泌尿道感染:修订间差异
小 Robot: en wiki 之規範控制 (Authority control) 模板轉移作業 |
醫週譯小時工作成果 |
||
| 第1行: | 第1行: | ||
{{medical}} |
{{medical}} |
||
{{unreferenced|time=2010-07-26}} |
|||
{{DiseaseDisorder infobox |
{{DiseaseDisorder infobox |
||
|Name = 泌尿道感染<br />({{lang|en|Urinary tract infection}}) |
|Name = 泌尿道感染<br />({{lang|en|Urinary tract infection}}) |
||
| 第18行: | 第17行: | ||
}} |
}} |
||
'''泌尿道感染'''({{lang|en|urinary tract infection}},UTI),也稱為急性膀胱炎或膀胱感染,是一種會影響到部分[[泌尿道]]的[[感染]]<ref name="mayoclinic">{{cite web|url=http://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/basics/definition/con-20037892|author=Mayo Clinic Staff|title=Diseases and Conditions - Urinary tract infection (UTI)|publisher=Mayo Clinic|date=August 29, 2012}}</ref>。泌尿道分為上、下泌尿道,感染部位不同對應到不同疾病名稱:當影響到下泌尿道,稱為膀胱炎;當影響到上泌尿道,也就是腎臟的時候,則稱為[[腎盂腎炎]]<ref name=EM2011/>。 |
|||
'''泌尿道感染'''({{lang-en|'''urinary tract infection'''}},缩写{{lang|en|'''UTI'''}})指[[泌尿道]]任何一部份受[[細菌]][[感染]]。雖然[[尿液]]中含有各種液體、[[鹽]]以及廢物,但在健康的膀胱中,尿液是沒有細菌的[http://www.guokr.com/article/438471/]。當細菌進入[[膀胱]]或[[腎臟]]並在尿液中繁殖,便引起尿道炎。最常見的泌尿道感染是膀胱感染,這通常也被稱為[[膀胱炎]]。另一種尿道炎是腎臟感染,稱為[[腎盂腎炎]](pyelonephritis),是比較嚴重的感染。雖然會引起不適,只要及時就醫,泌尿道感染通常是迅速而容易治療的。 |
|||
不同感染位置,症狀會稍有不同:下泌尿道感染的症狀主要是[[解尿]]時會疼痛,也可能會有頻尿或是一直想要解尿的感覺;上泌尿道感染除了會有跟下泌尿道感染同樣症狀外,還會有[[發燒]]、[[腹痛]]的症狀。有些情況,可能沒有解尿也能感受到尿道灼熱痛感。年長者和很年輕的人若感染,以上症狀可能不會表現得十分明顯。最常見造成泌尿道感染(上下都可能)的病菌是[[大腸桿菌]],而其他細菌、[[病毒]]或[[黴菌]]則鮮少造成感染。 |
|||
==症狀== |
|||
=== 膀胱感染 === |
|||
*[[尿急]](urinary urgency) |
|||
*[[頻尿症|尿頻]](urinary frequency),並且在只有少量尿液時仍覺得需要[[尿|排尿]] |
|||
*[[夜尿]](nocturia):需要在夜間排尿。 |
|||
*[[尿道炎]](urethritis):排尿時尿道口感到不適或疼痛,或是整個尿道有燒灼感 |
|||
*[[排尿困難]](dysuria) |
|||
*[[膀胱炎]] |
|||
*[[膿尿]](pyuria):尿液含[[膿]]或尿道排膿 |
|||
*[[血尿]]:尿中帶血 |
|||
*[[發燒]]:輕微發燒 |
|||
*[[尿液]]臭和混濁 |
|||
*[[小便失禁]](urinary incontinence) |
|||
*[[排尿時疼痛或灼熱感]] |
|||
女性其尿道較短,肛門和尿道開口距離也較近,因此較容易有泌尿道感染[中1],約過半數的 女性在其一生中有出現過泌尿道感染的情形。泌尿道感染也常會復發。其他的危險因子還包括性交及家族病史。若有出現腎盂腎炎,可能是因為膀胱感染而引起,但 也可能是因為{{le|菌血症|blood-borne infection}}而造成。若病患是年輕健康的女性,泌尿道感染可以只以其症狀來診斷。針對一些模糊的症狀,會比較不容易診斷,因為可能有些部位已有 細菌存在,只是沒有感染症狀。若是有併發症或是治療不成功的例子,可以進行[[尿液培養]],若頻繁感染,可用低劑量[[抗生素]]進行預防性醫療。 |
|||
=== 腎臟感染 === |
|||
* 上述症狀 |
|||
* [[噁心]] |
|||
* [[嘔吐]] |
|||
* [[背痛]]、[[腰痛]]或[[腹股溝疼痛]] |
|||
* [[腹痛]] |
|||
* 肋脊角不適(Costovertebral angle discomfort) |
|||
* 寒戰及高尖峰發燒(Shaking chills and high spiking fever) |
|||
* 睡覺時出汗 |
|||
* 極度疲勞 |
|||
若是沒有併發症的泌尿道感染,可以用短療程抗生素進行治療,不過不少抗生素已用來治療泌尿 道感染,細菌[[抗生素抗藥性]]也漸漸提高。若是已有併發症,需要長療程的抗生素或是注射抗生素,若症狀在二至三天還沒有改善,需要進一步的诊断测试。 在女性中,泌尿道感染是最常見的細菌感染,每年約會增加10%。若病患在尿液中有病菌或白血球,但沒有症狀,一般不建議使用抗生素,但若病患是已懷孕的婦 女,仍需使用抗生素。 |
|||
==流行病學== |
|||
泌尿道感染最常見於性生活活躍的女性或生育年齡的女性,懷孕婦女、男士前列腺增大、上廁所的習慣差劣、患有[[糖尿病]]或患有[[鐮刀型紅血球疾病]]的人士罹患泌尿道感染的風險也較高。 |
|||
==体征和症状== |
|||
嬰兒、小孩(小於六歲,[[包皮過長]][[包莖]])和小於50歲男性極少出現泌尿道感染,如有則通常和泌尿道結構畸型(膀胱逆流、尿路阻塞)有關。 |
|||
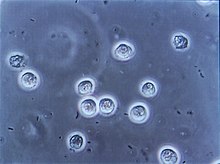
[[File:Pyuria2011.JPG|thumb|Urine may contain pus (a condition known as [[pyuria]]) as seen from a person with [[sepsis]] due to a urinary tract infection.]] |
|||
下泌尿道感染也稱為膀胱感染。最常見的症狀是[[排尿時有灼熱感]]與頻尿(或是有排尿的慾望)伴隨著沒有[[陰道分泌物]]與明顯的疼痛<ref name=Review08/>。這些症狀可能輕微,也可能嚴重<ref name=EM2011>{{cite journal |last1=Lane |first1=DR |author2=Takhar, SS |title=Diagnosis and management of urinary tract infection and pyelonephritis.|journal=Emergency medicine clinics of North America|date=August 2011|volume=29|issue=3|pages=539–52|pmid=21782073|doi=10.1016/j.emc.2011.04.001}}</ref>,在健康女性身上會持續平均六天<ref name=AFP2011/>,[[恥骨]]與[[下背部]]可能會出現些疼痛感。經歷過上泌尿道感染或是[[腎盂腎炎]]的人,可能會有[[側腹痛]],[[發燒]],或是反胃噁心的經驗,以及不同於典型下泌尿道感染的[[不適]]症狀。但比較少出現尿中帶[[血尿|血]]<ref name=Sal2011/>或尿中出現肉眼可見的[[膿]]的症狀<ref>{{cite book|last=Arellano|first=Ronald S.|title=Non-vascular interventional radiology of the abdomen|publisher=Springer|location=New York|isbn=978-1-4419-7731-1|page=67|url=https://books.google.com/books?id=au-OpXwnibMC&pg=PA67}}</ref>。 |
|||
===兒童=== |
|||
下泌尿道感染(lower urinary tract infections)和膀胱炎的主因通常是細菌通過尿道進入,但上泌尿道感染(upper urinary tract infections)如腎盂腎炎則不然。上泌尿道感染的主因可能是[[血原性]](hematogenous)的。 |
|||
對於年幼兒童來說,泌尿道感染的唯一可能症狀是發燒。也因為缺乏明顯的症狀,若兩歲以下女嬰或是未割包皮的一歲以下男嬰有發燒症狀時,醫療機構通常會建議進行尿液培養(culture of urine)。嬰兒泌尿道感染的症狀通常會有食慾降低、嘔吐、嗜睡、或[[黃疸]]等;年紀較大的兒童則會有[[尿失禁]]的現象<ref name=PeadsNA2011/>。 |
|||
===老年人=== |
|||
{{fact|[[過敏]]是泌尿道感染的一個隱性因素。舉例來說,對食物過敏可刺激[[膀胱|膀胱壁]],並增加感染此病的機會。 注意飲食並完成過敏測試,以避免可能導致過敏的食品。性交後患泌尿路感染可能是由於對[[乳膠]][[避孕套]]、[[殺精劑]](spermicide)或口服避孕藥過敏。在這種情況下,可以與醫生檢討控制生育的其他方法。 |
|||
尿道的症狀在老年人中並不常見<ref name=Elder2011/>,它呈現的方式不明顯,但會有尿失禁、 [[心理狀態的改變]]或是疲勞,是其少數可觀察到的症狀<ref name=EM2011/>。醫護人員可能會在一些患者檢測到[[敗血病]]-血液感染<ref name=Sal2011/>。因為很多老年人可能已有尿失禁或[[失智症]]等問題,因此常造成診斷上的複雜性<ref name=Elder2011/>。 |
|||
有時候,平時每天的飲水量不足,也是容易泌尿道感染原因之一。}} |
|||
若出現生理系統感染症狀,且無法回報尿道症狀的病患中(例如有進階[[失智症]]的情形),合理的作法是進行[[尿液培養]].<ref name=AMDA2015>{{Citation |author1 = AMDA – The Society for Post-Acute and Long-Term Care Medicine |author1-link = AMDA – The Society for Post-Acute and Long-Term Care Medicine |date = February 2014 |title = Ten Things Physicians and Patients Should Question |publisher = AMDA – The Society for Post-Acute and Long-Term Care Medicine |work = [[Choosing Wisely]]: an initiative of the [[ABIM Foundation]] |page = |url = http://www.choosingwisely.org/doctor-patient-lists/amda/ |accessdate = 20 April 2015}}</ref>。生理系統性的感染徵兆包括[[發燒]]、正常體溫上升多於1.1 °C (2.0 °F)、寒顫和[[血液中白血球的增加]]<ref name=AMDA2015/>。 |
|||
==診斷== |
|||
從患有排尿困難和頻尿的病人,在其排尿過程中抽取中間的那一段尿液作樣本送往檢驗,並特別留意[[亞硝酸鹽]]、白細胞或[[白細胞酯酶]]是否出現在樣本中。如果有一個較高的細菌負荷而沒有白細胞,則樣本很有可能已受到污染。診斷尿道炎是經尿液[[細菌培養]]證實的。 |
|||
==病因== |
|||
如果尿液細菌培養呈陰性反應: |
|||
[[大腸桿菌]]引起80%~85%的社區性泌尿道感染,而大約5%~10%是由於[[腐生葡萄球菌]]所造成的<ref name=Review08/>,還有極少數是因病毒或是真菌而感染的<ref>{{cite journal |last1=Amdekar |first1=S |author2=Singh, V, Singh, DD|title=Probiotic therapy: immunomodulating approach toward urinary tract infection.|journal=Current microbiology|date=November 2011|volume=63|issue=5|pages=484–90|pmid=21901556|doi=10.1007/s00284-011-0006-2}}</ref>。院內的泌尿道感染(大部分和[[導尿管]]有關)包含了非常廣泛的致病原:包括大腸桿菌(27%)、[[克雷白氏桿菌]](11%)、[[綠膿桿菌]](11%)、真菌病原體[[白色念珠菌]](9%)、腸球菌(7%)<ref name=Sal2011/><ref>{{cite journal |vauthors=Sievert DM, Ricks P, Edwards JR, etal |title=Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010 |journal=Infect Control Hosp Epidemiol |volume=34 |issue=1 |pages=1–14 | date=January 2013 |pmid=23221186 |doi=10.1086/668770 |url=}}</ref><ref>{{cite journal|last=Bagshaw|first=SM|author2=Laupland, KB |title=Epidemiology of intensive care unit-acquired urinary tract infections.|journal=Current opinion in infectious diseases|date=Feb 2006|volume=19|issue=1|pages=67–71|pmid=16374221|doi=10.1097/01.qco.0000200292.37909.e0}}</ref>。[[金黃色葡萄球菌]]而造成的泌尿道感染,其比率僅次於由血液傳播而造成的感染<ref name=EM2011/>。[[披衣菌]]和[[黴漿菌]]會感染尿道,但不會感染膀胱<ref>{{cite web |url=http://kidney.niddk.nih.gov/kudiseases/pubs/utiadult/ |title=Urinary Tract Infections in Adults |accessdate=January 1, 2015}}</ref>。這些感染通常被分類為[[尿道炎]]而非泌尿道感染。 |
|||
*尿道炎的症狀可能指向[[砂眼披衣菌]]或[[淋球菌]]感染。 |
|||
*膀胱炎的症狀可能指向[[間質性膀胱炎]]。 |
|||
*對於男性而言,排尿困難可能是由於[[前列腺炎]]。 |
|||
===性=== |
|||
在嚴重感染(如出現發燒、[[惡寒]]或腰痛)時,可測量[[尿素]]和[[肌酸酐]]以評估腎功能是否已受到影響。 |
|||
在性行為活躍的年輕女性中,75-90%膀胱感染是由性行為引起,且感染的風險與性愛頻率相關<ref name=Review08>{{cite journal|author=Nicolle LE|title=Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis|journal=Urol Clin North Am|volume=35|issue=1|pages=1–12, v|year=2008|pmid=18061019|doi=10.1016/j.ucl.2007.09.004}}</ref> 。蜜月膀胱炎(honeymoon cystitis)的術語已經用來描述在婚姻初期常患有上尿道感染疾病的現象。在[[停經]]後的婦女,性行為不會影響尿道感染的風險。在不考慮性交頻率的情況下,[[殺精劑]](Spermicide)的使用將會增加泌尿道感染的風險<ref name=Review08/>。而[[隔膜]](Diaphragm)的使用也會有相同的影響<ref name="recurrent uti">{{cite journal|last1=Franco|first1=AV|title=Recurrent urinary tract infections.|journal=Best practice & research. Clinical obstetrics & gynaecology|date=December 2005|volume=19|issue=6|pages=861–73|pmid=16298166|doi=10.1016/j.bpobgyn.2005.08.003}}</ref>。使用避孕套但不用殺精劑,或服用[[避孕藥]](birth control pills)不會提高無併發症的尿道感染風險<ref name=Review08/><ref>{{cite book |last1= Engleberg|first1= N C|authorlink1= |last2=DiRita |first2=V |last3=Dermody |first3=T S |title=Schaechter's Mechanism of Microbial Disease |year=2007 |publisher=Lippincott Williams & Wilkins |location= Baltimore|isbn=978-0-7817-5342-5}}</ref>。 |
|||
與男性相較,女性是屬於尿道感染疾病的較高風險群。其原因在於女性的尿道較短,且較接近肛門<ref name=NA2011>{{cite journal |last1=Dielubanza |first1=EJ |author2=Schaeffer, AJ|title=Urinary tract infections in women.|journal=The Medical clinics of North America|date=January 2011|volume=95|issue=1|pages=27–41|pmid=21095409|doi=10.1016/j.mcna.2010.08.023}}</ref>。此外,當女性的雌激素(estrogen)隨著[[停經]](menopause)而減少分泌時,尿道感染的機率也會提高,原因是缺少了[[陰道菌群]](vaginal flora)<ref name=NA2011/>的保護功能。另外,停經也會導致[[陰道萎縮]](vaginal atrophy),進而造成尿道感染疾病的復發<ref name="vaginal atrophy">{{cite journal|last1=Goldstein|first1=I|last2=Dicks|first2=B|last3=Kim|first3=NN|last4=Hartzell|first4=R|title=Multidisciplinary overview of vaginal atrophy and associated genitourinary symptoms in postmenopausal women.|journal=Sexual medicine|date=December 2013|volume=1|issue=2|pages=44–53|pmid=25356287|doi=10.1002/sm2.17}}</ref>。 |
|||
大多數情況下,女性的下尿路感染是良性的,並不需要詳盡的實驗跟進。不過,出生不久的嬰兒的尿道炎必須接受一些影像學檢查,通常是[[逆行尿道造影]],以確定是否出現先天性泌尿道異常(如膀胱輸尿管逆流、尿道瓣膜或尿路阻塞)。男性也必須作進一步的檢查。具體的檢查方法包括[[X光]]、[[核磁共振成像]]和[[X射線斷層成像]]掃描技術。 |
|||
。[[慢性前列腺炎]](chronic prostitis)也會導致男性尿道感染疾病的復發<ref name=Lipsky1999>{{cite journal|last1=Lipsky|first1=BA|title=Prostatitis and urinary tract infection in men: what's new; what's true?|journal=The American journal of medicine|date=March 1999|volume=106|issue=3|pages=327–34|pmid=10190383|doi=10.1016/s0002-9343(99)00017-0}}</ref>。其感染風險也會隨著男性的年齡增長提高<ref name=Lipsky1999/>。而較高齡男性的尿液中普遍上都有細菌的存在,故此點不列入影響尿道感染風險的討論<ref name=Lipsky1999/>。 |
|||
==治療== |
|||
最簡單的泌尿道感染可以透過服用[[抗生素]]如[[甲氧芐啶]](|Trimethoprim)、[[頭孢菌素]]、[[呋喃妥因]]或[[氟化奎林酮類]](fluoroquinolone,如[[環丙沙星]](Ciprofloxacin)、[[左氧氟沙星]](Levofloxacin))治療。通常年輕的成年人連續服用3天,老人則5天。雖然[[Co-trimoxazole]]以前曾在國際間被使用(在美國則繼續被使用),但相比於成分中的甲氧芐啶,額外的[[磺胺]](sulphonamide)只帶來一丁點額外的好處,卻是導致高發病率的輕度[[過敏]]反應和導致一些罕見但嚴重的[[併發症]]的主要原因。 |
|||
===導尿=== |
|||
如果病人的[[症狀]]與腎盂腎炎一致,這可能顯示需要[[靜脈注射]]抗生素治療。療法因人而異,通常是[[氨基糖苷類抗生素|氨基糖苷類]],如[[慶大霉素]](Gentamicin)和[[β內醯胺類抗生素]](Beta-lactam antibiotic)如[[氨芐青黴素]]或[[頭孢曲松]]等結合使用,直至發熱消退後的48小時。其後病人可以出院回家口服抗生素5天。 |
|||
