興奮劑
此條目需要精通或熟悉相關主題的編者參與及協助編輯。 (2017年4月15日) |


興奮劑又稱為中樞神經興奮劑、中樞神經刺激劑(英語:Stimulant),是一系列可刺激中樞神經系統和腦部脊髓的精神藥物統稱,其中包括可以增加活動力的藥物[1]、會令人感到愉快和振奮的藥物,以及有交感興奮作用的藥物[2]。興奮劑可以提升警覺心、注意力和活力,同時也增加血壓、心跳和呼吸[3],常用作處方藥(例如ADHD的兒童或成人[3]、嗜睡症、抑制食慾),但也有用於藥物治療以外的使用(可能是脫法藥物或是非法使用),可能做為表現增強物質或是娛樂性藥物。
一些藥物能影響自我管理能力。例如:歸類為中樞神經興奮劑的藥物:哌甲酯(methylphenidate)和安非他命(amphetamine)。適度適量使用,能提升一個人整體的衝動控制能力(inhibitory control),且被用來治療注意力不足過動症(ADHD)患者。[4][5] 同理,中樞神經抑制劑(depressants)(例如:酒精)由於會讓腦中神經傳導物質濃度降低、減少許多大腦區域的活性等,所以可能會造成專注力、神智清醒度等自我管理能力的下降。[6]
在美國,2013年最常用的處方藥興奮劑有甲磺酸賴氨酸安非他命、哌甲酯及安非他命[7]。
作用機制
[編輯]大多數興奮劑通過增強兒茶酚胺神經傳遞發揮其激活作用。兒茶酚胺神經遞質被用於涉及注意力、喚醒、動機、任務顯著性和報酬預期的調節途徑中。經典的興奮劑要麼阻止再攝取,要麼刺激這些兒茶酚胺的外排,導致其迴路活動增加。一些興奮劑,特別是那些具有致病和致幻作用的興奮劑,也會影響血清素能的傳遞。一些興奮劑,例如一些苯丙胺衍生物,尤其是育亨賓,可以通過拮抗調節性自體受體來減少負反饋。[8]腎上腺素能激動劑(例如,麻黃鹼)通過直接結合併激活腎上腺素能受體而起作用,產生擬交感神經作用
藥物還可以具有更多間接機制來激發激活作用。例如咖啡因是腺苷受體拮抗劑,僅間接增加兒茶酚胺在大腦中的傳播。[9]而Pitolisant是H3受體反向激動劑。 由於H3受體主要充當自體受體,因此pitolisant減少了對組織胺能神經元的負反饋,從而增強了組織胺能傳遞。
常見的興奮劑
[編輯]安非他命
[編輯]安非他命是苯乙胺類的強力中樞神經系統(CNS)興奮劑,已被批准用於治療注意力不足過動症(ADHD)和發作性嗜睡病。[10]安非他命也可以作為表現增強物質和認知增強劑使用,也可以作為春藥和娛樂用的欣快劑使用。[11][12][13][14]儘管在許多國家或地區,安非他命是處方藥,但未經控製或大量使用會帶來嚴重的健康風險,因此經常嚴格控制安非他命的未經授權擁有和分發。[15][16]因此,許多安非他命是在秘密實驗室非法製造的,並被販運並出售給使用者。[17]根據全世界毒品的緝獲情況,安非他命的非法生產和販運比甲基安非他命要少得多。[17]
第一種藥物安非他命是Benzedrine,這是一種用於治療各種疾病的吸入器品牌。[18][19]由於右旋異構體具有更大的刺激性,因此逐漸停用Benzedrine,轉而使用含有全部或大部分右旋苯丙胺的製劑。目前,通常將其處方為混合的苯丙胺鹽、右旋苯丙胺和甲磺酸賴氨酸安非他命。[18][20]
苯丙胺是去甲基腎上腺素—多巴胺釋放劑(NDRA)。它通過多巴胺轉運體和去甲腎上腺素轉運體進入神經元,並通過激活TAAR1和抑制VMAT2促進神經遞質排出。[21]在治療劑量下,這會引起情緒和認知影響,例如欣快感、性慾改變、喚起感增強和改善認知控制。[12][13][22]同樣,它會誘發身體反應,例如減少反應時間、降低疲勞強度和增加肌肉強度。[11]相比之下,超過治療劑量的安非他命可能會損害認知功能並引起橫紋肌溶解。[10][12][23]超高劑量會導致精神病(例如妄想和偏執狂),即使長期使用治療劑量,這種情況也很少發生。[10][23][24]由於娛樂劑量通常比規定的治療劑量大得多,因此娛樂性使用會產生嚴重的副作用(例如依賴性)的風險要大得多,苯丙胺類藥物的治療很少會出現這種副作用。[10][23][24]
