 diabetes: a critical review|url=http://dx.doi.org/10.1111/dme.13859|last=Sinclair|first=A. J.|last2=Abdelhafiz|first2=A. H.|date=2018-11-29|journal=Diabetic Medicine|issue=4|doi=10.1111/dme.13859|volume=36|pages=399–413|issn=0742-3071|last3=Forbes|first3=A.|last4=Munshi|first4=M.}}</ref>。 |
|||
==病因== |
==病因== |
||
2020年2月26日 (三) 08:11的版本
| 2型糖尿病 | |
|---|---|
| 同义词 | 非胰島素依賴型糖尿病(Noninsulin-dependent diabetes mellitus,NIDDM) 成人糖尿病(adult-onset diabetes)[1] |
 | |
| 空心蓝圈為糖尿病的國際象徵符號[2] | |
| 读音 | |
| 症状 | 煩渴、多尿症、不明原因體重下降、多食症[3] |
| 併發症 | 高渗性高血糖状态、糖尿病酮症酸中毒、心血管疾病、中風、糖尿病视网膜病变、腎功能衰竭、截肢[1][4][5] |
| 常見始發於 | 中年或老年[6] |
| 病程 | 終身[6] |
| 类型 | 糖尿病、疾病 |
| 肇因 | 肥胖症、缺乏運動、遺傳[1][6] |
| 診斷方法 | 血糖測量[3] |
| 預防 | 維持正常體重、體能鍛煉、均衡飲食[1] |
| 治療 | 飲食調整、二甲双胍、胰島素、代謝手術[1][7][8][9] |
| 预后 | 预期寿命縮短約10年[10] |
| 盛行率 | 3.92億(2015年)[11] |
| 分类和外部资源 | |
| 醫學專科 | 內分泌學 |
| ICD-11 | 5A11 |
| ICD-10 | E11 |
| OMIM | 125853、601283、601407、603694、608036 |
| DiseasesDB | 3661 |
| MedlinePlus | 000313 |
| eMedicine | 117853 |
| Orphanet | 181376、181376 |
2型糖尿病(英語:Diabetes mellitus type 2,简称T2DM,台湾称为第二型糖尿病),大陆旧称為非胰岛素依赖型糖尿病(英語:noninsulin-dependent diabetes mellitus,简称NIDDM)或成人发病型糖尿病(adult-onset diabetes),是一种慢性代謝疾病,患者特徵為高血糖、相對缺乏胰島素、有胰島素抗性等[6]。常見症狀有煩渴、頻尿、不明原因的體重減輕[3] ,可能還包括多食、疲倦、或有治不好的痠痛[3],以上症狀通常會慢慢出現[6]。高血糖帶來的長期併發症包括心臟病、中風、糖尿病視網膜病變,這可能導致失明、腎臟衰竭、甚至四肢血流不順而需要截肢[1] ;第二型糖尿病患者可能突然發生高渗性高血糖状态,但卻不太會併發糖尿病酮酸血症[4][5]。
第二型糖尿病主要發生在肥胖而又缺乏運動的人[1],具有先天基因遺傳者風險也較高[6]。2型糖尿病佔了糖尿病患者約九成的病例,另外一成為第一型糖尿病及妊娠糖尿病患者[1]。一型糖尿病患者因胰臟β細胞遭自體免疫破壞,而有絕對性胰島素缺乏的問題[12][13]。糖尿病確診需經由血液檢查而定,如檢測空腹血糖值、口服葡萄糖耐量試驗(OGTT)或檢測糖化血紅蛋白(HbA1c)[3]。
部分的第二型糖尿病可經由保持正常體重、規律運動及適當飲食來預防[1],治療方式有運動和改變飲食等[1]。如果沒有經常性血糖偏低,建議的治療藥物為二甲双胍[7][14],但許多患者最終都必須使用胰島素治療[9]。使用胰島素的患者必須定期測量血糖,口服降血糖藥的患者則不一定需要[15]。對肥胖的患者而言,接受减肥手术對改善糖尿病亦十分有效[8][16]。
自1960年起,第二型糖尿病病例就隨著肥胖率逐漸升高[17]。1985年時全球僅有約3000萬人罹患糖尿病,到了2015年患者增至3.92億人[11][18]。糖尿病好發於中高齡層[6],但現今青年人罹患2型糖尿病的比率逐漸增加[19][20]。第二型糖尿病患者可能減損長達約十年的壽命[10]。糖尿病是最早被描述的疾病之一[21],1920年代科學家就發現了胰島素對它的重要性[22]。
病征与症状
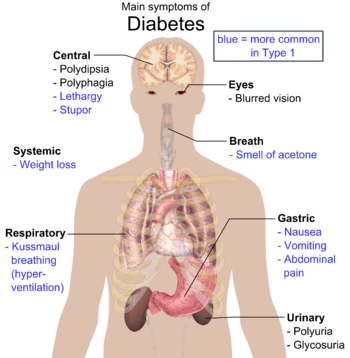
糖尿病的典型症状为多尿症、煩渴、多食症(Polyphagia)以及体重减轻[23]。诊断时其他常见的症状包括視野模糊、皮肤瘙痒、周围神经病变、反复阴道炎、疲劳等病史[13]。然而,很多人在最初数年间不会出现病征,一般在常规体检中才被诊断出来[13]。在少部分的患者會出現高渗性高血糖状态,此類患者會產生高血糖伴有意识水平下降,以及低血压的病况[13]。
併发症
2型糖尿病是慢性疾病,患者的预期寿命可减少長達10年[10]。导致预期寿命减少的部分原因是相关的并发症,包括:患上心血管疾病的风险是健康人群的二至四倍,其中包括缺血性心脏病及中风等等。下肢截肢率會增加20倍,住院率亦相对增高[10]。在发达国家及越来越多的其他地区里,2型糖尿病是导致非创伤性失明及肾衰竭的首要原因[24]。在发病过程中,患者罹患认知功能障碍及失智症风险也会增高,如阿兹海默病及血管性痴呆等等[25]。其他并发症還包括黑棘皮症、性功能障碍,以及容易发生感染[23]。
糖尿病患相較於正常族群會增加2到4倍的心血管疾病風險,約32%的糖友合併有心血管疾病。[26]心血管疾病是全世界糖尿病患者最重要的併發症及主要死因,近6成的糖尿病患者死於心血管疾病。[27]
糖化血色素(HbA1c)每增加1%會增加16%心衰竭發生率[28],近15%的糖友合併有心衰竭[29],增加60-80%心血管死亡風險。[30]男性心衰竭比例高2.5倍,女性心衰竭比例高4.1倍[31],30%-50%心衰竭患者有糖尿病[32],五年存活率僅剩12.5%[33]。約10%的第二型糖尿病友會發生腎病變(約20萬人),40%末期腎臟疾病原因來自於糖尿病。[34]
糖尿病血管併發症可分為小血管併發症 (microvascular complications) 及大血併發症 (macrovascular complications)且隨著併發症逐漸加重常會導致患的器官/身體功能的喪失。[35]
第二型糖尿病人的血脂異常特徵為,三酸甘油脂酯 (triglyceride, TG) 增高、高密度脂蛋白膽固醇 (high-densitylipoprotein cholesterol, HDL-C) 下降,低密度脂蛋白膽固醇 (low-density lipoproteincholesterol, LDL-C) 略上升[36]。HDL-C 下降,會增加糖尿病老年患者的心血管疾病及缺血性中風 (ischemic stroke) 風險[37]。
高血壓 (hypertension) 是在糖尿病很常見的共病症,相較於非糖尿病患者族群,糖尿病族群的高血壓發生率可高出1.5–3 倍之多。[38]約有 6–8 成的糖尿病患者死於心血管併發症,而這些心血管併發症的發生有高達 75% 可以歸咎於高血壓所造成[39]。除了心血管併發症,與高血壓相關的糖尿病併發症還包括了腎臟病變、視網膜病變、中風等[40]。
病因
2型糖尿病的發生與患者的生活方式与遗传因素有關[24][41]。有些因素如饮食习惯和肥胖症等是人为可控制的,但其他如年纪增长、性别为女性、遗传等因素则不然[10]。睡眠不足也与2型糖尿病有关[42],因為睡眠不足会使致身体的新陈代谢有所改变,進而诱发2型糖尿病[42]。孕妇在胎儿发育过程中的营养状况對胎兒未來罹患糖尿病的機率也佔有一席之地,其中DNA甲基化改變是造成此種影響的可能機制之一[43]。此外,腸道細菌如腸道普氏菌(Prevotella copri)和普通擬桿菌(Bacteroides vulgatus)也可能和2型糖尿病有關[44]。
生活方式
目前認為有不少生活方式都是引致2型糖尿病的重要因素,其中包括肥胖症和超重(BMI高于25)、身體活动量不足、不健康的飲食、压力過大以及城市化的生活等[10]。30%的華裔與日裔患者體脂過高,欧裔和非裔患者則有60%至80%,印第安人和太平洋岛民患者則100%都體脂過高[13]。至於非肥胖症的2型糖尿病患則常有過高的腰臀比[13]。吸菸似乎也會增加罹患2型糖尿病的機會[45]。