[[導尿]]会增加尿道感染的風險。[[菌尿症]](尿裡面有細菌)的風險是每天介乎3-6%, 而預防性的抗生素對正在減少的徵狀性感染是沒有效果的<ref name=NA2011/>。降低感染風險的方式有:只在有需要的情況下進行導尿、使用[[無菌操作]]插入方式、和保持封閉的、沒有堵塞的導尿管排尿<ref name="Nic2001"/><ref>{{cite journal|author1=Phipps, S.|author2= Lim, Y.N.|author3=McClinton, S.|author4=Barry, C.|author5=Rane, A.|author6=N'Dow, J.|journal=Cochrane Database of Systematic Reviews|volume=|issue=2|pages=CD004374|year=2006|pmid=16625600|doi=10.1002/14651858.CD004374.pub2|editor1-last=Phipps|editor1-first=Simon|title=Short term urinary catheter policies following urogenital surgery in adults}}</ref><ref name="Gould2009"/>。 |
|||
男性[[潛水員]]使用[[陰莖套導管]],女性潛水員在[[乾式潛水衣]]使用外在捕捉器具(external catching device)也比較容易有泌尿道感染的問題<ref name="pmid22752741">{{cite journal |author=Harris, Richard |title=Genitourinary infection and barotrauma as complications of 'P-valve' use in drysuit divers |journal=Diving and Hyperbaric Medicine : the Journal of the [[South Pacific Underwater Medicine Society]] |volume=39 |issue=4 |pages=210–2|date=December 2009 |pmid=22752741 |url=http://archive.rubicon-foundation.org/9482 |accessdate=2013-04-04}}</ref>。 |
|||
如果病人對 IV antibiotics 反應冷淡(例如持續高燒,腎功能惡化),那麼表明需要掃描成像,以排除在腎內或周圍形成[[膿瘡]],或是存在著一些堵塞組織(如[[結石]]或[[腫瘤]])的可能性。最好的成像方法是[[X射线断层成像|CT掃描]]。 |
|||
===其他=== |
|||
{{fact|作為[[在家治療]],多喝水、頻繁排尿、避免食[[糖]]和含糖食品、飲用未加糖的[[蔓越莓汁]]、服用[[蔓越莓]]濃縮膠囊,以及在每天最後一餐時服用[[維生素C]],可縮短感染的時間。糖分和酒精可以養活引起感染的細菌,並且惡化疼痛和其他症狀。維生素C在夜間會令尿液變酸,阻止細菌在泌尿道生長。}} |
|||
基因遺傳可能引起泌尿道感染.其他可能造成風險的因素有[[糖尿病]]<ref name=Review08/>,男性未接受[[割禮]],及[[攝護腺肥大]]<ref name=EM2011/>。其他複雜的因素相當的模糊,包括誘發結構性,功能性,或是代謝上的異常<ref name=bryan>[http://pathmicro.med.sc.edu/infectious%20disease/Urinary%20Tract%20Infections.htm Infectious Disease, Chapter Seven, Urinary Tract Infections] from ''Infectious Disease Section of Microbiology and Immunology On-line''. By Charles Bryan MD. University of South Carolina. This page last changed on Wednesday, April 27, 2011</ref>。對於兒童,泌尿道感染與[[膀胱輸尿管返流]]([[尿液]])從膀胱到輸尿管或腎臟的異常流動)及[[便秘]]有關連<ref name=PeadsNA2011/>。 |
|||
患有[[脊椎損傷]]的人因為長期使用導尿管及[[排尿]]的功能異常,有更高泌尿道感染的風險<ref name=Spine2010>{{cite journal |last1=Eves |first1=FJ |author2=Rivera, N|title=Prevention of urinary tract infections in persons with spinal cord injury in home health care.|journal=Home healthcare nurse|date=April 2010|volume=28|issue=4|pages=230–41|pmid=20520263|doi=10.1097/NHH.0b013e3181dc1bcb}}</ref>.這是此群體受到感染的主要原因之一,也是他們住院的主要緣由<ref name=Spine2010/>。而且蔓越莓汁與蔓越莓補給品對這些人群的預防與治療沒有呈現效果<ref>{{cite journal|last=Opperman|first=EA|title=Cranberry is not effective for the prevention or treatment of urinary tract infections in individuals with spinal cord injury.|journal=Spinal cord|date=June 2010|volume=48|issue=6|pages=451–6|pmid=19935757|doi=10.1038/sc.2009.159}}</ref>。 |
|||
如有以下情況建議諮詢醫生意見: |
|||
{{Hidden begin |title=未翻譯內容}} |
|||
*疼痛是在背部(back region,這可能是腎臟感染) |
|||
==Pathogenesis== |
|||
*疼痛持續 |
|||
[[File:Bladder Infection.png|thumb|Bladder infection.<ref>{{cite web|title=Bladder infection|url=http://blausen.com/?Topic=1628|website=Blausen Medical|accessdate=4 November 2015}}</ref>]] |
|||
*發燒 |
|||
The [[bacteria]] that cause urinary tract infections typically enter the bladder via the urethra. However, infection may also occur via the blood or [[lymph]].<!-- <ref name=Sal2011/> --> It is believed that the bacteria are usually transmitted to the urethra from the bowel, with females at greater risk due to their anatomy.<!-- <ref name=Sal2011/> --> After gaining entry to the bladder, ''E. Coli'' are able to attach to the bladder wall and form a [[biofilm]] that resists the body's immune response.<ref name=Sal2011/> |
|||
*尿液帶血 |
|||
==Diagnosis== |
|||
[[Image:Bacteriuria pyuria 4.jpg|thumb|left|Multiple [[bacilli]] (rod-shaped bacteria, here shown as black and bean-shaped) shown between white blood cells in urinary microscopy. These changes are indicative of a urinary tract infection.]] |
|||
In straightforward cases, a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation.<!-- <ref name=Review08/> --> In complicated or questionable cases, it may be useful to confirm the diagnosis via [[urinalysis]], looking for the presence of [[urinary nitrite]]s, [[white blood cells]] (leukocytes), or [[leukocyte esterase]].<ref name="Detweiler2015">{{cite journal|author=Detweiler K, Mayers D, Fletcher SG|title=Bacteruria and Urinary Tract Infections in the Elderly|journal=The Urologic Clinics of North America|volume=42|issue=4|pages=561–8|date=November 2015|pmid=26475952|doi=10.1016/j.ucl.2015.07.002|type=Review}}</ref> Another test, [[urine microscopy]], looks for the presence of [[red blood cells]], white blood cells, or bacteria.<!-- <ref name=Review08/> --> Urine [[microbiological culture|culture]] is deemed positive if it shows a bacterial colony count of greater than or equal to 10<sup>3</sup> [[colony-forming unit]]s per mL of a typical urinary tract organism.<!-- <ref name=Review08/> --> Antibiotic sensitivity can also be tested with these cultures, making them useful in the selection of antibiotic treatment.<!-- <ref name=Review08/> --> However, women with negative cultures may still improve with antibiotic treatment.<ref name=Review08/> As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.<ref name=Elder2011/> |
|||
===Classification=== |
|||
A urinary tract infection may involve only the lower urinary tract, in which case it is known as a bladder infection. Alternatively, it may involve the upper urinary tract, in which case it is known as pyelonephritis.<!-- <ref name=EM2011/> --> If the urine contains significant bacteria but there are no symptoms, the condition is known as [[asymptomatic bacteriuria]].<ref name=EM2011/> If a urinary tract infection involves the upper tract, and the person has [[diabetes mellitus]], is pregnant, is male, or [[immunocompromised]], it is considered complicated.<ref name=AFP2011/><ref name=Sal2011/> Otherwise if a woman is healthy and [[premenopausal]] it is considered uncomplicated.<ref name=AFP2011/> In children when a urinary tract infection is associated with a fever, it is deemed to be an upper urinary tract infection.<ref name=PeadsNA2011>{{cite journal |last1=Bhat |first1=RG |author2=Katy, TA, Place, FC|title=Pediatric urinary tract infections.|journal=Emergency medicine clinics of North America|date=August 2011|volume=29|issue=3|pages=637–53|pmid=21782079|doi=10.1016/j.emc.2011.04.004}}</ref> |
|||
===Children=== |
|||
To make the diagnosis of a urinary tract infection in children, a positive urinary culture is required.<!-- <ref name=PeadsNA2011/> --> Contamination poses a frequent challenge depending on the method of collection used, thus a cutoff of 10<sup>5</sup> CFU/mL is used for a "clean-catch" mid stream sample, 10<sup>4</sup> CFU/mL is used for catheter-obtained specimens, and 10<sup>2</sup> CFU/mL is used for [[suprapubic aspiration]]s (a sample drawn directly from the bladder with a needle).<!-- <ref name=PeadsNA2011/> --> The use of "urine bags" to collect samples is discouraged by the [[World Health Organization]] due to the high rate of contamination when cultured, and catheterization is preferred in those not toilet trained.<!-- <ref name=PeadsNA2011/> --> Some, such as the [[American Academy of Pediatrics]] recommends [[renal ultrasound]] and [[voiding cystourethrogram]] (watching a person's urethra and urinary bladder with real time x-rays while they urinate) in all children less than two years old who have had a urinary tract infection.<!-- <ref name=PeadsNA2011/> --> However, because there is a lack of effective treatment if problems are found, others such as the [[National Institute for Health and Care Excellence]] only recommends routine imaging in those less than six months old or who have unusual findings.<ref name=PeadsNA2011/> |
|||
===Differential diagnosis=== |
|||
In women with [[cervicitis]] (inflammation of the [[cervix]]) or [[vaginitis]] (inflammation of the [[vagina]]) and in young men with UTI symptoms, a ''[[Chlamydia trachomatis]]'' or ''[[Neisseria gonorrheae]]'' infection may be the cause.<ref name=EM2011/><ref>{{cite journal |last1=Raynor |first1=MC |author2=Carson CC, 3rd|title=Urinary infections in men.|journal=The Medical clinics of North America|date=January 2011|volume=95|issue=1|pages=43–54|pmid=21095410|doi=10.1016/j.mcna.2010.08.015}}</ref> These infections are typically classified as a [[urethritis]] rather than a urinary tract infection. Vaginitis may also be due to a [[candidal vulvovaginitis|yeast infection]].<ref name=Book2011>{{cite book |last1=Leung |first1=David Hui; edited by Alexander |title=Approach to internal medicine : a resource book for clinical practice|publisher=Springer|location=New York|isbn=978-1-4419-6504-2|page=244|url=https://books.google.com/books?id=lnXNpj5ZzKMC&pg=PA244|edition=3rd|author2=Padwal, Raj}}</ref> [[Interstitial cystitis]] (chronic pain in the bladder) may be considered for people who experience multiple episodes of UTI symptoms but urine cultures remain negative and not improved with antibiotics.<ref>{{cite book |last1=Kursh |first1=edited by Elroy D. |title=Office urology|year=2000|publisher=Humana Press|location=Totowa, N.J.|isbn=978-0-89603-789-2|page=131|url=https://books.google.com/books?id=AdYs-QwU8KQC&pg=PA131|author2=Ulchaker, James C.}}</ref> [[Prostatitis]] (inflammation of the [[prostate]]) may also be considered in the differential diagnosis.<ref>{{cite book|last=Walls|first=authors, Nathan W. Mick, Jessica Radin Peters, Daniel Egan; editor, Eric S. Nadel; advisor, Ron|title=Blueprints emergency medicine|year=2006|publisher=Lippincott Williams & Wilkins|location=Baltimore, Md.|isbn=978-1-4051-0461-6|page=152|url=https://books.google.com/books?id=NvqaWHi1OTsC&pg=RA1-PA152|edition=2nd}}</ref> |
|||