咖啡因
[編輯]
咖啡因是一種興奮性化合物,屬於黃嘌呤類化學物質,天然存在於咖啡、茶和(較小程度上)可可或巧克力中。它包含在許多軟性飲料中,以及大量的能量飲料中。咖啡因是世界上使用最廣泛的精神活性藥物,也是迄今為止最常見的興奮劑。在北美,每天有90%的成年人食用咖啡因。[25]一些司法管轄區限制其銷售和使用。咖啡因也包括在某些藥物中,通常是為了增強主要成分的作用或減少其某項副作用(尤其是嗜睡)。含有標準劑量咖啡因的片劑也可以廣泛獲得。
咖啡因的作用機制不同於許多興奮劑,因為它通過抑制腺苷受體產生興奮作用。[26]腺苷受體被認為是嗜睡和睡眠的主要驅動力,其作用隨著清醒時間的延長而增強。[27]在動物模型中發現咖啡因可增加紋狀體多巴胺,[28]並抑制腺苷受體對多巴胺受體的抑制作用,[29]然而,對人體的影響尚不清楚。與大多數興奮劑不同,咖啡因沒有成癮性。咖啡因似乎不是增強刺激,實際上可能會發生某種程度的厭惡,在NIDA研究專著中發表的一項關於藥物濫用責任的研究中,人們更喜歡安慰劑而不是咖啡因。[30]在大型電話調查中,只有11%的人報告了依賴症狀。然而,當人們在實驗室接受測試時,只有一半聲稱擁有依賴性的人實際經歷過這種情況,這對咖啡因產生依賴性的能力產生了懷疑,並使社會壓力成為人們關注的焦點。[31]
飲用咖啡與降低癌症的總體風險有關。[32]這主要是由於降低了肝細胞癌和子宮內膜癌的風險,但對大腸癌的影響也可能較小。[33]對於其他類型的癌症似乎沒有顯著的保護作用,而大量喝咖啡可能會增加患膀胱癌的風險。[33]咖啡因可能對阿茲海默症有保護作用,但證據尚無定論。[34][35][36]適量喝咖啡可以降低罹患心血管疾病的風險,[37]並且可以在某種程度上降低第2型糖尿病的風險。[38]與少喝或不喝咖啡相比,每天喝1-3杯咖啡不會影響患高血壓的風險。但是,那些每天喝2至4杯的人的患病風險可能會略有增加。[39]咖啡因可增加青光眼患者的眼壓,但似乎不影響正常人。[40]它可以保護人們免於肝硬化。[41]沒有證據表明咖啡會阻礙孩子的成長。[42]咖啡因可能會提高某些藥物的功效,包括用於治療頭痛的藥物。[43]如果在登高海拔的山區幾個小時前服用咖啡因,可能會減輕急性高山症的嚴重程度。[44]
麻黃鹼
[編輯]麻黃鹼是一種擬交感神經胺,其分子結構與眾所周知的藥物苯丙醇胺和甲基苯丙胺,以及重要的神經遞質腎上腺素相似。麻黃鹼通常用作興奮劑、食慾抑制劑、濃縮助劑和減充血藥,並用於治療與麻醉有關的低血壓。
從化學意義上講,它是一種在麻黃屬(麻黃科)的各種植物中發現的具有苯乙胺骨架的生物鹼。其作用主要是通過增加去甲腎上腺素對腎上腺素能受體的活性。[45]它最通常以鹽酸鹽或硫酸鹽的形式出售。
中藥中使用的草藥麻黃(Ephedra sinica)含有麻黃鹼和偽麻黃鹼作為其主要活性成分。含有其他麻黃種類提取物的其他草藥產品也可能如此。
MDMA
[編輯]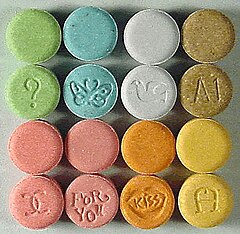
3,4-亞甲二氧基甲基苯丙胺(MDMA, ecstasy,molly)是一種安非他命類的欣快劑、神入感激發劑和興奮劑。[46]一些心理治療師短暫地將其用作治療的輔助手段,該藥物在娛樂中大受歡迎,美國緝毒局將MDMA列為附表I受控物質,禁止大多數醫學研究和應用。MDMA以其神入感激發作用特性而聞名。MDMA的刺激作用包括高血壓,食慾不振,欣快感,社交抑制,失眠(增強清醒/無法入睡),能量改善,喚起感增強和排汗增加等。相對於兒茶酚胺能傳遞,與經典的興奮劑(如安非他命)相比,MDMA顯著增強了血清素能傳遞。MDMA似乎沒有明顯的成癮或依賴性形成。[47]
由於MDMA的相對安全性,一些研究人員(例如David Nutt)批評了調度水平,撰寫了一篇諷刺性的文章,發現MDMA的危險性比馬術低28倍,他稱這種情況為「馬術」或「馬匹成癮綜合症」。[48]