饮食也是影响2型糖尿病发病风险的重要因素。饮用过量的含糖饮料可增加患病风险[46][47]。饮食裡摄取的脂肪也是很重要的因素,饱和脂肪与反式脂肪均會增加患病风险,而多元不饱和脂肪与单元不饱和脂肪則有助於降低风险[41]。攝取大量白米似乎也会使致病风险增加[48]。也有學者相信,7%的病例可能是缺乏运动所致[49]。持久性有機污染物可能也和糖尿病相關[50]。
遗传因素
大多数糖尿病个案涉及多種基因,而这些不同的基因都可能会使患上2型糖尿病的几率上升[10]。如果同卵双胞胎的其中一人有糖尿病,另一人患上糖尿病的机会高于90%,然而非同卵的兄弟姐妹的几率只有25%至50%[13]。到2011年为止,共发现了超过36个基因都可能增加罹患2型糖尿病的风险[51]。然而,即使全部这些基因加在一起,亦只占诱发糖尿病的整体遗传因素中的10%[51]。舉例來說,可使发病风险增加1.5倍的等位基因TCF7L2为常见基因变异中擁有最高风险的基因[13]。多数与糖尿病有关的基因都与β細胞功能有关[13]。
在一部分罕见的糖尿病个案中,发病原因是因单个基因出现异常而引起的(称为单基因型糖尿病或“其他特殊类型糖尿病”)。[13][10]其中包括年輕人成人型糖尿病(简称MODY)、矮妖精貌综合征、Rabson-Mendenhall综合征等等[10]。其中年輕人成人型糖尿病占年轻糖尿病患者个案总和的1%至5%[52]。
健康状况
許多药物和健康问题都会使人較易患糖尿病[53]。這些药物包括:糖皮质激素、噻嗪类利尿剂、β受体阻滞剂、非典型抗精神病药物[54]及他汀类药物[55]。曾患妊娠糖尿病的人患上2型糖尿病的风险较高[23],而其他和2型糖尿病相关的健康问题還包括肢端肥大症、皮质醇增多症、甲状腺功能亢进症、嗜铬细胞瘤及某些癌症如胰高血糖素瘤[53]。另外,睾酮缺乏与2型糖尿病也有很密切的关联[56][57]。
病理生理学
2型糖尿病的病因复杂,对于单一病患而言,难以确认引发疾病的原因,往往环境和遗传因素中的一种或者多种均有可能与发病相关[58]。胰岛β细胞功能失常和胰岛素抵抗引发了2型糖尿病[59]:尽管在1980年代,人们普遍认为仅靠胰岛素抵抗即可引发糖尿病,但后来的研究表明,在没有β细胞功能失常的情况下,糖尿病不可能发生[60]。在这两种症状的程度方面,患者表现出的胰岛素抵抗和相对胰岛素不足的程度有所差异:有些人以胰岛素抵抗为主、轻微的胰岛素分泌缺陷为次;而其他人可能只有轻微的胰岛素抵抗,而以胰岛素分泌不足为主[13]。
在2型糖尿病中,胰岛素抵抗和高血浆胰岛素水平的发生往往先于疾病发生[58]:尽管过去曾认为高胰岛素水平是胰岛素抵抗引起的代偿,但后来的研究表明,血浆中的高胰岛素水平不一定是代偿胰岛素抵抗的后果,亦有可能是产生胰岛素抵抗的原因[61]。再者,在肥胖诱导的炎症等各种因素作用下,胰岛β细胞的生产或者分泌胰岛素的功能受损。[58]
其他可能与2型糖尿病和胰岛素抵抗、胰岛功能受损有关的重要机制還包括:脂肪细胞内脂质的分解增加、对腸泌素的抵抗或缺乏、血液中胰高血糖素水平过高、肾脏积蓄的盐份和水份上升,及中枢神经系统的代谢調節異常[10]。
胰岛素抵抗
胰岛素抵抗被认为是2型糖尿病的主要特征之一[59]。在胰岛素抵抗的情况下,应当对胰岛素进行响应的组织或器官(如肌肉、肝脏及脂肪组织)无法对正常濃度的胰岛素作出适当响应[62]——例如:具体到肝脏而言,指的是肝脏无法正常响应胰岛素信号,致使糖原分解和葡萄糖异生不能被抑制,血糖被不当增加[63];具体到肌肉而言,指的是肌肉组织无法无法正常响应胰岛素信号,致使肌肉吸收的血糖减少,血糖下降变缓[64]。并不只有葡萄糖在这一过程受到影响:2型糖尿病患者的肝脏和肌肉常见异位脂肪沉积,其氧化过程和葡萄糖形成底物竞争,抑制了葡萄糖的氧化,亦被用来解释胰岛素抵抗的形成。此类的脂肪累积早于2型糖尿病的发病。[65]
动物实验显示,单独的胰岛素抵抗并不一定引起糖尿病:消耗大量能量的大脑和肌肉之中存在的胰岛素抵抗并未在引起胰岛素抵抗,有鉴于此,肝脏和胰岛中的胰岛素抵抗可能是借由其它途径诱导。双基因敲除则提示胰岛素抵抗的多基因型,如IRS-1和GK双基因敲除可以诱导小鼠糖尿病,而单基因敲除不能。胰岛素抵抗往往会与高血压、高血脂等心血管风险因子聚集,形成所谓的“代谢综合征”。[58]
β细胞功能异常
然而,并非所有出现胰岛素抵抗的人士都会患上糖尿病,患者的胰岛β细胞需同時有胰岛素分泌障碍時才会发病[13]。胰岛β细胞功能失常是1型糖尿病和2型糖尿病的共同特征之一,但在2型糖尿病中,胰岛功能常常被忽视。2型糖尿病中的β细胞功能下降往往在糖类不耐受发生以前就已经发生[59]。确诊时,胰岛功能通常已经是正常水平的三成左右;英国前瞻性糖尿病研究中显示,胰岛的功能衰减无法透过饮食,磺脲类、二甲双胍或胰岛素治疗等单一治疗手段进行控制[66]。
1型糖尿病的胰岛素分泌不足主要是因为自体免疫引起的β细胞死亡,而2型糖尿病中的β细胞功能下降或者死亡的原因则较为复杂,与氧化应激、炎症等相关[59]。如以脂质毒性的角度而言,在肝脏和肌肉中异位累积的过量脂肪难以被有效氧化,透过非氧化途径生成反应性脂肪,诱导脂质的凋亡亦纠正脂肪过载的情形;在这一过程生成的神经酰胺等物质可介导胰腺细胞的衰亡[65]。由于饮食和遗传因素等原因,亚裔群体,特别是印度人,易于产生在器官内累积大量脂肪的腹部肥胖;尽管亚裔人群较西方群体纤瘦,也有较高的糖尿病流行率可能与之相关[67][68]。但这一过程不仅仅和脂质毒性有关,还和糖类引发的氧化应激有关[69]:过量的糖类与脂质在能量循环中会形成竞争,糖类的氧化往往受到抑制[70]。
诊断
| 条件 | 餐后两小时血糖 | 空腹血糖 | HbA1c |
|---|---|---|---|
| mmol/l(mg/dl) | mmol/l(mg/dl) | % | |
| 正常 | <7.8(<140) | <6.1(<100) | <5.7 |
| 空腹血糖障碍 | <7.8(<140) | ≥6.1(≥100)& <7.0(<126) | 5.7–6.4 |
| 糖耐量受损 | ≥7.8(≥140) | <7.0(<126) | 5.7–6.4 |
| 糖尿病 | ≥11.1(≥200) | ≥7.0(≥126) | ≥6.5 |
世界卫生组织定义糖尿病(包括1型和2型)为有症状之单次血糖值上升,或两次血糖值上升達到以下標準[73]:
- 空腹血糖≥7.0 mmol/l(126 mg/dl)
- 或
- 作出糖耐力测试,口服两小时之后,血糖≥11.1 mmol/l(200 mg/dl)。
随机血糖高于11.1 mmol/l (200 mg/dl )且出現典型症狀[23]或糖化血红蛋白(HbA1c)高于6.5%是也一种诊断糖尿病的方法[10]。2009年,一个由美国糖尿病协会(American Diabetes Association,简称ADA)、国际糖尿病联合会(International Diabetes Federation,简称IDF)和欧洲糖尿病研究协会(European Association for the Study of Diabetes,简称EASD)之專家代表組成的国际专家委员会建议糖尿病诊断应使用48 mmol/mol作為臨界值(相當於 HbA1c 6.5%)[74],美国糖尿病协会于2010年采用此建议[75]。只有病患出现典型症状和血糖>11.1 mmol/l(>200 mg/dl)才应该重复进行阳性检验[74]。
糖尿病診斷之临界阈根據的是糖耐力测试、空腹血糖或HbA1c,和并发症(如視網膜病變)的关系[10]。比起糖耐力测试,空腹或随机血糖因为比较方便而被廣泛使用[10]。HbA1c的优点是不需禁食且结果较稳定,但缺点是检验较血糖测量昂贵[76]。估计美國有20%的糖尿患者不知道自己患有糖尿病[10]。
2型糖尿病的特征是在胰岛素抵抗或胰岛素相對缺乏所造成的高血糖[77],这与1型糖尿病中的绝对胰岛素缺乏大不相同,後者是因為胰岛细胞损坏所導致的。而妊娠期糖尿病則是在懷孕時新發生的高血糖[13]。1型和2型糖尿病通常可以根据臨床表現来区分[74]。如果对诊断存在疑问,抗体试验可能有助于判定1型糖尿病,C-胜肽水平则有助于判定2型糖尿病[78]。
筛檢
由于没有证据证明大規模糖尿病篩檢可改善最终结果,因此没有大型組織或部门建议进行全面篩檢[79][80]。美國預防服務任務小組(USPSTF)建议对没有症状且血压高于 135/80 毫米水银柱的成年人进行筛檢[81]。对于血压较低的人,并没有充分证据顯示能夠降低此群體的風險和死亡率[81][80]。USPSTF也建議40至70歲之間的過重者進行篩檢[82]。
世界卫生组织(WHO)和USPSTF皆建議高風險者進行篩檢[79][83]。在美國,高風險者包含年齡超過45歲、一等親(包含手足)有糖尿病、部分族裔(如拉美裔、非裔,以及美洲原住民)、有妊娠糖尿病或多囊卵巢綜合症病史、過重,或是患有代謝症候群等等[23]。美國糖尿病學會建議BMI超過25者進行篩檢(亞裔則建議23以上就應該篩檢)[84]。