[[Hemorrhagic cystitis]], characterized by [[hematuria|blood in the urine]], can occur secondary to a number of causes including: infections, [[radiation therapy]], underlying cancer, medications and toxins.<ref name=Keanse2009/> Medications that commonly cause this problem include the [[chemotherapeutic agent]] [[cyclophosphamide]] with rates of 2 to 40%.<ref name=Keanse2009>{{cite book|last=Keane|first=edited by Sam D. Graham, Thomas E.|title=Glenn's urologic surgery|year=2009|publisher=Lippincott Williams & Wilkins|location=Philadelphia, Pa.|isbn=9780781791410|page=148|url=https://books.google.com/books?id=GahMzaKgMKAC&pg=PA148|edition=7th}}</ref> [[Eosinophilic cystitis]] is a rare condition where [[eosinophiles]] are present in the bladder wall.<ref name=Kramer2002/> Signs and symptoms are similar to a bladder infection.<ref name=Kramer2002>{{cite book|last=Kramer|first=ed. by A. Barry Belman; Lowell R. King; Stephen A.|title=Clinical pediatric urology|year=2002|publisher=Dunitz|location=London|isbn=9781901865639|page=338|url=https://books.google.com/books?id=IKexq6xCRmIC&pg=PA338|edition=4.}}</ref> Its cause is not entirely clear; however, it may be linked to [[food allergies]], [[infections]], and medications among others.<ref>{{cite journal |last1=Popescu |first1=OE |author2=Landas, SK; Haas, GP|title=The spectrum of eosinophilic cystitis in males: case series and literature review.|journal=Archives of pathology & laboratory medicine|date=February 2009|volume=133|issue=2|pages=289–94|pmid=19195972|doi=10.1043/1543-2165-133.2.289}}</ref> |
|||
==Prevention== |
|||
A number of measures have not been confirmed to affect UTI frequency including: urinating immediately after intercourse, the type of underwear used, personal hygiene methods used after urinating or [[defecating]], or whether a person typically bathes or showers.<ref name=Review08/> There is similarly a lack of evidence surrounding the effect of holding one's urine, [[tampon]] use, and douching.<ref name=NA2011/> In those with frequent urinary tract infections who use [[spermicide]] or a [[diaphragm (contraceptive)|diaphragm]] as a method of contraception, they are advised to use alternative methods.<ref name=Sal2011/> In those with [[benign prostatic hyperplasia]] urinating in a sitting position appears to improve bladder emptying which might decrease urinary tract infections in this group.<ref>{{cite journal|last1=de Jong|first1=Y|last2=Pinckaers|first2=JH|last3=Ten Brinck|first3=RM|last4=Lycklama À Nijeholt|first4=AA|last5=Dekkers|first5=OM|title=Urinating Standing versus Sitting: Position Is of Influence in Men with Prostate Enlargement. A Systematic Review and Meta-Analysis.|journal=PLoS ONE|date=2014|volume=9|issue=7|pages=e101320|DOI=10.1371/journal.pone.0101320|pmid=25051345|pmc=4106761}}</ref> |
|||
Using urinary catheters as little and as short of time as possible and appropriate care of the catheter when used prevents infections.<ref name=Nic2001>{{cite journal|author=Nicolle LE|title=The chronic indwelling catheter and urinary infection in long-term-care facility residents|journal=Infect Control Hosp Epidemiol|volume=22|issue=5|pages=316–21|year=2001|pmid=11428445|doi=10.1086/501908}}</ref> |
|||
They should be inserted using sterile technique in hospital however non-sterile technique may be appropriate in those who self catheterize.<ref name=Gould2009>{{cite journal|author=Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA|title=Guideline for prevention of catheter-associated urinary tract infections 2009|journal=Infect Control Hosp Epidemiol|volume=31|issue=4|pages=319–26|year=2010|pmid=20156062|doi=10.1086/651091}}</ref> The urinary catheter set up should also be kept sealed.<ref name=Gould2009/> Evidence does not support a significant decrease in risk when silver-alloy catheters are used.<ref name=Lam2014>{{cite journal|last1=Lam|first1=TB|last2=Omar|first2=MI|last3=Fisher|first3=E|last4=Gillies|first4=K|last5=MacLennan|first5=S|title=Types of indwelling urethral catheters for short-term catheterisation in hospitalised adults.|journal=The Cochrane database of systematic reviews|date=Sep 23, 2014|volume=9|pages=CD004013|pmid=25248140|doi=10.1002/14651858.CD004013.pub4}}</ref> |
|||
===Medications=== |
|||
For those with recurrent infections, taking a short course of antibiotics when each infection occurs is associated with the lowest antibiotic use.<ref name=P2013>{{cite journal|title=Recurrent uncomplicated cystitis in women: allowing patients to self-initiate antibiotic therapy.|journal=Rev Prescire|date=Nov 2013|volume=22|issue=361|pages=835–837|pmid=24669389}}</ref> A prolonged course of daily antibiotics is also effective.<ref name=Review08/> Medications frequently used include [[nitrofurantoin]] and [[trimethoprim/sulfamethoxazole]] (TMP/SMX).<ref name=Sal2011/> [[Methenamine]] is another agent used for this purpose as in the bladder where the acidity is low it produces [[formaldehyde]] to which resistance does not develop.<ref>{{cite book|last=Cubeddu|first=Richard Finkel, Michelle A. Clark, Luigi X.|title=Pharmacology|year=2009|publisher=Lippincott Williams & Wilkins|location=Philadelphia|isbn=9780781771559|pages=397|url=https://books.google.com/books?id=Q4hG2gRhy7oC&pg=PA397&lpg=PA397|edition=4th}}</ref> Some recommend against prolonged use due to concerns of [[antibiotic resistance]].<ref name=P2013/> |
|||
In cases where infections are related to intercourse, taking antibiotics afterwards may be useful.<ref name=Sal2011/> In post-menopausal women, [[topical]] vaginal [[estrogen]] has been found to reduce recurrence.<!-- <ref name=Cochrane2008/> --> As opposed to topical creams, the use of vaginal estrogen from [[Pessary|pessaries]] has not been as useful as low dose antibiotics.<ref name=Cochrane2008>{{cite journal |last1=Perrotta |first1=C |author2=Aznar, M, Mejia, R, Albert, X, Ng, CW|title=Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. |journal=Cochrane database of systematic reviews (Online) |date=2008-04-16 |issue=2 |pages=CD005131 |pmid=18425910 |doi=10.1002/14651858.CD005131.pub2}}</ref> Antibiotics following short term urinary catheterization decreases the subsequent risk of a bladder infection.<ref>{{cite journal |author=Marschall J, Carpenter CR, Fowler S, Trautner BW |title=Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analysis |journal=BMJ |volume=346 |issue= |pages=f3147 |year=2013 |pmid=23757735 |pmc=3678514 |doi= 10.1136/bmj.f3147|url=}}</ref> A number of [[vaccine]]s are in development as of 2011.<ref name=Sal2011/> |
|||
===Children=== |
|||
The evidence that [[prophylactic|preventative]] antibiotics decrease urinary tract infections in children is poor.<ref name=Child2010>{{cite journal|last1=Dai|first1=B|last2=Liu|first2=Y|last3=Jia|first3=J|last4=Mei|first4=C|title=Long-term antibiotics for the prevention of recurrent urinary tract infection in children: a systematic review and meta-analysis|journal=Archives of Disease in Childhood|volume=95|issue=7|pages=499–508|year=2010|pmid=20457696|doi=10.1136/adc.2009.173112}}</ref> However recurrent UTIs are a rare cause of further kidney problems if there are no underlying abnormalities of the kidneys, resulting in less than a third of a percent (0.33%) of [[chronic kidney disease]] in adults.<ref>{{cite journal |last1=Salo |first1=J |author2=Ikäheimo, R, Tapiainen, T, Uhari, M|title=Childhood urinary tract infections as a cause of chronic kidney disease.|journal=Pediatrics|date=November 2011|volume=128|issue=5|pages=840–7|pmid=21987701|doi=10.1542/peds.2010-3520}}</ref> Whether routine circumcisions prevents UTIs has not been well studied as of 2011.<ref>{{cite journal |last1=Jagannath |first1=VA |author2=Fedorowicz, Z; Sud, V; Verma, AK; Hajebrahimi, S|title=Routine neonatal circumcision for the prevention of urinary tract infections in infancy.|journal=Cochrane database of systematic reviews (Online) |date=November 14, 2012 |volume=11 |pages=CD009129 |pmid=23152269 |doi=10.1002/14651858.CD009129.pub2}}</ref> |
|||
===Alternative medicine=== |
|||
Some research suggests that [[cranberry]] (juice or capsules) may decrease the number of UTIs in those with frequent infections.<ref name=Wang2012>{{cite journal |vauthors=Wang CH, Fang CC, Chen NC, etal |title=Cranberry-containing products for prevention of urinary tract infections in susceptible populations | journal=Arch Intern Med | year=2012 | volume=172 |issue=13 | pages=988–96 | doi=10.1001/archinternmed.2012.3004 | pmid=22777630}}</ref><ref>{{cite journal |last1=Wang |first1=CH |author2=Fang, CC; Chen, NC; Liu, SS; Yu, PH; Wu, TY; Chen, WT; Lee, CC; Chen, SC|title=Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials.|journal=Archives of Internal Medicine|date=July 9, 2012 |volume=172|issue=13|pages=988–96|pmid=22777630|doi=10.1001/archinternmed.2012.3004}}</ref> A [[Cochrane review]] concluded that the benefit, if it exists, is small.<ref name=Jepsen2012>{{cite journal |last1=Jepson |first1=RG |author2=Williams, G; Craig, JC|title=Cranberries for preventing urinary tract infections.|journal=Cochrane database of systematic reviews (Online)|date=October 17, 2012 |volume=10|pages=CD001321|pmid=23076891|doi=10.1002/14651858.CD001321.pub5}}</ref> Long-term tolerance is also an issue<ref name="Jepsen2012" /> with gastrointestinal upset occurring in more than 30%.<ref>{{cite journal |last1=Rossi |first1=R |author2=Porta, S, Canovi, B|title=Overview on cranberry and urinary tract infections in females.|journal=Journal of Clinical Gastroenterology|date=September 2010|volume=44 Suppl 1|pages=S61-2|pmid=20495471|doi=10.1097/MCG.0b013e3181d2dc8e}}</ref> Cranberry juice is thus not currently recommended for this indication.<ref name=Jepsen2012/> As of 2011, intravaginal [[probiotics]] require further study to determine if they are beneficial.<ref name=Sal2011/> |
|||
==Treatment== |
|||
The mainstay of treatment is [[antibiotic]]s. [[Phenazopyridine]] is occasionally prescribed during the first few days in addition to antibiotics to help with the burning and urgency sometimes felt during a bladder infection.<ref>{{cite journal|last=Gaines|first=KK|title=Phenazopyridine hydrochloride: the use and abuse of an old standby for UTI.|journal=Urologic nursing|date=June 2004|volume=24|issue=3|pages=207–9|pmid=15311491}}</ref> However, it is not routinely recommended due to safety concerns with its use, specifically an elevated risk of [[methemoglobinemia]] (higher than normal level of [[methemoglobin]] in the blood).<ref>{{cite book|last=Aronson|first=edited by Jeffrey K.|title=Meyler's side effects of analgesics and anti-inflammatory drugs|year=2008|publisher=Elsevier Science|location=Amsterdam|isbn=978-0-444-53273-2|page=219|url=https://books.google.com/books?id=2WxotnWiiWkC&pg=PA219}}</ref> [[Acetaminophen]] (paracetamol) may be used for fevers.<ref>{{cite book|last=Glass|first=[edited by] Jill C. Cash, Cheryl A.|title=Family practice guidelines|year=2010|publisher=Springer|location=New York|isbn=978-0-8261-1812-7|page=271|url=https://books.google.com/books?id=4uKsZZ4BoRUC&pg=PA271|edition=2nd}}</ref> There is no good evidence for the use of cranberry products for treating current infections.<ref>{{cite journal|last=Santillo|first=VM|author2=Lowe, FC |title=Cranberry juice for the prevention and treatment of urinary tract infections.|journal=Drugs of today (Barcelona, Spain : 1998)|date=Jan 2007|volume=43|issue=1|pages=47–54|pmid=17315052|doi=10.1358/dot.2007.43.1.1032055}}</ref><ref>{{cite journal|last=Guay|first=DR|title=Cranberry and urinary tract infections.|journal=Drugs|year=2009|volume=69|issue=7|pages=775–807|pmid=19441868|doi=10.2165/00003495-200969070-00002}}</ref> |
|||
===Asymptomatic bacteriuria=== |
|||
Those who have bacteria in the urine but no symptoms should not generally be treated with antibiotics.<ref name="Ariathianto">{{cite journal|last=Ariathianto|first=Y|title=Asymptomatic bacteriuria - prevalence in the elderly population.|journal=Australian family physician|date=Oct 2011|volume=40|issue=10|pages=805–9|pmid=22003486}}</ref> This includes those who are old, those with spinal cord injuries, and those who have urinary catheters.<ref name="Colgan">{{cite journal|last=Colgan|first=R|author2=Nicolle, LE |author3=McGlone, A |author4= Hooton, TM |title=Asymptomatic bacteriuria in adults.|journal=American family physician|date=Sep 15, 2006|volume=74|issue=6|pages=985–90|pmid=17002033}}</ref><ref name="AGSfive">{{Citation |author1 = American Geriatrics Society |author1-link = American Geriatrics Society |title = Five Things Physicians and Patients Should Question |publisher = American Geriatrics Society |work = [[Choosing Wisely]]: an initiative of the [[ABIM Foundation]] |page = |url = http://www.choosingwisely.org/doctor-patient-lists/american-geriatrics-society/ |accessdate = August 1, 2013}}</ref> Pregnancy is an exception and it is recommended that women take 7 days of antibiotics.<ref name="Widmer-2011">{{Cite journal | last1 = Widmer | first1 = M. | last2 = Gülmezoglu | first2 = AM. | last3 = Mignini | first3 = L. | last4 = Roganti | first4 = A. | title = Duration of treatment for asymptomatic bacteriuria during pregnancy. | journal = Cochrane Database Syst Rev | volume = | issue = 12 | pages = CD000491 | year = 2011 | doi = 10.1002/14651858.CD000491.pub2 | PMID = 22161364 }}</ref><ref name="Guinto-2010">{{Cite journal | last1 = Guinto | first1 = VT. | last2 = De Guia | first2 = B. | last3 = Festin | first3 = MR. | last4 = Dowswell | first4 = T. | title = Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy. | journal = Cochrane Database Syst Rev | volume = | issue = 9 | pages = CD007855 | year = 2010 | doi = 10.1002/14651858.CD007855.pub2 | PMID = 20824868 }}</ref> If not treated it causes up to 30% of mothers to develop [[pyelonephritis]] and increases risk of [[low birth weight]] and [[preterm birth]].<ref name="Smaill-2007"/> Some also support treatment of those with [[diabetes mellitus]]<ref>{{cite journal|last=Julka|first=S|title=Genitourinary infection in diabetes.|journal=Indian journal of endocrinology and metabolism|date=Oct 2013|volume=17|issue=Suppl1|pages=S83-S87|pmid=24251228|doi=10.4103/2230-8210.119512|pmc=3830375}}</ref> and treatment before urinary tract procedures which will likely cause bleeding.<ref name="AGSfive"/> |
|||
===Uncomplicated=== |
|||
Uncomplicated infections can be diagnosed and treated based on symptoms alone.<ref name=Review08/> Oral antibiotics such as [[trimethoprim/sulfamethoxazole]] (TMP/SMX), [[nitrofurantoin]], or [[fosfomycin]] are typically first line.<ref>{{cite journal|last1=Grigoryan|first1=L|last2=Trautner|first2=BW|last3=Gupta|first3=K|title=Diagnosis and management of urinary tract infections in the outpatient setting: a review.|journal=JAMA|date=October 22, 2014 |volume=312|issue=16|pages=1677–84|pmid=25335150|doi=10.1001/jama.2014.12842}}</ref> [[Cephalosporin]]s, [[amoxicillin/clavulanic acid]], or a [[quinolone|fluoroquinolone]] may also be used.<ref name=Cochrane10/> However, [[antibiotic resistance|resistance]] to fluoroquinolones among the bacterial that cause urinary infections has been increasing.<ref name="Detweiler2015"/> These medications substantially shorten the time to recovery with all being equally effective.<ref name=Cochrane10>{{cite journal|author1=Zalmanovici Trestioreanu, A.|author2= Green, H.|author3= Paul, M.|author4= Yaphe, J.|author5= Leibovici, L.|journal=Cochrane Database of Systematic Reviews|volume=10|issue= 10|pages=CD007182|year=2010|pmid=20927755|doi=10.1002/14651858.CD007182.pub2|editor1-last=Zalmanovici Trestioreanu|editor1-first=Anca|title=Antimicrobial agents for treating uncomplicated urinary tract infection in women}}</ref><ref>{{cite journal|last=Jarvis|first=TR|author2=Chan, L |author3=Gottlieb, T |title=Assessment and management of lower urinary tract infection in adults|journal=Australian Prescriber|date=February 2014|volume=37|issue=1|pages=7–9|url=http://www.australianprescriber.com/magazine/37/1/article/1477.pdf}}</ref> A three-day treatment with trimethoprim, TMP/SMX, or a fluoroquinolone is usually sufficient, whereas nitrofurantoin requires 5–7 days.<ref name=Review08/><ref name=IDSA2010/> Fosfomycin may be used as a single dose but has been associated with lower rates of efficacy.<ref name="Detweiler2015"/> |
|||
With treatment, symptoms should improve within 36 hours.<ref name=AFP2011/> About 50% of people will recover without treatment within a few days or weeks.<ref name=Review08/> Fluoroquinolones are not recommended as a first treatment.<ref name="Detweiler2015"/><ref name="AUSFive">{{Citation |author1 = American Urogynecologic Society|author1-link = American Urogynecologic Society |date = May 5, 2015 |title = Five Things Physicians and Patients Should Question |publisher = American Urogynecologic Society |work = [[Choosing Wisely]]: an initiative of the [[ABIM Foundation]] |page = |url = http://www.choosingwisely.org/societies/american-urogynecologic-society/ |accessdate = June 1, 2015}}</ref> The Infectious Diseases Society of America states this due to the concern of generating [[antibiotic resistance|resistance]] to this class of medication.<ref name=IDSA2010>{{cite journal |last1=Gupta |first1=K |author2=Hooton, TM, Naber, KG, Wullt, B, Colgan, R, Miller, LG, Moran, GJ, Nicolle, LE, Raz, R, Schaeffer, AJ, Soper, DE, Infectious Diseases Society of America, European Society for Microbiology and Infectious, Diseases|title=International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases.|journal=Clinical infectious diseases : an official publication of the Infectious Diseases Society of America|date=2011-03-01|volume=52|issue=5|pages=e103-20|pmid=21292654|doi=10.1093/cid/ciq257}}</ref> [[Amoxicillin-clavulanate]] appears less effective than other options.<ref>{{cite journal |last1=Knottnerus |first1=BJ |author2=Grigoryan, L; Geerlings, SE; Moll van Charante, EP; Verheij, TJ; Kessels, AG; ter Riet, G|title=Comparative effectiveness of antibiotics for uncomplicated urinary tract infections: network meta-analysis of randomized trials.|journal=Family practice|date=December 2012|volume=29|issue=6|pages=659–70|pmid=22516128|doi=10.1093/fampra/cms029}}</ref> Despite this precaution, some resistance has developed to all of these medications related to their widespread use.<ref name=Review08/> [[Trimethoprim]] alone is deemed to be equivalent to TMP/SMX in some countries.<ref name=IDSA2010/> For simple UTIs, children often respond to a three-day course of antibiotics.<ref>{{cite web|url=http://www.bestbets.org/bets/bet.php?id=939|author=Shadi Afzalnia|date=December 15, 2006|title=BestBets: Is a short course of antibiotics better than a long course in the treatment of UTI in children|website=www.bestbets.org}}</ref> Women with recurrent simple UTIs may benefit from self-treatment upon occurrence of symptoms with medical follow-up only if the initial treatment fails.<ref name=Review08/> |
|||
===Complicated=== |
|||
Complicated UTIs are more difficult to treat and usually requires more aggressive evaluation, treatment and follow-up.<ref name=Bryan2002>{{cite book |author=Bryan, Charles S. |title=Infectious diseases in primary care |publisher=W.B. Saunders |location=Philadelphia |year=2002 |pages=319 |isbn=0-7216-9056-4 |oclc= |doi= |url=http://pathmicro.med.sc.edu/infectious%20disease/Urinary%20Tract%20Infections.htm}}</ref> It may require identifying and addressing the underlying complication.<ref>{{Cite journal | last1 = Wagenlehner |first1 = FM. | last2 = Vahlensieck | first2 = W. | last3 = Bauer | first3 = HW. | last4 = Weidner | first4 = W. | last5 = Piechota | first5 = HJ. | last6 = Naber | first6 = KG. | title = Prevention of recurrent urinary tract infections. | journal = Minerva Urol Nefrol | volume = 65 | issue = 1 | pages = 9–20 |date=Mar 2013 | doi = | PMID = 23538307 }}</ref> Increasing [[antibiotic resistance]] is causing concern about the future of treating those with complicated and recurrent UTI.<ref name="Pallett-2010">{{Cite journal | last1 = Pallett | first1 = A. | last2 = Hand | first2 = K. | title = Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria. | journal = J Antimicrob Chemother | volume = 65 Suppl 3 | issue = | pages = iii25-33 |date=Nov 2010 | doi = 10.1093/jac/dkq298 | PMID = 20876625 }}</ref><ref name="Shepherd-2013">{{Cite journal | last1 = Shepherd | first1 = AK. | last2 = Pottinger | first2 = PS. | title = Management of urinary tract infections in the era of increasing antimicrobial resistance. | journal = Med Clin North Am | volume = 97 | issue = 4 | pages = 737–57, xii |date=Jul 2013 | doi = 10.1016/j.mcna.2013.03.006 | PMID = 23809723 }}</ref> |
|||
===Pyelonephritis=== |
|||