预防
适当营养和经常运动可以延缓或防止2型糖尿病的发病[85][86],強力的執行生活方式控制可以降低超過一半的風險[24][87]。無論原始體重多寡或后来的体重是否减轻,运动皆有益处[88]。但单靠調整饮食便能降低風險的证据卻十分有限[89],一些证据支持多攝取綠色蔬菜[90],也有一些证据支持限制含糖饮料[46]。对于葡萄糖耐受不良的人士,只改变饮食习惯和运动,或同時使用二甲双胍或阿拉伯糖,可以降低罹患糖尿病的风险[24][91],改变生活方式比服用二甲双胍还有效[24]。一份2017年的回顧文獻指出,長期的生活方式改造能降低28%罹病風險,但糖尿病藥物在停藥後將無助於減低風險[92]。血中的維生素D含量較低會增加糖尿病的風險,但口服補充維生素D3無法改善罹病風險[93]。
管理
2型糖尿病的疾病管理着重于調整生活型態、减低其他心血管风险因素,以及將血糖維持在正常值[24]。英国國民保健署建议2型糖尿病初诊人士进行血糖自我监测[94],但是对于没有使用多剂量胰岛素的人士,自我监测的益处仍有爭議[24][95]。管理其他心血管风险因素如高血压、高胆固醇和微量白蛋白尿能改善预期餘命[24]。將收縮壓控制於 140 mmHg 以下能夠降低死亡風險,並改善預後[96],更高積極的血壓管理(低于130/80 mmHg)相較於標準血壓管理(140/85–100 mmHg)雖能使中风风险轻微减低,但对总体死亡风险并没有影响[97]。
相对于标准血糖控制(HbA1C7-7.9%),更積極的血糖控制(HbA1C<6%)似乎并未改善死亡率[98][99]。2型糖尿病的治疗目标通常是HbA1C低于7%至8%或空腹血糖低于7.2 mmol/L(130 mg/dl);但若將低血糖症和预期餘命等特定风险納入考量,这些目标在专业临床会诊后可以改变[100][101]。儘管臨床指引建議醫師須衡量血糖控制的長期好處和立即傷害,許多人仍被過度治療,例如對預期餘命小於9年的患者進行強化血糖控制便沒有好處[102]。
所有患有2型糖尿病的人士都應定期进行眼科检查[13]。有限的證據顯示以刮除牙結石和牙根整平術治療牙周病或許可以短期改善糖尿病患者的血糖[103],但沒有證據顯示這樣的改善能持續超過4個月[103]。目前並沒有證據表示治療牙周病的藥物有助於改善血糖[103]。
生活方式
适当的饮食和运动是糖尿病治疗的基础[23],运动量越充足效果越佳[104]。運動能改善血糖控制,降低體脂和血脂,這些效果即使在沒有體重減輕的情形下也都有證據支持[105]。有氧运动可使HbA1c下降并改善胰岛素敏感性[106]。阻力训练也有改善的效果,若能同時進行有氧運動及阻力训练效果尤佳[106]。
能促進減重的飲食調整相當重要[107]。目前最理想的飲食配方為何仍有爭議[107],但目前已知低升糖指數飲食或低碳水化合物飲食可以改善血糖[108][109]。在第二型糖尿病發病後短時間內開始超低卡路里飲食能使疾病緩解[110]。素食者相對來說罹患糖尿病的機會較低,但葷食攝取適量者效果則與素食無異[111]。目前尚無證據支持肉桂可以改善第二型糖尿病患者的血糖[112]。
適當的衛教也能協助患者控制血糖,效果最佳可維持到24個月[113]。若輕度糖尿病患者的血糖無法藉由調整生活型態改善,則可能需要考慮配合藥物治療[23]。目前仍尚無足夠證據說明調整生活型態對於患者死亡率的影響[87]。
药物

目前有几类抗糖尿病药。由于有证据表明二甲双胍(metformin)可降低死亡率,因此通常将其作為第一线治疗药物[7][24][114]。然而目前有關此議結論仍有疑問[115],且並非所有第二線糖尿病患者都能一體適用,如具有嚴重腎臟或肝臟疾病者,不應使用二甲双胍[23]。
如二甲双胍不足以控制病情,则可使用另一个类的口服制剂或注射胰島素辅助控制[100]。其他类别的药物包括有磺酰脲类(sulfonylureas)、噻唑烷二酮类药物(thiazolidinedione)、DPP-4抑制剂、SGLT2抑制剂以及GLP-1类似物等[100]。截至2015年為止,目前研究仍無法表明不同製劑間的效果是否有顯著差異[100]。一份2018年的回顧性文章表示SGLT2抑制剂的效果優於GLP-1类似物及DDP-4抑制剂[116]。
罗格列酮(Rosiglitazone)為一種噻唑烷二酮类药物,該藥物被發現可以改善長期預後,並可以改善血糖值[117],但同時他也有導致心臟疾病的風險[118]。血管紧张肽I转化酶抑制剂(ACEIs)可以預防腎臟疾病,並可以改善糖尿病的預後[119][120]。但類似藥物血管紧张素II受体拮抗剂(ARBs)則無此效果[120]。一份2016年的回顧性文章指出糖尿病患者的血壓最好控制於140至150 mmHg之間[121]。
胰岛素可以單獨使用,也可以配合其他口服藥劑一起使用[24],大多数人最初都无需注射胰岛素[13]。当使用时,通常在夜间采用一种长效制剂,同时继续口服药物[23][24]。劑量會過一段時間才起效,達到控制血糖的效果[24]。当夜间胰岛素不足,每日两次胰岛素可达到更好的控制[23]。长效胰岛素,甘精胰岛素(glargine)和地特胰岛素效果及安全性相同[122],其效果並不優於中效胰岛素(NPH insulin),且價格又較貴,因此截至2010年的研究並無發現其實質效益[123]。对于怀孕的患者,胰岛素通常是治疗选择[23]。
補充维生素D可能也可以改善胰島素阻抗的問題,以及降低HbA1c[124]。
外科手术
对于超重的患者,代謝手術(减肥手术)是治疗糖尿病的有效措施[125]。许多人手术后,能够维持正常的血糖水平并服用很少或根本不服用药物[126],且长期死亡率也會降低了[127]。不过仍存在低于1%的短期手术死亡风险[128]。目前建議身高體重指數(BMI)大於35的糖尿病患者進行代謝手術[129][130]。BMI介於30-35之間的若血糖控制不佳或有高度胰島素阻抗者,也建議進行[129][130]。
流行病学

2015年,全球2型糖尿病患者約有3.92亿人,占糖尿病患者的90%[10][11],約相当于世界成人人口的6%[11]。糖尿病是已開發國家和发展中国家常见的疾病[10]。在经济欠发达地区仍然相當罕见[13]。
女性在某些族裔中似乎罹病風險較高[10][131],如南亚裔、太平洋岛民(Pacific Islander)、拉美裔(Latino),和美洲原住民等族裔群体似乎有更高的患病风险[23]。这可能是由于這些群体对西方的生活方式更为敏感[132]。传统上,2型糖尿病歸類為成人疾病,然而随着儿童肥胖率的增加,越来越多的儿童也被诊断罹患2型糖尿病[10]。美国青少年被诊断为2型糖尿病的频率与1型糖尿病同样频繁[13]。
糖尿病患者在1985年的数量估计在3000万,在1995年增至1.36亿,2005年增加至2.17亿[18]。增加的原因主要是全球人口老龄化、运动减少,和肥胖率增加[18]。至2000年為止,糖尿病患者数最多的五个国家是印度(3170万)、中国(2080万)、美国(1770万)、印度尼西亚(840万)和日本(680万)[133]。糖尿病被世界卫生组织确认为一种全球性流行病[1]。
历史
糖尿病是最早被記錄的疾病之一[21],早在公元前约1500年的埃及手稿将其称为“尿液過多”[134]。據信首个有记载的病例被认为是1型糖尿病[134]。同時期,古印度的医生在同期也發現了该病,由於患者的尿液會引來螞蟻,因此將其歸稱为“蜜糖尿”(madhumeha)[134]。而現今所使用的醫學術語「diabetes」一詞源自希臘文的「siphon」(虹吸管),意思是「在彎管中流動」,描述其多尿的症狀。該词是由希腊人孟菲斯之阿波罗尼奥斯(Apollonius of Memphis)在公元前230年首次使用[134]。根據蓋倫的描述,在罗马帝国时期,该病可能属罕见病,在其生涯中僅見兩例[134]。
公元400-500年,印度医生妙聞和揭羅迦首次将1型和2型糖尿病区分开来,认为1型与青年有关,而2型与體重過重有关[134]。“mellitus”一词由英国人约翰·罗尔(John Rolle)于1700年代末期首次使用,用于与频繁排尿的尿崩症相区分[134]。雖然有關糖尿病的紀述相當古老,但该病一直没有有效的治疗。直到20世纪初,加拿大人弗雷德里克·班廷和查尔斯·贝斯特在1921年和1922年发现胰岛素[134]。随后又在1940年代开发出长效NPH胰岛素[134]。
参考文献
- ^ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Diabetes Fact sheet N°312. World Health Organization. August 2011 [2012-01-09]. (原始内容存档于2013-08-26).