[[Pyelonephritis]] is treated more aggressively than a simple bladder infection using either a longer course of oral antibiotics or [[intravenous]] antibiotics.<ref name=Pylo2011>{{cite journal |last1=Colgan |first1=R |author2=Williams, M, Johnson, JR|title=Diagnosis and treatment of acute pyelonephritis in women.|journal=American family physician|date=2011-09-01|volume=84|issue=5|pages=519–26|pmid=21888302}}</ref> Seven days of the oral fluoroquinolone [[ciprofloxacin]] is typically used in areas where the resistance rate is less than 10%.<!-- <ref name=Pylo2011/> --> If the local resistance rates are greater than 10%, a dose of intravenous [[ceftriaxone]] is often prescribed.<ref name=Pylo2011/> Trimethoprim/sulfamethoxazole or [[amoxicillin/clavulanate]] orally for 14 days is another reasonable option.<ref>{{cite book |title=The Sanford Guide to Antimicrobial Therapy 2011 (Guide to Antimicrobial Therapy (Sanford)) |publisher=Antimicrobial Therapy |location= |year=2011 |pages=30 |isbn=1-930808-65-8 |oclc= |doi= |accessdate=}}</ref> In those who exhibit more severe symptoms, admission to a hospital for ongoing antibiotics may be needed.<ref name=Pylo2011/> Complications such as [[urinary obstruction]] from a [[kidney stone]] may be considered if symptoms do not improve following two or three days of treatment.<ref name=EM2011/><ref name=Pylo2011/> |
|||
==Epidemiology== |
|||
Urinary tract infections are the most frequent bacterial infection in women.<ref name=AFP2011>{{cite journal |last1=Colgan |first1=R |author2=Williams, M|title=Diagnosis and treatment of acute uncomplicated cystitis.|journal=American family physician|date=2011-10-01|volume=84|issue=7|pages=771–6|pmid=22010614}}</ref> They occur most frequently between the ages of 16 and 35 years, with 10% of women getting an infection yearly and 60% having an infection at some point in their lives.<ref name=Review08/><ref name=Sal2011>{{cite journal |last1=Salvatore |first1=S |author2=Salvatore, S, Cattoni, E, Siesto, G, Serati, M, Sorice, P, Torella, M|title=Urinary tract infections in women.|journal=European journal of obstetrics, gynecology, and reproductive biology|date=June 2011|volume=156|issue=2|pages=131–6|pmid=21349630|doi=10.1016/j.ejogrb.2011.01.028}}</ref> Recurrences are common, with nearly half of people getting a second infection within a year.<!-- <ref name=Sal2011/> --> Urinary tract infections occur four times more frequently in females than males.<ref name=Sal2011/> Pyelonephritis occurs between 20–30 times less frequently.<ref name=Review08/> They are the most common cause of [[Nosocomial infection|hospital acquired infections]] accounting for approximately 40%.<ref name=Nurse2010>{{cite book|title=Brunner & Suddarth's textbook of medical-surgical nursing.|year=2010|publisher=Wolters Kluwer Health/Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0-7817-8589-1|page=1359|url=https://books.google.com/books?id=SmtjSD1x688C&pg=PA1359|edition=12th}}</ref> Rates of asymptomatic bacteria in the urine increase with age from two to seven percent in women of child bearing age to as high as 50% in elderly women in care homes.<ref name=NA2011/> Rates of asymptomatic bacteria in the urine among men over 75 are between 7-10%.<ref name=Elder2011>{{cite journal |last1=Woodford |first1=HJ |author2=George, J |title=Diagnosis and management of urinary infections in older people |journal= [[Clinical Medicine]] |location= London |date=February 2011|volume=11|issue=1|pages=80–3|pmid=21404794 |doi=10.7861/clinmedicine.11-1-80}}</ref> Asymptomatic bacteria in the urine occurs in 2% to 10% of pregnancies.<ref name="Smaill-2007">{{Cite journal | last1 = Smaill | first1 = F. | last2 = Vazquez | first2 = JC. | title = Antibiotics for asymptomatic bacteriuria in pregnancy. | journal = Cochrane Database Syst Rev | volume = | issue = 2 | pages = CD000490 | year = 2007 | doi = 10.1002/14651858.CD000490.pub2 | PMID = 17443502 }}</ref> |
|||
Urinary tract infections may affect 10% of people during childhood.<ref name=Sal2011/> Among children urinary tract infections are the most common in uncircumcised males less than three months of age, followed by females less than one year.<ref name=PeadsNA2011/> Estimates of frequency among children however vary widely. In a group of children with a fever, ranging in age between birth and two years, two to 20% were diagnosed with a UTI.<ref name=PeadsNA2011/> |
|||
==Society and culture== |
|||
In the United States, urinary tract infections account for nearly seven million office visits, a million emergency department visits, and one hundred thousand hospitalizations every year.<ref name=Sal2011/> The cost of these infections is significant both in terms of lost time at work and costs of medical care.<!-- <ref name=Nurse2010/> --> In the United States the direct cost of treatment is estimated at 1.6 billion USD yearly.<ref name=Nurse2010/> |
|||
==History== |
|||
Urinary tract infections have been described since ancient times with the first documented description in the [[Ebers Papyrus]] dated to c. 1550 BC.<ref name=His2008>{{cite book|last=Al-Achi|first=Antoine|title=An introduction to botanical medicines : history, science, uses, and dangers|year=2008|publisher=Praeger Publishers|location=Westport, Conn.|isbn=978-0-313-35009-2|page=126|url=https://books.google.com/books?id=HMzxKua4_rcC&pg=PA126}}</ref> It was described by the Egyptians as "sending forth heat from the bladder".<ref>{{cite book|last=Wilson...]|first=[general ed.: Graham|title=Topley and Wilson's Principles of bacteriology, virology and immunity : in 4 volumes|year=1990|publisher=Arnold|location=London|isbn=0-7131-4591-9|page=198|edition=8.}}</ref> Effective treatment did not occur until the development and availability of antibiotics in the 1930s before which time herbs, [[bloodletting]] and rest were recommended.<ref name=His2008/> |
|||
==Pregnancy== |
|||
Urinary tract infections are more concerning in [[pregnancy]] due to the increased risk of kidney infections.<!-- <ref name=NA2011/> --> During pregnancy, high [[progesterone]] levels elevate the risk of decreased muscle tone of the ureters and bladder, which leads to a greater likelihood of reflux, where urine flows back up the ureters and towards the kidneys.<!-- <ref name=NA2011/> --> While pregnant women do not have an increased risk of asymptomatic bacteriuria, if bacteriuria is present they do have a 25–40% risk of a kidney infection.<ref name=NA2011/> Thus if urine testing shows signs of an infection—even in the absence of symptoms—treatment is recommended.<!-- <ref name=Preg10/> --> [[Cephalexin]] or [[nitrofurantoin]] are typically used because they are generally considered safe in pregnancy.<ref name=Preg10>{{cite journal|author1=Guinto, V.T.|author2=De Guia, B.|author3=Festin, M.R.|author4=Dowswell, T.|journal=Cochrane Database of Systematic Reviews|volume=|issue=9|pages=CD007855|year=2010|pmid=20824868|doi=10.1002/14651858.CD007855.pub2|editor1-last=Guinto|editor1-first=Valerie T|title=Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy}}</ref> A kidney infection during pregnancy may result in [[premature birth]] or [[pre-eclampsia]] (a state of [[hypertension|high blood pressure]] and kidney dysfunction during pregnancy that can lead to [[seizures]]).<ref name=NA2011/> |
|||
{{Hidden end}} |
|||
== 参考文獻 == |
== 参考文獻 == |
||
2016年1月4日 (一) 12:56的版本
| 泌尿道感染 (Urinary tract infection) | |
|---|---|
 | |
| 在尿鏡檢驗(urinary microscopy)下,泌尿道感染患者的尿液的白細胞中出現多個桿狀細菌 | |
| 症状 | 血尿、发热、排尿灼熱感、肚痛、頻尿症 |
| 类型 | 膀胱炎、傳染病、泌尿系統疾病[*]、细菌感染疾病[*]、疾病 |
| 分类和外部资源 | |
| 醫學專科 | 泌尿外科 |
| ICD-11 | GC00.1 |
| ICD-10 | N39.0 |
| ICD-9-CM | 599.0 |
| DiseasesDB | 13657 |
| MedlinePlus | 000521 |
| eMedicine | emerg/625 emerg/626 |
| MeSH | D014552 |
泌尿道感染(urinary tract infection,UTI),也稱為急性膀胱炎或膀胱感染,是一種會影響到部分泌尿道的感染[1]。泌尿道分為上、下泌尿道,感染部位不同對應到不同疾病名稱:當影響到下泌尿道,稱為膀胱炎;當影響到上泌尿道,也就是腎臟的時候,則稱為腎盂腎炎[2]。
不同感染位置,症狀會稍有不同:下泌尿道感染的症狀主要是解尿時會疼痛,也可能會有頻尿或是一直想要解尿的感覺;上泌尿道感染除了會有跟下泌尿道感染同樣症狀外,還會有發燒、腹痛的症狀。有些情況,可能沒有解尿也能感受到尿道灼熱痛感。年長者和很年輕的人若感染,以上症狀可能不會表現得十分明顯。最常見造成泌尿道感染(上下都可能)的病菌是大腸桿菌,而其他細菌、病毒或黴菌則鮮少造成感染。
女性其尿道較短,肛門和尿道開口距離也較近,因此較容易有泌尿道感染[中1],約過半數的 女性在其一生中有出現過泌尿道感染的情形。泌尿道感染也常會復發。其他的危險因子還包括性交及家族病史。若有出現腎盂腎炎,可能是因為膀胱感染而引起,但 也可能是因為菌血症而造成。若病患是年輕健康的女性,泌尿道感染可以只以其症狀來診斷。針對一些模糊的症狀,會比較不容易診斷,因為可能有些部位已有 細菌存在,只是沒有感染症狀。若是有併發症或是治療不成功的例子,可以進行尿液培養,若頻繁感染,可用低劑量抗生素進行預防性醫療。
若是沒有併發症的泌尿道感染,可以用短療程抗生素進行治療,不過不少抗生素已用來治療泌尿 道感染,細菌抗生素抗藥性也漸漸提高。若是已有併發症,需要長療程的抗生素或是注射抗生素,若症狀在二至三天還沒有改善,需要進一步的诊断测试。 在女性中,泌尿道感染是最常見的細菌感染,每年約會增加10%。若病患在尿液中有病菌或白血球,但沒有症狀,一般不建議使用抗生素,但若病患是已懷孕的婦 女,仍需使用抗生素。
体征和症状

下泌尿道感染也稱為膀胱感染。最常見的症狀是排尿時有灼熱感與頻尿(或是有排尿的慾望)伴隨著沒有陰道分泌物與明顯的疼痛[3]。這些症狀可能輕微,也可能嚴重[2],在健康女性身上會持續平均六天[4],恥骨與下背部可能會出現些疼痛感。經歷過上泌尿道感染或是腎盂腎炎的人,可能會有側腹痛,發燒,或是反胃噁心的經驗,以及不同於典型下泌尿道感染的不適症狀。但比較少出現尿中帶血[5]或尿中出現肉眼可見的膿的症狀[6]。
兒童
對於年幼兒童來說,泌尿道感染的唯一可能症狀是發燒。也因為缺乏明顯的症狀,若兩歲以下女嬰或是未割包皮的一歲以下男嬰有發燒症狀時,醫療機構通常會建議進行尿液培養(culture of urine)。嬰兒泌尿道感染的症狀通常會有食慾降低、嘔吐、嗜睡、或黃疸等;年紀較大的兒童則會有尿失禁的現象[7]。
老年人
尿道的症狀在老年人中並不常見[8],它呈現的方式不明顯,但會有尿失禁、 心理狀態的改變或是疲勞,是其少數可觀察到的症狀[2]。醫護人員可能會在一些患者檢測到敗血病-血液感染[5]。因為很多老年人可能已有尿失禁或失智症等問題,因此常造成診斷上的複雜性[8]。
若出現生理系統感染症狀,且無法回報尿道症狀的病患中(例如有進階失智症的情形),合理的作法是進行尿液培養.[9]。生理系統性的感染徵兆包括發燒、正常體溫上升多於1.1 °C (2.0 °F)、寒顫和血液中白血球的增加[9]。
病因
大腸桿菌引起80%~85%的社區性泌尿道感染,而大約5%~10%是由於腐生葡萄球菌所造成的[3],還有極少數是因病毒或是真菌而感染的[10]。院內的泌尿道感染(大部分和導尿管有關)包含了非常廣泛的致病原:包括大腸桿菌(27%)、克雷白氏桿菌(11%)、綠膿桿菌(11%)、真菌病原體白色念珠菌(9%)、腸球菌(7%)[5][11][12]。金黃色葡萄球菌而造成的泌尿道感染,其比率僅次於由血液傳播而造成的感染[2]。披衣菌和黴漿菌會感染尿道,但不會感染膀胱[13]。這些感染通常被分類為尿道炎而非泌尿道感染。
性
在性行為活躍的年輕女性中,75-90%膀胱感染是由性行為引起,且感染的風險與性愛頻率相關[3] 。蜜月膀胱炎(honeymoon cystitis)的術語已經用來描述在婚姻初期常患有上尿道感染疾病的現象。在停經後的婦女,性行為不會影響尿道感染的風險。在不考慮性交頻率的情況下,殺精劑(Spermicide)的使用將會增加泌尿道感染的風險[3]。而隔膜(Diaphragm)的使用也會有相同的影響[14]。使用避孕套但不用殺精劑,或服用避孕藥(birth control pills)不會提高無併發症的尿道感染風險[3][15]。
與男性相較,女性是屬於尿道感染疾病的較高風險群。其原因在於女性的尿道較短,且較接近肛門[16]。此外,當女性的雌激素(estrogen)隨著停經(menopause)而減少分泌時,尿道感染的機率也會提高,原因是缺少了陰道菌群(vaginal flora)[16]的保護功能。另外,停經也會導致陰道萎縮(vaginal atrophy),進而造成尿道感染疾病的復發[17]。
。慢性前列腺炎(chronic prostitis)也會導致男性尿道感染疾病的復發[18]。其感染風險也會隨著男性的年齡增長提高[18]。而較高齡男性的尿液中普遍上都有細菌的存在,故此點不列入影響尿道感染風險的討論[18]。
導尿
導尿会增加尿道感染的風險。菌尿症(尿裡面有細菌)的風險是每天介乎3-6%, 而預防性的抗生素對正在減少的徵狀性感染是沒有效果的[16]。降低感染風險的方式有:只在有需要的情況下進行導尿、使用無菌操作插入方式、和保持封閉的、沒有堵塞的導尿管排尿[19][20][21]。
男性潛水員使用陰莖套導管,女性潛水員在乾式潛水衣使用外在捕捉器具(external catching device)也比較容易有泌尿道感染的問題[22]。
其他
基因遺傳可能引起泌尿道感染.其他可能造成風險的因素有糖尿病[3],男性未接受割禮,及攝護腺肥大[2]。其他複雜的因素相當的模糊,包括誘發結構性,功能性,或是代謝上的異常[23]。對於兒童,泌尿道感染與膀胱輸尿管返流(尿液)從膀胱到輸尿管或腎臟的異常流動)及便秘有關連[7]。
患有脊椎損傷的人因為長期使用導尿管及排尿的功能異常,有更高泌尿道感染的風險[24].這是此群體受到感染的主要原因之一,也是他們住院的主要緣由[24]。而且蔓越莓汁與蔓越莓補給品對這些人群的預防與治療沒有呈現效果[25]。
Pathogenesis
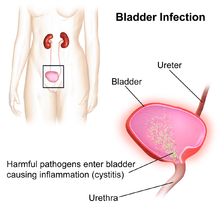
The bacteria that cause urinary tract infections typically enter the bladder via the urethra. However, infection may also occur via the blood or lymph. It is believed that the bacteria are usually transmitted to the urethra from the bowel, with females at greater risk due to their anatomy. After gaining entry to the bladder, E. Coli are able to attach to the bladder wall and form a biofilm that resists the body's immune response.[5]
Diagnosis
In straightforward cases, a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation. In complicated or questionable cases, it may be useful to confirm the diagnosis via urinalysis, looking for the presence of urinary nitrites, white blood cells (leukocytes), or leukocyte esterase.[27] Another test, urine microscopy, looks for the presence of red blood cells, white blood cells, or bacteria. Urine culture is deemed positive if it shows a bacterial colony count of greater than or equal to 103 colony-forming units per mL of a typical urinary tract organism. Antibiotic sensitivity can also be tested with these cultures, making them useful in the selection of antibiotic treatment. However, women with negative cultures may still improve with antibiotic treatment.[3] As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.[8]
Classification
A urinary tract infection may involve only the lower urinary tract, in which case it is known as a bladder infection. Alternatively, it may involve the upper urinary tract, in which case it is known as pyelonephritis. If the urine contains significant bacteria but there are no symptoms, the condition is known as asymptomatic bacteriuria.[2] If a urinary tract infection involves the upper tract, and the person has diabetes mellitus, is pregnant, is male, or immunocompromised, it is considered complicated.[4][5] Otherwise if a woman is healthy and premenopausal it is considered uncomplicated.[4] In children when a urinary tract infection is associated with a fever, it is deemed to be an upper urinary tract infection.[7]
Children
To make the diagnosis of a urinary tract infection in children, a positive urinary culture is required. Contamination poses a frequent challenge depending on the method of collection used, thus a cutoff of 105 CFU/mL is used for a "clean-catch" mid stream sample, 104 CFU/mL is used for catheter-obtained specimens, and 102 CFU/mL is used for suprapubic aspirations (a sample drawn directly from the bladder with a needle). The use of "urine bags" to collect samples is discouraged by the World Health Organization due to the high rate of contamination when cultured, and catheterization is preferred in those not toilet trained. Some, such as the American Academy of Pediatrics recommends renal ultrasound and voiding cystourethrogram (watching a person's urethra and urinary bladder with real time x-rays while they urinate) in all children less than two years old who have had a urinary tract infection. However, because there is a lack of effective treatment if problems are found, others such as the National Institute for Health and Care Excellence only recommends routine imaging in those less than six months old or who have unusual findings.[7]
Differential diagnosis
In women with cervicitis (inflammation of the cervix) or vaginitis (inflammation of the vagina) and in young men with UTI symptoms, a Chlamydia trachomatis or Neisseria gonorrheae infection may be the cause.[2][28] These infections are typically classified as a urethritis rather than a urinary tract infection. Vaginitis may also be due to a yeast infection.[29] Interstitial cystitis (chronic pain in the bladder) may be considered for people who experience multiple episodes of UTI symptoms but urine cultures remain negative and not improved with antibiotics.[30] Prostatitis (inflammation of the prostate) may also be considered in the differential diagnosis.[31]
Hemorrhagic cystitis, characterized by blood in the urine, can occur secondary to a number of causes including: infections, radiation therapy, underlying cancer, medications and toxins.[32] Medications that commonly cause this problem include the chemotherapeutic agent cyclophosphamide with rates of 2 to 40%.[32] Eosinophilic cystitis is a rare condition where eosinophiles are present in the bladder wall.[33] Signs and symptoms are similar to a bladder infection.[33] Its cause is not entirely clear; however, it may be linked to food allergies, infections, and medications among others.[34]
Prevention
A number of measures have not been confirmed to affect UTI frequency including: urinating immediately after intercourse, the type of underwear used, personal hygiene methods used after urinating or defecating, or whether a person typically bathes or showers.[3] There is similarly a lack of evidence surrounding the effect of holding one's urine, tampon use, and douching.[16] In those with frequent urinary tract infections who use spermicide or a diaphragm as a method of contraception, they are advised to use alternative methods.[5] In those with benign prostatic hyperplasia urinating in a sitting position appears to improve bladder emptying which might decrease urinary tract infections in this group.[35]
Using urinary catheters as little and as short of time as possible and appropriate care of the catheter when used prevents infections.[19] They should be inserted using sterile technique in hospital however non-sterile technique may be appropriate in those who self catheterize.[21] The urinary catheter set up should also be kept sealed.[21] Evidence does not support a significant decrease in risk when silver-alloy catheters are used.[36]
Medications
For those with recurrent infections, taking a short course of antibiotics when each infection occurs is associated with the lowest antibiotic use.[37] A prolonged course of daily antibiotics is also effective.[3] Medications frequently used include nitrofurantoin and trimethoprim/sulfamethoxazole (TMP/SMX).[5] Methenamine is another agent used for this purpose as in the bladder where the acidity is low it produces formaldehyde to which resistance does not develop.[38] Some recommend against prolonged use due to concerns of antibiotic resistance.[37]
In cases where infections are related to intercourse, taking antibiotics afterwards may be useful.[5] In post-menopausal women, topical vaginal estrogen has been found to reduce recurrence. As opposed to topical creams, the use of vaginal estrogen from pessaries has not been as useful as low dose antibiotics.[39] Antibiotics following short term urinary catheterization decreases the subsequent risk of a bladder infection.[40] A number of vaccines are in development as of 2011.[5]
Children
The evidence that preventative antibiotics decrease urinary tract infections in children is poor.[41] However recurrent UTIs are a rare cause of further kidney problems if there are no underlying abnormalities of the kidneys, resulting in less than a third of a percent (0.33%) of chronic kidney disease in adults.[42] Whether routine circumcisions prevents UTIs has not been well studied as of 2011.[43]
Alternative medicine
Some research suggests that cranberry (juice or capsules) may decrease the number of UTIs in those with frequent infections.[44][45] A Cochrane review concluded that the benefit, if it exists, is small.[46] Long-term tolerance is also an issue[46] with gastrointestinal upset occurring in more than 30%.[47] Cranberry juice is thus not currently recommended for this indication.[46] As of 2011, intravaginal probiotics require further study to determine if they are beneficial.[5]
Treatment
The mainstay of treatment is antibiotics. Phenazopyridine is occasionally prescribed during the first few days in addition to antibiotics to help with the burning and urgency sometimes felt during a bladder infection.[48] However, it is not routinely recommended due to safety concerns with its use, specifically an elevated risk of methemoglobinemia (higher than normal level of methemoglobin in the blood).[49] Acetaminophen (paracetamol) may be used for fevers.[50] There is no good evidence for the use of cranberry products for treating current infections.[51][52]
Asymptomatic bacteriuria
Those who have bacteria in the urine but no symptoms should not generally be treated with antibiotics.[53] This includes those who are old, those with spinal cord injuries, and those who have urinary catheters.[54][55] Pregnancy is an exception and it is recommended that women take 7 days of antibiotics.[56][57] If not treated it causes up to 30% of mothers to develop pyelonephritis and increases risk of low birth weight and preterm birth.[58] Some also support treatment of those with diabetes mellitus[59] and treatment before urinary tract procedures which will likely cause bleeding.[55]
Uncomplicated
Uncomplicated infections can be diagnosed and treated based on symptoms alone.[3] Oral antibiotics such as trimethoprim/sulfamethoxazole (TMP/SMX), nitrofurantoin, or fosfomycin are typically first line.[60] Cephalosporins, amoxicillin/clavulanic acid, or a fluoroquinolone may also be used.[61] However, resistance to fluoroquinolones among the bacterial that cause urinary infections has been increasing.[27] These medications substantially shorten the time to recovery with all being equally effective.[61][62] A three-day treatment with trimethoprim, TMP/SMX, or a fluoroquinolone is usually sufficient, whereas nitrofurantoin requires 5–7 days.[3][63] Fosfomycin may be used as a single dose but has been associated with lower rates of efficacy.[27]
With treatment, symptoms should improve within 36 hours.[4] About 50% of people will recover without treatment within a few days or weeks.[3] Fluoroquinolones are not recommended as a first treatment.[27][64] The Infectious Diseases Society of America states this due to the concern of generating resistance to this class of medication.[63] Amoxicillin-clavulanate appears less effective than other options.[65] Despite this precaution, some resistance has developed to all of these medications related to their widespread use.[3] Trimethoprim alone is deemed to be equivalent to TMP/SMX in some countries.[63] For simple UTIs, children often respond to a three-day course of antibiotics.[66] Women with recurrent simple UTIs may benefit from self-treatment upon occurrence of symptoms with medical follow-up only if the initial treatment fails.[3]