- ^ Diabetes Blue Circle Symbol. International Diabetes Federation. 2006-03-17. (原始内容存档于2007年8月5日).
- ^ 3.0 3.1 3.2 3.3 3.4 Diabetes Tests & Diagnosis. National Institute of Diabetes and Digestive and Kidney Diseases. [2017-12-16].
- ^ 4.0 4.1 Pasquel, FJ; Umpierrez, GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment.. Diabetes Care. November 2014, 37 (11): 3124–31. PMC 4207202
 . PMID 25342831. doi:10.2337/dc14-0984.
. PMID 25342831. doi:10.2337/dc14-0984.
- ^ 5.0 5.1 Fasanmade, OA; Odeniyi, IA; Ogbera, AO. Diabetic ketoacidosis: diagnosis and management. African Journal of Medicine and Medical Sciences. June 2008, 37 (2): 99–105. PMID 18939392.
- ^ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Symptoms & Causes of Diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. 2016-11 [2017-12-16].
- ^ 7.0 7.1 7.2 Maruthur, NM; Tseng, E; Hutfless, S; Wilson, LM; Suarez-Cuervo, C; Berger, Z; Chu, Y; Iyoha, E; Segal, JB; Bolen, S. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis. Annals of Internal Medicine. 2016-04-19, 164: 740–51. PMID 27088241. doi:10.7326/M15-2650.
- ^ 8.0 8.1 Cetinkunar, S; Erdem, H; Aktimur, R; Sozen, S. Effect of bariatric surgery on humoral control of metabolic derangements in obese patients with type 2 diabetes mellitus: How it works.. World Journal of Clinical Cases. 2015-06-16, 3 (6): 504–9. PMC 4468896
 . PMID 26090370. doi:10.12998/wjcc.v3.i6.504.
. PMID 26090370. doi:10.12998/wjcc.v3.i6.504.
- ^ 9.0 9.1 Krentz AJ, Bailey CJ. Oral antidiabetic agents: current role in type 2 diabetes mellitus.. Drugs. February 2005, 65 (3): 385–411. PMID 15669880. doi:10.2165/00003495-200565030-00005.
- ^ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 Melmed, Shlomo; Polonsky, Kenneth S.; Larsen, P. Reed; Kronenberg, Henry M. (编). Williams textbook of endocrinology. 12th. Philadelphia: Elsevier/Saunders. : 1371–1435. ISBN 978-1-4377-0324-5.
- ^ 11.0 11.1 11.2 11.3 GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015.. The Lancet. 2016-10-08, 388 (10053): 1545–1602. PMC 5055577
 . PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
. PMID 27733282. doi:10.1016/S0140-6736(16)31678-6.
- ^ MacKay, Ian; Rose, Noel (编). The Autoimmune Diseases. Academic Press. 2014: 575. ISBN 978-0-123-84929-8. OCLC 965646175.
- ^ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 13.12 13.13 13.14 13.15 13.16 Gardner, David G.; Shoback, Dolores (编). Chapter 17: Pancreatic hormones & diabetes mellitus. Greenspan's basic & clinical endocrinology 9th. New York: McGraw-Hill Medical. 2011. ISBN 0-07-162243-8. OCLC 613429053.
- ^ Saenz A, Fernandez-Esteban I, Mataix A, Ausejo M, Roque M, Moher D. Metformin monotherapy for type 2 diabetes mellitus.. Cochrane Database of Systematic Reviews. 2005-07-20, (3): CD002966. PMID 16034881. doi:10.1002/14651858.CD002966.pub3.
- ^ Malanda UL, Welschen LM, Riphagen II, Dekker JM, Nijpels G, Bot SD. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin.. Cochrane Database of Systematic Reviews. 2012-01-18, 1: CD005060. PMID 22258959. doi:10.1002/14651858.CD005060.pub3.
- ^ Ganguly, S; Tan, HC; Lee, PC; Tham, KW. Metabolic bariatric surgery and type 2 diabetes mellitus: an endocrinologist's perspective.. The Journal of Biomedical Research. April 2015, 29 (2): 105–11. PMC 4389109
 . PMID 25859264. doi:10.7555/JBR.29.20140127.
. PMID 25859264. doi:10.7555/JBR.29.20140127.
- ^ Moscou, Susan. Getting the word out: advocacy, social marketing, and policy development and enforcement. Truglio-Londrigan, Marie; Lewenson, Sandra B. (编). Public health nursing: practicing population-based care 2nd. Burlington, MA: Jones & Bartlett Learning. 2013: 317. ISBN 978-1-4496-4660-8. OCLC 758391750.
- ^ 18.0 18.1 18.2 Smyth, S; Heron, A. Diabetes and obesity: the twin epidemics. Nature Medicine. January 2006, 12 (1): 75–80. PMID 16397575. doi:10.1038/nm0106-75.
- ^ Tfayli, H; Arslanian, S. Pathophysiology of type 2 diabetes mellitus in youth: the evolving chameleon. Arquivos Brasileiros de Endocrinologia & Metabologia. March 2009, 53 (2): 165–74. PMC 2846552
 . PMID 19466209. doi:10.1590/s0004-27302009000200008.
. PMID 19466209. doi:10.1590/s0004-27302009000200008.
- ^ Imperatore, Giuseppina; Boyle, James P.; Thompson, Theodore J.; Case, Doug; Dabelea, Dana; Hamman, Richard F.; Lawrence, Jean M.; Liese, Angela D.; Liu, Lenna L. Projections of Type 1 and Type 2 Diabetes Burden in the U.S. Population Aged <20 Years Through 2050. Diabetes Care. December 2012, 35 (12): 2515–2520. ISSN 0149-5992. PMC 3507562
 . PMID 23173134. doi:10.2337/dc12-0669. (原始内容存档于2016-08-14) (英语).
. PMID 23173134. doi:10.2337/dc12-0669. (原始内容存档于2016-08-14) (英语).
- ^ 21.0 21.1 Leutholtz, Brian C.; Ripoll, Ignacio. Diabetes. Exercise and disease management 2nd. Boca Raton: CRC Press. 2011: 25. ISBN 978-1-4398-2759-8. OCLC 725919496.
- ^ Zaccardi F, Webb DR, Yates T, Davies MJ. Pathophysiology of type 1 and type 2 diabetes mellitus: a 90-year perspective.. Postgraduate Medical Journal. February 2016, 92 (1084): 63–9. PMID 26621825. doi:10.1136/postgradmedj-2015-133281.
- ^ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 Vijan, S. Type 2 diabetes. Annals of Internal Medicine. 2010-03-02, 152 (5): ITC31–15; quiz ITC316. PMID 20194231. doi:10.7326/0003-4819-152-5-201003020-01003.
- ^ 24.00 24.01 24.02 24.03 24.04 24.05 24.06 24.07 24.08 24.09 24.10 24.11 Ripsin CM, Kang H, Urban RJ. Management of blood glucose in type 2 diabetes mellitus. American Family Physician. January 2009, 79 (1): 29–36. PMID 19145963.
- ^ Pasquier, F. Diabetes and cognitive impairment: how to evaluate the cognitive status?. Diabetes & Metabolism. October 2010,. 36 Suppl 3: S100–5. PMID 21211730. doi:10.1016/S1262-3636(10)70475-4.
- ^ Einarson, Thomas R.; Acs, Annabel; Ludwig, Craig; Panton, Ulrik H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology. 2018-12, 17 (1): 83. ISSN 1475-2840. PMC 5994068
 . PMID 29884191. doi:10.1186/s12933-018-0728-6 (英语).
. PMID 29884191. doi:10.1186/s12933-018-0728-6 (英语).
- ^ Diabetes Mellitus, Fasting Glucose, and Risk of Cause-Specific Death. New England Journal of Medicine. 2011-03-03, 364 (9): 829–841. ISSN 0028-4793. doi:10.1056/nejmoa1008862.
- ^ MENON, V.; AGGARWAL, B. Why are we doing cardiovascular outcome trials in type 2 diabetes?. Cleveland Clinic Journal of Medicine. 2014-11-01, 81 (11): 665–671. ISSN 0891-1150. doi:10.3949/ccjm.81gr.14005.
- ^ Einarson, Thomas R.; Acs, Annabel; Ludwig, Craig; Panton, Ulrik H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology. 2018-12, 17 (1): 83. ISSN 1475-2840. PMC 5994068
 . PMID 29884191. doi:10.1186/s12933-018-0728-6 (英语).
. PMID 29884191. doi:10.1186/s12933-018-0728-6 (英语).
- ^ Supplementary file 8. Summary of published reports of LFY function in a range of angiosperm species.. dx.doi.org. [2020-02-26].
- ^ Chen, Hua-Fen; Ho, Ching-An; Li, Chung-Yi. Risk of heart failure in a population with type 2 diabetes versus a population without diabetes with and without coronary heart disease. Diabetes, Obesity and Metabolism. 2018-09-04, 21 (1): 112–119. ISSN 1462-8902. doi:10.1111/dom.13493.
- ^ Kidder, G. W.; Montgomery, C. W. Oxygenation of frog gastric mucosa in vitro. The American Journal of Physiology. 1975-12, 229 (6): 1510–1513. ISSN 0002-9513. PMID 2018. doi:10.1152/ajplegacy.1975.229.6.1510.
- ^ Figure 2—source data 1. Quantification of RyR organization using 150 vs 100 nm CRU inclusion criteria.. dx.doi.org. [2020-02-26].
- ^ Collins, Allan J.; Foley, Robert N.; Herzog, Charles; Chavers, Blanche M.; Gilbertson, David; Ishani, Areef; Kasiske, Bertram L.; Liu, Jiannong; Mau, Lih-Wen. Excerpts From the US Renal Data System 2009 Annual Data Report. American Journal of Kidney Diseases. 2010-01, 55 (1): A6–A7. ISSN 0272-6386. doi:10.1053/j.ajkd.2009.10.009.
- ^ Bansal, Nidhi; Dhaliwal, Ruban; Weinstock, Ruth S. Management of Diabetes in the Elderly. Medical Clinics of North America. 2015-03, 99 (2): 351–377. ISSN 0025-7125. doi:10.1016/j.mcna.2014.11.008.
- ^ Sinclair, A. J.; Abdelhafiz, A. H.; Forbes, A.; Munshi, M. Evidence-based diabetes care for older people with Type 2 diabetes: a critical review. Diabetic Medicine. 2018-11-29, 36 (4): 399–413. ISSN 0742-3071. doi:10.1111/dme.13859.
- ^ Hayashi, T.; Kawashima, S.; Itoh, H.; Yamada, N.; Sone, H.; Watanabe, H.; Hattori, Y.; Ohrui, T.; Yokote, K. Low HDL Cholesterol Is Associated With the Risk of Stroke in Elderly Diabetic Individuals: Changes in the risk for atherosclerotic diseases at various ages. Diabetes Care. 2009-06-09, 32 (7): 1221–1223. ISSN 0149-5992. doi:10.2337/dc08-1677.
- ^ Arauz-Pacheco, C.; Parrott, M. A.; Raskin, P. The Treatment of Hypertension in Adult Patients With Diabetes. Diabetes Care. 2002-01-01, 25 (1): 134–147. ISSN 0149-5992. doi:10.2337/diacare.25.1.134.
- ^ Sowers, James R.; Epstein, Murray. Diabetes Mellitus and Associated Hypertension, Vascular Disease, and Nephropathy. Hypertension. 1995-12, 26 (6): 869–879. ISSN 0194-911X. doi:10.1161/01.hyp.26.6.869.
- ^ Sinclair, A. J.; Abdelhafiz, A. H.; Forbes, A.; Munshi, M. Evidence-based diabetes care for older people with Type 2 diabetes: a critical review. Diabetic Medicine. 2018-11-29, 36 (4): 399–413. ISSN 0742-3071. doi:10.1111/dme.13859.
- ^ 41.0 41.1 Risérus U, Willett WC, Hu FB. Dietary fats and prevention of type 2 diabetes. Progress in Lipid Research. January 2009, 48 (1): 44–51. PMC 2654180
 . PMID 19032965. doi:10.1016/j.plipres.2008.10.002.
. PMID 19032965. doi:10.1016/j.plipres.2008.10.002.
- ^ 42.0 42.1 Touma, C; Pannain, S. Does lack of sleep cause diabetes?. Cleveland Clinic journal of medicine. 2011 Aug, 78 (8): 549–58. PMID 21807927. doi:10.3949/ccjm.78a.10165.
- ^ Christian, P; Stewart, CP. Maternal micronutrient deficiency, fetal development, and the risk of chronic disease. The Journal of nutrition. 2010 Mar, 140 (3): 437–45. PMID 20071652. doi:10.3945/jn.109.116327.
- ^ Pedersen HK, Gudmundsdottir V, Nielsen HB, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016-07-21, 535 (7612): 376–381. PMID 27409811. doi:10.1038/nature18646.
- ^ Pan, A; Wang, Y; Talaei, M; Hu, FB; Wu, T. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis.. The Lancet Diabetes & Endocrinology. 2015-09-17, 3: 958–967. PMC 4656094
 . PMID 26388413. doi:10.1016/S2213-8587(15)00316-2.
. PMID 26388413. doi:10.1016/S2213-8587(15)00316-2.
- ^ 46.0 46.1 Malik, VS; Popkin, BM, Bray, GA, Després, JP, Hu, FB. Sugar Sweetened Beverages, Obesity, Type 2 Diabetes and Cardiovascular Disease risk. Circulation. 2010-03-23, 121 (11): 1356–64. PMC 2862465
 . PMID 20308626. doi:10.1161/CIRCULATIONAHA.109.876185.
. PMID 20308626. doi:10.1161/CIRCULATIONAHA.109.876185.
- ^ Malik, VS; Popkin, BM, Bray, GA, Després, JP, Willett, WC, Hu, FB. Sugar-Sweetened Beverages and Risk of Metabolic Syndrome and Type 2 Diabetes: A meta-analysis. Diabetes Care. 2010 Nov, 33 (11): 2477–83. PMC 2963518
 . PMID 20693348. doi:10.2337/dc10-1079.
. PMID 20693348. doi:10.2337/dc10-1079.
- ^ Hu, EA; Pan, A, Malik, V, Sun, Q. White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review. BMJ (Clinical research ed.). 2012-03-15, 344: e1454. PMC 3307808
 . PMID 22422870. doi:10.1136/bmj.e1454.
. PMID 22422870. doi:10.1136/bmj.e1454.
- ^ Lee, I-Min; Shiroma, Eric J; Lobelo, Felipe; Puska, Pekka; Blair, Steven N; Katzmarzyk, Peter T. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet. 2012-07-01. doi:10.1016/S0140-6736(12)61031-9.
- ^ Lind, L; Lind, PM. Can persistent organic pollutants and plastic-associated chemicals cause cardiovascular disease?. Journal of Internal Medicine. Jun 2012, 271 (6): 537–53. PMID 22372998. doi:10.1111/j.1365-2796.2012.02536.x.
- ^ 51.0 51.1 Herder, C; Roden, M. Genetics of type 2 diabetes: pathophysiologic and clinical relevance. European journal of clinical investigation. 2011 Jun, 41 (6): 679–92. PMID 21198561. doi:10.1111/j.1365-2362.2010.02454.x.