Complicated
Complicated UTIs are more difficult to treat and usually requires more aggressive evaluation, treatment and follow-up.[67] It may require identifying and addressing the underlying complication.[68] Increasing antibiotic resistance is causing concern about the future of treating those with complicated and recurrent UTI.[69][70]
Pyelonephritis
Pyelonephritis is treated more aggressively than a simple bladder infection using either a longer course of oral antibiotics or intravenous antibiotics.[71] Seven days of the oral fluoroquinolone ciprofloxacin is typically used in areas where the resistance rate is less than 10%. If the local resistance rates are greater than 10%, a dose of intravenous ceftriaxone is often prescribed.[71] Trimethoprim/sulfamethoxazole or amoxicillin/clavulanate orally for 14 days is another reasonable option.[72] In those who exhibit more severe symptoms, admission to a hospital for ongoing antibiotics may be needed.[71] Complications such as urinary obstruction from a kidney stone may be considered if symptoms do not improve following two or three days of treatment.[2][71]
Epidemiology
Urinary tract infections are the most frequent bacterial infection in women.[4] They occur most frequently between the ages of 16 and 35 years, with 10% of women getting an infection yearly and 60% having an infection at some point in their lives.[3][5] Recurrences are common, with nearly half of people getting a second infection within a year. Urinary tract infections occur four times more frequently in females than males.[5] Pyelonephritis occurs between 20–30 times less frequently.[3] They are the most common cause of hospital acquired infections accounting for approximately 40%.[73] Rates of asymptomatic bacteria in the urine increase with age from two to seven percent in women of child bearing age to as high as 50% in elderly women in care homes.[16] Rates of asymptomatic bacteria in the urine among men over 75 are between 7-10%.[8] Asymptomatic bacteria in the urine occurs in 2% to 10% of pregnancies.[58]
Urinary tract infections may affect 10% of people during childhood.[5] Among children urinary tract infections are the most common in uncircumcised males less than three months of age, followed by females less than one year.[7] Estimates of frequency among children however vary widely. In a group of children with a fever, ranging in age between birth and two years, two to 20% were diagnosed with a UTI.[7]
Society and culture
In the United States, urinary tract infections account for nearly seven million office visits, a million emergency department visits, and one hundred thousand hospitalizations every year.[5] The cost of these infections is significant both in terms of lost time at work and costs of medical care. In the United States the direct cost of treatment is estimated at 1.6 billion USD yearly.[73]
History
Urinary tract infections have been described since ancient times with the first documented description in the Ebers Papyrus dated to c. 1550 BC.[74] It was described by the Egyptians as "sending forth heat from the bladder".[75] Effective treatment did not occur until the development and availability of antibiotics in the 1930s before which time herbs, bloodletting and rest were recommended.[74]
Pregnancy
Urinary tract infections are more concerning in pregnancy due to the increased risk of kidney infections. During pregnancy, high progesterone levels elevate the risk of decreased muscle tone of the ureters and bladder, which leads to a greater likelihood of reflux, where urine flows back up the ureters and towards the kidneys. While pregnant women do not have an increased risk of asymptomatic bacteriuria, if bacteriuria is present they do have a 25–40% risk of a kidney infection.[16] Thus if urine testing shows signs of an infection—even in the absence of symptoms—treatment is recommended. Cephalexin or nitrofurantoin are typically used because they are generally considered safe in pregnancy.[76] A kidney infection during pregnancy may result in premature birth or pre-eclampsia (a state of high blood pressure and kidney dysfunction during pregnancy that can lead to seizures).[16]
参考文獻
- ^ Mayo Clinic Staff. Diseases and Conditions - Urinary tract infection (UTI). Mayo Clinic. August 29, 2012.
- ^ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Lane, DR; Takhar, SS. Diagnosis and management of urinary tract infection and pyelonephritis.. Emergency medicine clinics of North America. August 2011, 29 (3): 539–52. PMID 21782073. doi:10.1016/j.emc.2011.04.001.
- ^ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Nicolle LE. Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis. Urol Clin North Am. 2008, 35 (1): 1–12, v. PMID 18061019. doi:10.1016/j.ucl.2007.09.004.
- ^ 4.0 4.1 4.2 4.3 4.4 Colgan, R; Williams, M. Diagnosis and treatment of acute uncomplicated cystitis.. American family physician. 2011-10-01, 84 (7): 771–6. PMID 22010614.
- ^ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 Salvatore, S; Salvatore, S, Cattoni, E, Siesto, G, Serati, M, Sorice, P, Torella, M. Urinary tract infections in women.. European journal of obstetrics, gynecology, and reproductive biology. June 2011, 156 (2): 131–6. PMID 21349630. doi:10.1016/j.ejogrb.2011.01.028.
- ^ Arellano, Ronald S. Non-vascular interventional radiology of the abdomen. New York: Springer. : 67. ISBN 978-1-4419-7731-1.
- ^ 7.0 7.1 7.2 7.3 7.4 7.5 Bhat, RG; Katy, TA, Place, FC. Pediatric urinary tract infections.. Emergency medicine clinics of North America. August 2011, 29 (3): 637–53. PMID 21782079. doi:10.1016/j.emc.2011.04.004.
- ^ 8.0 8.1 8.2 8.3 Woodford, HJ; George, J. Diagnosis and management of urinary infections in older people. Clinical Medicine (London). February 2011, 11 (1): 80–3. PMID 21404794. doi:10.7861/clinmedicine.11-1-80.
- ^ 9.0 9.1 AMDA – The Society for Post-Acute and Long-Term Care Medicine, Ten Things Physicians and Patients Should Question, Choosing Wisely: an initiative of the ABIM Foundation (AMDA – The Society for Post-Acute and Long-Term Care Medicine), February 2014 [20 April 2015]
- ^ Amdekar, S; Singh, V, Singh, DD. Probiotic therapy: immunomodulating approach toward urinary tract infection.. Current microbiology. November 2011, 63 (5): 484–90. PMID 21901556. doi:10.1007/s00284-011-0006-2.
- ^ Sievert DM, Ricks P, Edwards JR, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol. January 2013, 34 (1): 1–14. PMID 23221186. doi:10.1086/668770.
- ^ Bagshaw, SM; Laupland, KB. Epidemiology of intensive care unit-acquired urinary tract infections.. Current opinion in infectious diseases. Feb 2006, 19 (1): 67–71. PMID 16374221. doi:10.1097/01.qco.0000200292.37909.e0.
- ^ Urinary Tract Infections in Adults. [January 1, 2015].
- ^ Franco, AV. Recurrent urinary tract infections.. Best practice & research. Clinical obstetrics & gynaecology. December 2005, 19 (6): 861–73. PMID 16298166. doi:10.1016/j.bpobgyn.2005.08.003.
- ^ Engleberg, N C; DiRita, V; Dermody, T S. Schaechter's Mechanism of Microbial Disease. Baltimore: Lippincott Williams & Wilkins. 2007. ISBN 978-0-7817-5342-5.
- ^ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 Dielubanza, EJ; Schaeffer, AJ. Urinary tract infections in women.. The Medical clinics of North America. January 2011, 95 (1): 27–41. PMID 21095409. doi:10.1016/j.mcna.2010.08.023.
- ^ Goldstein, I; Dicks, B; Kim, NN; Hartzell, R. Multidisciplinary overview of vaginal atrophy and associated genitourinary symptoms in postmenopausal women.. Sexual medicine. December 2013, 1 (2): 44–53. PMID 25356287. doi:10.1002/sm2.17.
- ^ 18.0 18.1 18.2 Lipsky, BA. Prostatitis and urinary tract infection in men: what's new; what's true?. The American journal of medicine. March 1999, 106 (3): 327–34. PMID 10190383. doi:10.1016/s0002-9343(99)00017-0.
- ^ 19.0 19.1 Nicolle LE. The chronic indwelling catheter and urinary infection in long-term-care facility residents. Infect Control Hosp Epidemiol. 2001, 22 (5): 316–21. PMID 11428445. doi:10.1086/501908.
- ^ Phipps, S.; Lim, Y.N.; McClinton, S.; Barry, C.; Rane, A.; N'Dow, J. Phipps, Simon , 编. Short term urinary catheter policies following urogenital surgery in adults. Cochrane Database of Systematic Reviews. 2006, (2): CD004374. PMID 16625600. doi:10.1002/14651858.CD004374.pub2.
- ^ 21.0 21.1 21.2 Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010, 31 (4): 319–26. PMID 20156062. doi:10.1086/651091.
- ^ Harris, Richard. Genitourinary infection and barotrauma as complications of 'P-valve' use in drysuit divers. Diving and Hyperbaric Medicine : the Journal of the South Pacific Underwater Medicine Society. December 2009, 39 (4): 210–2 [2013-04-04]. PMID 22752741.
- ^ Infectious Disease, Chapter Seven, Urinary Tract Infections from Infectious Disease Section of Microbiology and Immunology On-line. By Charles Bryan MD. University of South Carolina. This page last changed on Wednesday, April 27, 2011
- ^ 24.0 24.1 Eves, FJ; Rivera, N. Prevention of urinary tract infections in persons with spinal cord injury in home health care.. Home healthcare nurse. April 2010, 28 (4): 230–41. PMID 20520263. doi:10.1097/NHH.0b013e3181dc1bcb.
- ^ Opperman, EA. Cranberry is not effective for the prevention or treatment of urinary tract infections in individuals with spinal cord injury.. Spinal cord. June 2010, 48 (6): 451–6. PMID 19935757. doi:10.1038/sc.2009.159.
- ^ Bladder infection. Blausen Medical. [4 November 2015].
- ^ 27.0 27.1 27.2 27.3 Detweiler K, Mayers D, Fletcher SG. Bacteruria and Urinary Tract Infections in the Elderly. The Urologic Clinics of North America (Review). November 2015, 42 (4): 561–8. PMID 26475952. doi:10.1016/j.ucl.2015.07.002.
- ^ Raynor, MC; Carson CC, 3rd. Urinary infections in men.. The Medical clinics of North America. January 2011, 95 (1): 43–54. PMID 21095410. doi:10.1016/j.mcna.2010.08.015.
- ^ Leung, David Hui; edited by Alexander; Padwal, Raj. Approach to internal medicine : a resource book for clinical practice 3rd. New York: Springer. : 244. ISBN 978-1-4419-6504-2.
- ^ Kursh, edited by Elroy D.; Ulchaker, James C. Office urology. Totowa, N.J.: Humana Press. 2000: 131. ISBN 978-0-89603-789-2.
- ^ Walls, authors, Nathan W. Mick, Jessica Radin Peters, Daniel Egan; editor, Eric S. Nadel; advisor, Ron. Blueprints emergency medicine 2nd. Baltimore, Md.: Lippincott Williams & Wilkins. 2006: 152. ISBN 978-1-4051-0461-6.
- ^ 32.0 32.1 Keane, edited by Sam D. Graham, Thomas E. Glenn's urologic surgery 7th. Philadelphia, Pa.: Lippincott Williams & Wilkins. 2009: 148. ISBN 9780781791410.
- ^ 33.0 33.1 Kramer, ed. by A. Barry Belman; Lowell R. King; Stephen A. Clinical pediatric urology 4. London: Dunitz. 2002: 338. ISBN 9781901865639.
- ^ Popescu, OE; Landas, SK; Haas, GP. The spectrum of eosinophilic cystitis in males: case series and literature review.. Archives of pathology & laboratory medicine. February 2009, 133 (2): 289–94. PMID 19195972. doi:10.1043/1543-2165-133.2.289.
- ^ de Jong, Y; Pinckaers, JH; Ten Brinck, RM; Lycklama À Nijeholt, AA; Dekkers, OM. Urinating Standing versus Sitting: Position Is of Influence in Men with Prostate Enlargement. A Systematic Review and Meta-Analysis.. PLoS ONE. 2014, 9 (7): e101320. PMC 4106761
 . PMID 25051345. doi:10.1371/journal.pone.0101320.
. PMID 25051345. doi:10.1371/journal.pone.0101320.
- ^ Lam, TB; Omar, MI; Fisher, E; Gillies, K; MacLennan, S. Types of indwelling urethral catheters for short-term catheterisation in hospitalised adults.. The Cochrane database of systematic reviews. Sep 23, 2014, 9: CD004013. PMID 25248140. doi:10.1002/14651858.CD004013.pub4.
- ^ 37.0 37.1 Recurrent uncomplicated cystitis in women: allowing patients to self-initiate antibiotic therapy.. Rev Prescire. Nov 2013, 22 (361): 835–837. PMID 24669389.
- ^ Cubeddu, Richard Finkel, Michelle A. Clark, Luigi X. Pharmacology 4th. Philadelphia: Lippincott Williams & Wilkins. 2009: 397. ISBN 9780781771559.
- ^ Perrotta, C; Aznar, M, Mejia, R, Albert, X, Ng, CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women.. Cochrane database of systematic reviews (Online). 2008-04-16, (2): CD005131. PMID 18425910. doi:10.1002/14651858.CD005131.pub2.
- ^ Marschall J, Carpenter CR, Fowler S, Trautner BW. Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analysis. BMJ. 2013, 346: f3147. PMC 3678514
 . PMID 23757735. doi:10.1136/bmj.f3147.
. PMID 23757735. doi:10.1136/bmj.f3147.
- ^ Dai, B; Liu, Y; Jia, J; Mei, C. Long-term antibiotics for the prevention of recurrent urinary tract infection in children: a systematic review and meta-analysis. Archives of Disease in Childhood. 2010, 95 (7): 499–508. PMID 20457696. doi:10.1136/adc.2009.173112.
- ^ Salo, J; Ikäheimo, R, Tapiainen, T, Uhari, M. Childhood urinary tract infections as a cause of chronic kidney disease.. Pediatrics. November 2011, 128 (5): 840–7. PMID 21987701. doi:10.1542/peds.2010-3520.
- ^ Jagannath, VA; Fedorowicz, Z; Sud, V; Verma, AK; Hajebrahimi, S. Routine neonatal circumcision for the prevention of urinary tract infections in infancy.. Cochrane database of systematic reviews (Online). November 14, 2012, 11: CD009129. PMID 23152269. doi:10.1002/14651858.CD009129.pub2.
- ^ Wang CH, Fang CC, Chen NC, et al. Cranberry-containing products for prevention of urinary tract infections in susceptible populations. Arch Intern Med. 2012, 172 (13): 988–96. PMID 22777630. doi:10.1001/archinternmed.2012.3004.
- ^ Wang, CH; Fang, CC; Chen, NC; Liu, SS; Yu, PH; Wu, TY; Chen, WT; Lee, CC; Chen, SC. Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials.. Archives of Internal Medicine. July 9, 2012, 172 (13): 988–96. PMID 22777630. doi:10.1001/archinternmed.2012.3004.
- ^ 46.0 46.1 46.2 Jepson, RG; Williams, G; Craig, JC. Cranberries for preventing urinary tract infections.. Cochrane database of systematic reviews (Online). October 17, 2012, 10: CD001321. PMID 23076891. doi:10.1002/14651858.CD001321.pub5.
- ^ Rossi, R; Porta, S, Canovi, B. Overview on cranberry and urinary tract infections in females.. Journal of Clinical Gastroenterology. September 2010,. 44 Suppl 1: S61–2. PMID 20495471. doi:10.1097/MCG.0b013e3181d2dc8e.
- ^ Gaines, KK. Phenazopyridine hydrochloride: the use and abuse of an old standby for UTI.. Urologic nursing. June 2004, 24 (3): 207–9. PMID 15311491.
- ^ Aronson, edited by Jeffrey K. Meyler's side effects of analgesics and anti-inflammatory drugs. Amsterdam: Elsevier Science. 2008: 219. ISBN 978-0-444-53273-2.
- ^ Glass, [edited by] Jill C. Cash, Cheryl A. Family practice guidelines 2nd. New York: Springer. 2010: 271. ISBN 978-0-8261-1812-7.
- ^ Santillo, VM; Lowe, FC. Cranberry juice for the prevention and treatment of urinary tract infections.. Drugs of today (Barcelona, Spain : 1998). Jan 2007, 43 (1): 47–54. PMID 17315052. doi:10.1358/dot.2007.43.1.1032055.
- ^ Guay, DR. Cranberry and urinary tract infections.. Drugs. 2009, 69 (7): 775–807. PMID 19441868. doi:10.2165/00003495-200969070-00002.
- ^ Ariathianto, Y. Asymptomatic bacteriuria - prevalence in the elderly population.. Australian family physician. Oct 2011, 40 (10): 805–9. PMID 22003486.
- ^ Colgan, R; Nicolle, LE; McGlone, A; Hooton, TM. Asymptomatic bacteriuria in adults.. American family physician. Sep 15, 2006, 74 (6): 985–90. PMID 17002033.
- ^ 55.0 55.1 American Geriatrics Society, Five Things Physicians and Patients Should Question, Choosing Wisely: an initiative of the ABIM Foundation (American Geriatrics Society), [August 1, 2013]
- ^ Widmer, M.; Gülmezoglu, AM.; Mignini, L.; Roganti, A. Duration of treatment for asymptomatic bacteriuria during pregnancy.. Cochrane Database Syst Rev. 2011, (12): CD000491. PMID 22161364. doi:10.1002/14651858.CD000491.pub2.
- ^ Guinto, VT.; De Guia, B.; Festin, MR.; Dowswell, T. Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy.. Cochrane Database Syst Rev. 2010, (9): CD007855. PMID 20824868. doi:10.1002/14651858.CD007855.pub2.
- ^ 58.0 58.1 Smaill, F.; Vazquez, JC. Antibiotics for asymptomatic bacteriuria in pregnancy.. Cochrane Database Syst Rev. 2007, (2): CD000490. PMID 17443502. doi:10.1002/14651858.CD000490.pub2.
- ^ Julka, S. Genitourinary infection in diabetes.. Indian journal of endocrinology and metabolism. Oct 2013, 17 (Suppl1): S83–S87. PMC 3830375
 . PMID 24251228. doi:10.4103/2230-8210.119512.
. PMID 24251228. doi:10.4103/2230-8210.119512.
- ^ Grigoryan, L; Trautner, BW; Gupta, K. Diagnosis and management of urinary tract infections in the outpatient setting: a review.. JAMA. October 22, 2014, 312 (16): 1677–84. PMID 25335150. doi:10.1001/jama.2014.12842.
- ^ 61.0 61.1 Zalmanovici Trestioreanu, A.; Green, H.; Paul, M.; Yaphe, J.; Leibovici, L. Zalmanovici Trestioreanu, Anca , 编. Antimicrobial agents for treating uncomplicated urinary tract infection in women. Cochrane Database of Systematic Reviews. 2010, 10 (10): CD007182. PMID 20927755. doi:10.1002/14651858.CD007182.pub2.
- ^ Jarvis, TR; Chan, L; Gottlieb, T. Assessment and management of lower urinary tract infection in adults (PDF). Australian Prescriber. February 2014, 37 (1): 7–9.
- ^ 63.0 63.1 63.2 Gupta, K; Hooton, TM, Naber, KG, Wullt, B, Colgan, R, Miller, LG, Moran, GJ, Nicolle, LE, Raz, R, Schaeffer, AJ, Soper, DE, Infectious Diseases Society of America, European Society for Microbiology and Infectious, Diseases. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases.. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2011-03-01, 52 (5): e103–20. PMID 21292654. doi:10.1093/cid/ciq257.
- ^ American Urogynecologic Society, Five Things Physicians and Patients Should Question, Choosing Wisely: an initiative of the ABIM Foundation (American Urogynecologic Society), May 5, 2015 [June 1, 2015]
- ^ Knottnerus, BJ; Grigoryan, L; Geerlings, SE; Moll van Charante, EP; Verheij, TJ; Kessels, AG; ter Riet, G. Comparative effectiveness of antibiotics for uncomplicated urinary tract infections: network meta-analysis of randomized trials.. Family practice. December 2012, 29 (6): 659–70. PMID 22516128. doi:10.1093/fampra/cms029.
- ^ Shadi Afzalnia. BestBets: Is a short course of antibiotics better than a long course in the treatment of UTI in children. www.bestbets.org. December 15, 2006.
- ^ Bryan, Charles S. Infectious diseases in primary care. Philadelphia: W.B. Saunders. 2002: 319. ISBN 0-7216-9056-4.
- ^ Wagenlehner, FM.; Vahlensieck, W.; Bauer, HW.; Weidner, W.; Piechota, HJ.; Naber, KG. Prevention of recurrent urinary tract infections.. Minerva Urol Nefrol. Mar 2013, 65 (1): 9–20. PMID 23538307.
- ^ Pallett, A.; Hand, K. Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria.. J Antimicrob Chemother. Nov 2010,. 65 Suppl 3: iii25–33. PMID 20876625. doi:10.1093/jac/dkq298.
- ^ Shepherd, AK.; Pottinger, PS. Management of urinary tract infections in the era of increasing antimicrobial resistance.. Med Clin North Am. Jul 2013, 97 (4): 737–57, xii. PMID 23809723. doi:10.1016/j.mcna.2013.03.006.
- ^ 71.0 71.1 71.2 71.3 Colgan, R; Williams, M, Johnson, JR. Diagnosis and treatment of acute pyelonephritis in women.. American family physician. 2011-09-01, 84 (5): 519–26. PMID 21888302.
- ^ The Sanford Guide to Antimicrobial Therapy 2011 (Guide to Antimicrobial Therapy (Sanford)). Antimicrobial Therapy. 2011: 30. ISBN 1-930808-65-8.
- ^ 73.0 73.1 Brunner & Suddarth's textbook of medical-surgical nursing. 12th. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2010: 1359. ISBN 978-0-7817-8589-1.
- ^ 74.0 74.1 Al-Achi, Antoine. An introduction to botanical medicines : history, science, uses, and dangers. Westport, Conn.: Praeger Publishers. 2008: 126. ISBN 978-0-313-35009-2.
- ^ Wilson...], [general ed.: Graham. Topley and Wilson's Principles of bacteriology, virology and immunity : in 4 volumes 8. London: Arnold. 1990: 198. ISBN 0-7131-4591-9.
- ^ Guinto, V.T.; De Guia, B.; Festin, M.R.; Dowswell, T. Guinto, Valerie T , 编. Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy. Cochrane Database of Systematic Reviews. 2010, (9): CD007855. PMID 20824868. doi:10.1002/14651858.CD007855.pub2.
外部連結
參見
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||