- ^ Monogenic Forms of Diabetes: Neonatal Diabetes Mellitus and Maturity-onset Diabetes of the Young. National Diabetes Information Clearinghouse (NDIC) (National Institute of Diabetes and Digestive and Kidney Diseases, NIH). 2007年3月 [2008-08-04]. (原始内容存档于2008-07-04).
- ^ 53.0 53.1 Bethel, edited by Mark N. Feinglos, M. Angelyn. Type 2 diabetes mellitus: an evidence-based approach to practical management. Totowa, NJ: Humana Press. 2008: 462. ISBN 978-1-58829-794-5.
- ^ Izzedine, H; Launay-Vacher, V, Deybach, C, Bourry, E, Barrou, B, Deray, G. Drug-induced diabetes mellitus. Expert opinion on drug safety. 2005 Nov, 4 (6): 1097–109. PMID 16255667. doi:10.1517/14740338.4.6.1097.
- ^ Sampson, UK; Linton, MF, Fazio, S. Are statins diabetogenic?. Current opinion in cardiology. 2011 Jul, 26 (4): 342–7. PMC 3341610
 . PMID 21499090. doi:10.1097/HCO.0b013e3283470359.
. PMID 21499090. doi:10.1097/HCO.0b013e3283470359.
- ^ Saad F, Gooren L. The role of testosterone in the metabolic syndrome: a review. The Journal of Steroid Biochemistry and Molecular Biology. March 2009, 114 (1–2): 40–3. PMID 19444934. doi:10.1016/j.jsbmb.2008.12.022.
- ^ Farrell JB, Deshmukh A, Baghaie AA. Low testosterone and the association with type 2 diabetes. The Diabetes Educator. 2008, 34 (5): 799–806. PMID 18832284. doi:10.1177/0145721708323100.
- ^ 58.0 58.1 58.2 58.3 David K McCulloch; R Paul Robertson,. Pathogenesis of type 2 diabetes mellitus. Uptodate. 2019-10 [2019-11-22].
- ^ 59.0 59.1 59.2 59.3 Saisho, Yoshifumi. β-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World Journal of Diabetes. 2015-02-15, 6 (1): 109–124. ISSN 1948-9358. PMC 4317303
 . PMID 25685282. doi:10.4239/wjd.v6.i1.109.
. PMID 25685282. doi:10.4239/wjd.v6.i1.109.
- ^ Why We Are Fat | BU Today. Boston University. [2019-12-07] (英语).
- ^ Shanik, Michael H.; Xu, Yuping; Škrha, Jan; Dankner, Rachel; Zick, Yehiel; Roth, Jesse. Insulin Resistance and Hyperinsulinemia: Is hyperinsulinemia the cart or the horse?. Diabetes Care. 2008-02-01, 31 (Supplement 2): S262–S268. ISSN 0149-5992. PMID 18227495. doi:10.2337/dc08-s264 (英语).
- ^ Diabetes mellitus a guide to patient care.. Philadelphia: Lippincott Williams & Wilkins. 2007: 15. ISBN 978-1-58255-732-8.
- ^ Meshkani, Reza; Adeli, Khosrow. Hepatic insulin resistance, metabolic syndrome and cardiovascular disease. Clinical Biochemistry. 2009-09-01, 42 (13): 1331–1346. ISSN 0009-9120. doi:10.1016/j.clinbiochem.2009.05.018.
- ^ Turcotte, Lorraine P; Fisher, Jonathan S. Skeletal Muscle Insulin Resistance: Roles of Fatty Acid Metabolism and Exercise. Physical Therapy. 2008-11, 88 (11): 1279–1296. ISSN 0031-9023. PMC 2579902
 . PMID 18801860. doi:10.2522/ptj.20080018.
. PMID 18801860. doi:10.2522/ptj.20080018.
- ^ 65.0 65.1 Taylor, Roy. Causation of Type 2 Diabetes — The Gordian Knot Unravels. New England Journal of Medicine. 2004-02-12, 350 (7): 639–641. ISSN 0028-4793. PMID 14960738. doi:10.1056/NEJMp038239.
- ^ Taylor, Roy. Causation of Type 2 Diabetes — The Gordian Knot Unravels. New England Journal of Medicine. 2004-02-12, 350 (7): 639–641. ISSN 0028-4793. PMID 14960738. doi:10.1056/NEJMp038239.
- ^ Gulati, S.; Misra, A. Abdominal obesity and type 2 diabetes in Asian Indians: dietary strategies including edible oils, cooking practices and sugar intake. European Journal of Clinical Nutrition. 2017-07, 71 (7): 850–857. ISSN 1476-5640. doi:10.1038/ejcn.2017.92 (英语).
- ^ Ramachandran, Ambady; Chamukuttan, Snehalatha; Shetty, Samith A.; Arun, Nanditha; Susairaj, Priscilla. Obesity in Asia – is it different from rest of the world. Diabetes/Metabolism Research and Reviews. 2012, 28 (s2): 47–51. ISSN 1520-7560. doi:10.1002/dmrr.2353 (英语).
- ^ Robertson, R. Paul; Harmon, Jamie; Tran, Phuong Oanh; Tanaka, Yoshito; Takahashi, Hiroki. Glucose Toxicity in β-Cells: Type 2 Diabetes, Good Radicals Gone Bad, and the Glutathione Connection. Diabetes. 2003-03-01, 52 (3): 581–587. ISSN 0012-1797. PMID 12606496. doi:10.2337/diabetes.52.3.581 (英语).
- ^ Hue, Louis; Taegtmeyer, Heinrich. The Randle cycle revisited: a new head for an old hat. American Journal of Physiology - Endocrinology and Metabolism. 2009, 297 (3): E578–E591. ISSN 0193-1849. PMC 2739696
 . PMID 19531645. doi:10.1152/ajpendo.00093.2009.
. PMID 19531645. doi:10.1152/ajpendo.00093.2009.
- ^ Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation (PDF). Geneva: World Health Organization. 2006: 21. ISBN 978-92-4-159493-6.
- ^ Vijan, Sandeep. Type 2 Diabetes. Annals of Internal Medicine. 2010-03-02, 152 (5): ITC3–1. ISSN 0003-4819. PMID 20194231. doi:10.7326/0003-4819-152-5-201003020-01003 (英语).
- ^ World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: Report of a WHO Consultation. Part 1. Diagnosis and classification of diabetes mellitus. [2007-05-29].
- ^ 74.0 74.1 74.2 International Expert, Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009 Jul, 32 (7): 1327–34. PMC 2699715
 . PMID 19502545. doi:10.2337/dc09-9033.
. PMID 19502545. doi:10.2337/dc09-9033.
- ^ Diagnosis and classification of diabetes mellitus. Diabetes Care (American Diabetes Association). January 2010,. 33 Suppl 1 (Supplement_1): S62–9. PMC 2797383
 . PMID 20042775. doi:10.2337/dc10-S062.
. PMID 20042775. doi:10.2337/dc10-S062.
- ^ American Diabetes, Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. January 2012,. 35 Suppl 1: S64–71. PMID 22187472. doi:10.2337/dc12-s064.
- ^ Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Cotran, Ramzi S. ; Robbins, Stanley L. Robbins and Cotran Pathologic Basis of Disease 7th. Philadelphia, Pa.: Saunders. 2005: 1194–1195. ISBN 0-7216-0187-1.
- ^ Diabetes mellitus a guide to patient care.. Philadelphia: Lippincott Williams & Wilkins. 2007: 201. ISBN 978-1-58255-732-8.
- ^ 79.0 79.1 Valdez R. Detecting Undiagnosed Type 2 Diabetes: Family History as a Risk Factor and Screening Tool. Journal of Diabetes Science and Technology. 2009, 3 (4): 722–26. PMC 2769984
 . PMID 20144319. doi:10.1177/193229680900300417.
. PMID 20144319. doi:10.1177/193229680900300417.
- ^ 80.0 80.1 Selph, S; Dana, T; Blazina, I; Bougatsos, C; Patel, H; Chou, R. Screening for Type 2 Diabetes Mellitus: A Systematic Review for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2015-06-22, 162 (11): 765–76. PMID 25867111. doi:10.7326/M14-2221.
- ^ 81.0 81.1 Archived: Diabetes Mellitus (Type 2) in Adults: Screening. U.S. Preventive Services Task Force. June 2008 [2014-03-16]. (原始内容存档于2014-02-07).
- ^ Siu, AL. Screening for Abnormal Blood Glucose and Type 2 Diabetes Mellitus: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2015-10-27, 163 (11): 861–68. PMID 26501513. doi:10.7326/M15-2345.
- ^ Draft Recommendation Statement Screening for Abnormal Glucose and Type 2 Diabetes Mellitus. U.S. Preventive Services Task Force. [2014-10-07]. (原始内容存档于2014年10月9日).
- ^ Standards of Medical Care in Diabetes – 2015: Summary of Revisions. Diabetes Care. 2015, 54 (38): S4. PMID 25537706. doi:10.2337/dc15-S003.
- ^ Raina Elley C, Kenealy T. Lifestyle interventions reduced the long-term risk of diabetes in adults with impaired glucose tolerance. Evid Based Med. December 2008, 13 (6): 173. PMID 19043031. doi:10.1136/ebm.13.6.173.
- ^ Orozco LJ, Buchleitner AM, Gimenez-Perez G, Roqué I Figuls M, Richter B, Mauricio D. Mauricio, Didac , 编. Exercise or exercise and diet for preventing type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008, (3): CD003054. PMID 18646086. doi:10.1002/14651858.CD003054.pub3.
- ^ 87.0 87.1 Schellenberg, ES.; Dryden, DM.; Vandermeer, B.; Ha, C.; Korownyk, C. Lifestyle Interventions for Patients With and at Risk for Type 2 Diabetes: A Systematic Review and Meta-analysis. Annals of Internal Medicine. October 2013, 159 (8): 543–51. PMID 24126648. doi:10.7326/0003-4819-159-8-201310150-00007.
- ^ O'Gorman, DJ; Krook, A. Exercise and the treatment of diabetes and obesity. The Medical clinics of North America. 2011 Sep, 95 (5): 953–69. PMID 21855702. doi:10.1016/j.mcna.2011.06.007.
- ^ Nield L, Summerbell CD, Hooper L, Whittaker V, Moore H. Nield, Lucie , 编. Dietary advice for the prevention of type 2 diabetes mellitus in adults. Cochrane Database Syst Rev. 2008, (3): CD005102. PMID 18646120. doi:10.1002/14651858.CD005102.pub2.
- ^ Carter, P; Gray, LJ, Troughton, J, Khunti, K, Davies, MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ (Clinical research ed.). 2010-08-18, 341: c4229. PMC 2924474
 . PMID 20724400. doi:10.1136/bmj.c4229.
. PMID 20724400. doi:10.1136/bmj.c4229.
- ^ Santaguida PL, Balion C, Hunt D; et al. Diagnosis, prognosis, and treatment of impaired glucose tolerance and impaired fasting glucose (PDF). Evid Rep Technol Assess (Summ). August 2005, (128): 1–11. PMID 16194123. (原始内容 (PDF)存档于2008-09-10).
- ^ Haw, JS; Galaviz, KI; Straus, AN; Kowalski, AJ; Magee, MJ; Weber, MB; Wei, J; Narayan, KMV; Ali, MK. Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Internal Medicine. 2017-11-06, 177 (12): 1808–17. PMID 29114778. doi:10.1001/jamainternmed.2017.6040.
- ^ Seida, Jennifer C.; Mitri, Joanna; Colmers, Isabelle N.; Majumdar, Sumit R.; Davidson, Mayer B.; Edwards, Alun L.; Hanley, David A.; Pittas, Anastassios G.; Tjosvold, Lisa; Johnson, Jeffrey A. Effect of Vitamin D3 Supplementation on Improving Glucose Homeostasis and Preventing Diabetes: A Systematic Review and Meta-Analysis. The Journal of Clinical Endocrinology & Metabolism. Oct 2014, 99 (10): 3551–60. PMC 4483466
 . PMID 25062463. doi:10.1210/jc.2014-2136.
. PMID 25062463. doi:10.1210/jc.2014-2136.
- ^ Type 2 diabetes: The management of type 2 diabetes. May 2009. (原始内容存档于2015-05-22).
- ^ Farmer, AJ; Perera, R; Ward, A; Heneghan, C; Oke, J; Barnett, AH; Davidson, MB; Guerci, B; Coates, V; Schwedes, U; O'Malley, S. Meta-analysis of individual patient data in randomised trials of self monitoring of blood glucose in people with non-insulin treated type 2 diabetes. The BMJ. 27 February 2012, 344: e486. PMID 22371867. doi:10.1136/bmj.e486.
- ^ Emdin, CA; Rahimi, K; Neal, B; Callender, T; Perkovic, V; Patel, A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA: the Journal of the American Medical Association. 10 February 2015, 313 (6): 603–15. PMID 25668264. doi:10.1001/jama.2014.18574.
- ^ McBrien, K; Rabi, DM; Campbell, N; Barnieh, L; Clement, F; Hemmelgarn, BR; Tonelli, M; Leiter, LA; Klarenbach, SW; Manns, BJ. Intensive and Standard Blood Pressure Targets in Patients With Type 2 Diabetes Mellitus: Systematic Review and Meta-analysis. Archives of Internal Medicine. 6 August 2012, 172 (17): 1–8. PMID 22868819. doi:10.1001/archinternmed.2012.3147.
- ^ Boussageon, R; Bejan-Angoulvant, T; Saadatian-Elahi, M; Lafont, S; Bergeonneau, C; Kassaï, B; Erpeldinger, S; Wright, JM; Gueyffier, F; Cornu, C. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. The BMJ. 2011-07-26, 343: d4169. PMC 3144314
 . PMID 21791495. doi:10.1136/bmj.d4169.
. PMID 21791495. doi:10.1136/bmj.d4169.
- ^ Webster, MW. Clinical practice and implications of recent diabetes trials. Current Opinion in Cardiology. July 2011, 26 (4): 288–93. PMID 21577100. doi:10.1097/HCO.0b013e328347b139.
- ^ 100.0 100.1 100.2 100.3 Inzucchi, SE; Bergenstal, RM; Buse, JB; Diamant, M; Ferrannini, E; Nauck, M; Peters, AL; Tsapas, A; Wender, R; Matthews, DR. Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred approach. Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes.. Diabetologia. March 2015, 58 (3): 429–42. PMID 25583541. doi:10.1007/s00125-014-3460-0.
- ^ Qaseem, Amir; Wilt, Timothy J.; Kansagara, Devan; Horwitch, Carrie; Barry, Michael J.; Forciea, Mary Ann. Hemoglobin A Targets for Glycemic Control With Pharmacologic Therapy for Nonpregnant Adults With Type 2 Diabetes Mellitus: A Guidance Statement Update From the American College of Physicians. Annals of Internal Medicine. 6 March 2018. doi:10.7326/M17-0939.
- ^ Makam, AN; Nguyen, OK. An Evidence-Based Medicine Approach to Antihyperglycemic Therapy in Diabetes Mellitus to Overcome Overtreatment.. Circulation. 10 January 2017, 135 (2): 180–95. PMID 28069712. doi:10.1161/CIRCULATIONAHA.116.022622.
- ^ 103.0 103.1 103.2 Simpson, Terry C.; Weldon, Jo C.; Worthington, Helen V.; Needleman, Ian; Wild, Sarah H.; Moles, David R.; Stevenson, Brian; Furness, Susan; Iheozor-Ejiofor, Zipporah. Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database of Systematic Reviews. 2015-11-06, (11): CD004714. ISSN 1469-493X. PMID 26545069. doi:10.1002/14651858.CD004714.pub3.
- ^ Smith, AD; Crippa, A; Woodcock, J; Brage, S. Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies.. Diabetologia. December 2016, 59 (12): 2527–45. PMID 27747395. doi:10.1007/s00125-016-4079-0.
- ^ Thomas, D. E.; Elliott, E. J.; Naughton, G. A. Exercise for type 2 diabetes mellitus. The Cochrane Database of Systematic Reviews. 2006-07-19, (3): CD002968. ISSN 1469-493X. PMID 16855995. doi:10.1002/14651858.CD002968.pub2.
- ^ 106.0 106.1 Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S. Exercise for the management of type 2 diabetes: a review of the evidence (PDF). Acta Diabetologica. March 2010, 47 (1): 15–22. PMID 19495557. doi:10.1007/s00592-009-0126-3.
- ^ 107.0 107.1 Davis N, Forbes B, Wylie-Rosett J. Nutritional strategies in type 2 diabetes mellitus. Mount Sinai Journal of Medicine. June 2009, 76 (3): 257–68. PMID 19421969. doi:10.1002/msj.20118.
- ^ Thomas D, Elliott EJ. Thomas, Diana , 编. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. Cochrane Database of Systematic Reviews. 2009, (1): CD006296. PMID 19160276. doi:10.1002/14651858.CD006296.pub2.
- ^ Feinman, RD; Pogozelski, WK; Astrup, A; Bernstein, RK; Fine, EJ; Westman, EC; Accurso, A; Frassetto, L; Gower, BA; McFarlane, SI; Nielsen, JV; Krarup, T; Saslow, L; Roth, KS; Vernon, MC; Volek, JS; Wilshire, GB; Dahlqvist, A; Sundberg, R; Childers, A; Morrison, K; Manninen, AH; Dashti, HM; Wood, RJ; Wortman, J; Worm, N. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base.. Nutrition (Burbank, Los Angeles County, Calif.). January 2015, 31 (1): 1–13. PMID 25287761. doi:10.1016/j.nut.2014.06.011.
- ^ Clifton, P. Assessing the evidence for weight loss strategies in people with and without type 2 diabetes.. World journal of diabetes. 15 October 2017, 8 (10): 440–454. PMID 29085571. doi:10.4239/wjd.v8.i10.440.
- ^ Glick-Bauer M, Yeh MC. The health advantage of a vegan diet: exploring the gut microbiota connection. Nutrients (Review). 2014, 6 (11): 4822–38. PMC 4245565
 . PMID 25365383. doi:10.3390/nu6114822.
. PMID 25365383. doi:10.3390/nu6114822.
- ^ Leach, Matthew J.; Kumar, Saravana. Cinnamon for diabetes mellitus. Cochrane Database of Systematic Reviews. 2012-09-12, (9): CD007170. ISSN 1469-493X. PMID 22972104. doi:10.1002/14651858.CD007170.pub2.
- ^ Attridge, Madeleine; Creamer, John; Ramsden, Michael; Cannings-John, Rebecca; Hawthorne, Kamila. Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews. 2014-09-04, (9): CD006424. ISSN 1469-493X. PMID 25188210. doi:10.1002/14651858.CD006424.pub3.
- ^ Palmer, Suetonia C.; Mavridis, Dimitris; Nicolucci, Antonio; Johnson, David W.; Tonelli, Marcello; Craig, Jonathan C.; Maggo, Jasjot; Gray, Vanessa; De Berardis, Giorgia; Ruospo, Marinella; Natale, Patrizia; Saglimbene, Valeria; Badve, Sunil V.; Cho, Yeoungjee; Nadeau-Fredette, Annie-Claire; Burke, Michael; Faruque, Labib; Lloyd, Anita; Ahmad, Nasreen; Liu, Yuanchen; Tiv, Sophanny; Wiebe, Natasha; Strippoli, Giovanni F.M. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes. JAMA: the Journal of the American Medical Association. 2016-07-19, 316 (3): 313–24. PMID 27434443. doi:10.1001/jama.2016.9400.
- ^ Boussageon, R; Supper, I; Bejan-Angoulvant, T; Kellou, N; Cucherat, M; Boissel, JP; Kassai, B; Moreau, A; Gueyffier, F; Cornu, C. Groop, Leif , 编. Reappraisal of metformin efficacy in the treatment of type 2 diabetes: a meta-analysis of randomised controlled trials. PLOS Medicine. 2012, 9 (4): e1001204. PMC 3323508
 . PMID 22509138. doi:10.1371/journal.pmed.1001204.
. PMID 22509138. doi:10.1371/journal.pmed.1001204.
- ^ Zheng, Sean L.; Roddick, Alistair J.; Aghar-Jaffar, Rochan; Shun-Shin, Matthew J.; Francis, Darrel; Oliver, Nick; Meeran, Karim. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes. JAMA. 2018-04-17, 319 (15): 1580. doi:10.1001/jama.2018.3024.
- ^ Richter, B; Bandeira-Echtler, E; Bergerhoff, K; Clar, C; Ebrahim, SH. Richter, Bernd , 编. Rosiglitazone for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews. 2007-07-18, (3): CD006063. PMID 17636824. doi:10.1002/14651858.CD006063.pub2.
- ^ Chen, X; Yang, L; Zhai, SD. Risk of cardiovascular disease and all-cause mortality among diabetic patients prescribed rosiglitazone or pioglitazone: a meta-analysis of retrospective cohort studies. Chinese Medical Journal. December 2012, 125 (23): 4301–06. PMID 23217404.
- ^ Lv, J; Perkovic, V; Foote, CV; Craig, ME; Craig, JC; Strippoli, GF. Strippoli, Giovanni FM , 编. Antihypertensive agents for preventing diabetic kidney disease. Cochrane Database of Systematic Reviews. 2012-12-12, 12: CD004136. PMID 23235603. doi:10.1002/14651858.CD004136.pub3.
- ^ 120.0 120.1 Cheng, J; Zhang, W; Zhang, X; Han, F; Li, X; He, X; Li, Q; Chen, J. Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis.. JAMA Internal Medicine. May 2014, 174 (5): 773–85. PMID 24687000. doi:10.1001/jamainternmed.2014.348.
- ^ Brunström, Mattias; Carlberg, Bo. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. The BMJ. 2016-02-24, 352: i717. PMC 4770818
 . PMID 26920333. doi:10.1136/bmj.i717.
. PMID 26920333. doi:10.1136/bmj.i717.
- ^ Swinnen, SG.; Simon, AC.; Holleman, F.; Hoekstra, JB.; Devries, JH. Simon, Airin CR , 编. Insulin detemir versus insulin glargine for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews. 2011, (7): CD006383. PMID 21735405. doi:10.1002/14651858.CD006383.pub2.
- ^ Waugh, N; Cummins, E; Royle, P; Clar, C; Marien, M; Richter, B; Philip, S. Newer agents for blood glucose control in type 2 diabetes: systematic review and economic evaluation. Health Technology Assessment (Winchester, England). July 2010, 14 (36): 1–248. PMID 20646668. doi:10.3310/hta14360.
- ^ Mirhosseini, Naghmeh; Vatanparast, Hassanali; Mazidi, Mohsen; Kimball, Samantha M. The Effect of Improved Serum 25-Hydroxyvitamin D Status on Glycemic Control in Diabetic Patients: A Meta-Analysis. The Journal of Clinical Endocrinology & Metabolism. 2017-09-01, 102 (9): 3097–3110. doi:10.1210/jc.2017-01024.
- ^ Picot, J; Jones, J; Colquitt, JL; Gospodarevskaya, E; Loveman, E; Baxter, L; Clegg, AJ. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technology Assessment (Winchester, England). September 2009, 13 (41): iii–iv, 1–190, 215–357. PMID 19726018. doi:10.3310/hta13410.
- ^ Frachetti, KJ; Goldfine, AB. Bariatric surgery for diabetes management. Current Opinion in Endocrinology, Diabetes and Obesity. April 2009, 16 (2): 119–24. PMID 19276974. doi:10.1097/MED.0b013e32832912e7.
- ^ Schulman, AP; del Genio, F; Sinha, N; Rubino, F. "Metabolic" surgery for treatment of type 2 diabetes mellitus. Endocrine Practice. September–October 2009, 15 (6): 624–31. PMID 19625245. doi:10.4158/EP09170.RAR.
- ^ Colucci, RA. Bariatric surgery in patients with type 2 diabetes: a viable option. Postgraduate Medicine. January 2011, 123 (1): 24–33. PMID 21293081. doi:10.3810/pgm.2011.01.2242.
- ^ 129.0 129.1 Brito, Juan P.; Montori, Victor M.; Davis, Andrew M. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes. JAMA. 2017-02-14, 317 (6): 635–636. ISSN 0098-7484. PMC 5557277
 . PMID 28196240. doi:10.1001/jama.2016.20563.
. PMID 28196240. doi:10.1001/jama.2016.20563.
- ^ 130.0 130.1 Rubino, Francesco; Nathan, David M.; Eckel, Robert H.; Schauer, Philip R.; Alberti, K. George M. M.; Zimmet, Paul Z.; Del Prato, Stefano; Ji, Linong; Sadikot, Shaukat M. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery. July 2016, 12 (6): 1144–1162. ISSN 1878-7533. PMID 27568469. doi:10.1016/j.soard.2016.05.018.
- ^ Abate N, Chandalia M. Ethnicity and type 2 diabetes: focus on Asian Indians. Journal of Diabetes and its Complications. 2001, 15 (6): 320–27. PMID 11711326. doi:10.1016/S1056-8727(01)00161-1.
- ^ Carulli, L; Rondinella, S; Lombardini, S; Canedi, I; Loria, P; Carulli, N. Review article: diabetes, genetics and ethnicity. Alimentary Pharmacology & Therapeutics. November 2005,. 22 Suppl 2: 16–19. PMID 16225465. doi:10.1111/j.1365-2036.2005.02588.x.
- ^ Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. May 2004, 27 (5): 1047–53. PMID 15111519. doi:10.2337/diacare.27.5.1047.
- ^ 134.0 134.1 134.2 134.3 134.4 134.5 134.6 134.7 134.8 Zajac, Jacek; Shrestha, Anil; Patel, Parini; Poretsky, Leonid. The Main Events in the History of Diabetes Mellitus. Poretsky, Leonid (编). Principles of diabetes mellitus 2nd. New York: Springer. 2009: 3–16. ISBN 978-0-387-09840-1. OCLC 663097550.
- 附注
外部链接
| 维基词典上的字词解释 | |
| 维基共享资源上的多媒体资源 | |
| 维基新闻上的新闻 | |
| 维基语录上的名言 | |
| 维基文库上的原始文献 | |
| 维基教科书上的教科书和手册 | |
| 维基学院上的學習资源 | |
- 开放式目录计划中和2型糖尿病相关的内容
- 国家糖尿病信息中心
- 美国疾病控制中心(内分泌病理)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