MDPV
[編輯]亞甲基二氧吡咯戊酮(MDPV)是一種興奮性精神藥物,具有刺激性,可作為去甲腎上腺素-多巴胺再攝取抑制劑(NDRI)。[49]它是由勃林格殷格翰公司的一個團隊於1960年代首次開發的。[50]直到2004年左右,MDPV仍然是一種無名的刺激劑,當時有報導稱它是作為設計藥物出售的。標有含MDPV的浴鹽的產品以前曾在美國的加油站和便利店以娛樂性用藥的形式出售,類似於Spice和K2的營銷。[51][52]
甲氧麻黃酮
[編輯]甲氧麻黃酮是苯丙胺和卡西酮類的合成興奮劑。俗名包括drone[55]和MCAT。[56]據報導,它是在中國製造的,化學上類似於在東非卡塔植物中發現的卡西酮化合物。它以片劑或粉劑形式出現,使用者可以吞嚥、鼻腔吸入或注射,產生與搖頭丸、苯丙胺和古柯鹼相似的作用。
甲氧麻黃酮於1929年首次合成,但直到2003年重新發現後才廣為人知。據報告,到2007年,甲氧麻黃酮可在網際網路上出售; 到2008年,執法機構已意識到該化合物; 到2010年,在歐洲大部分地區都有報導,在英國尤為普遍。甲氧麻黃酮在2008年首先在以色列被定為非法,隨後是瑞典。2010年,在許多歐洲國家/地區將其定為違法,2010年12月,歐盟裁定該法為違法。在澳大利亞、紐西蘭和美國,它被認為是其他非法藥物的類似物,可以通過類似於《聯邦模擬法》的法律加以控制。自2011年10月起,美國於2011年9月將甲氧麻黃酮暫時歸類為非法。
甲基安非他命
[編輯]甲基苯丙胺是一種有效的苯乙胺和苯丙胺類興奮劑,用於治療注意力不足過動症(ADHD)和肥胖症。[57][58][59]甲基苯丙胺以右旋和左旋兩種對映體形式存在。[60][61]與左旋甲基苯丙胺相比,右旋甲基苯丙胺是一種更強的中樞神經系統興奮劑;[23][60][61]然而,它們都具有成癮性,並且在高劑量時會產生相同的毒性症狀。[61]儘管由於潛在的風險很少開處方,但鹽酸甲基苯丙胺已被美國食品和藥物管理局(USFDA)批准,商品名為Desoxyn。[58] 甲基苯丙胺在娛樂上被用來增加性慾,提升心情和增加精力,使一些使用者連續幾天連續進行性活動。[58][62]
甲基苯丙胺可能以純右旋甲基苯丙胺或左右手分子等比例混合的混合物(即50%左旋甲基苯丙胺和50%右旋甲基苯丙胺)非法出售。[62]在美國,右甲基苯丙胺和外消旋甲基苯丙胺均為附表II管制物質。[58]此外,由於甲基苯丙胺已列入《聯合國精神藥物公約》附表二,因此在許多其他國家受到限制或非法生產、分發、銷售和擁有甲基苯丙胺。[63][64]相比之下,左旋苯丙胺是美國的一種非處方藥。[註 1]
在低劑量下,甲基苯丙胺會引起疲勞的人情緒升高、提高機敏性、注意力和精力。[23][58]大劑量服用可誘發精神病、橫紋肌溶解和腦出血。[23][58] 已知甲基苯丙胺具有很高的濫用和成癮潛力。[23][58]娛樂性使用甲基苯丙胺可能會導致精神病或戒斷後綜合症,這種戒斷綜合症可以持續超過典型戒斷期數月。[67]與苯丙胺和古柯鹼不同,甲基苯丙胺對人類具有神經毒性,會破壞中樞神經系統(CNS)的多巴胺和5-羥色胺神經元。[57][59]與長期使用苯丙胺完全相反的是,有證據表明,甲基苯丙胺會因長期使用而對人造成大腦損害; [57][59]這種損害包括大腦結構和功能的不利變化,例如減少灰質。 腦幾個區域的血容量和代謝完整性標誌物的不利變化。[68][69][59]
派醋甲酯
[編輯]派醋甲酯是一種中樞神經系統興奮劑 其結構和藥理與安非他命、古柯鹼相似,能改善使用者的情緒和專注力,被應用於注意力不足過動症(ADHD)、嗜睡症、躁鬱症和憂鬱症的治療。
古柯鹼
[編輯]
古柯鹼是一種5-羥色胺、去甲腎上腺素和多巴胺再攝取抑制劑,古柯鹼由古柯灌木的葉子製成,古柯灌木生長在南美國家的玻利維亞、哥倫比亞和秘魯等山區。在歐洲、北美和亞洲的某些地區,古柯鹼最常見的形式是白色結晶性粉末。古柯鹼是一種興奮劑,儘管古柯鹼將臨床用途視為局部麻醉劑,特別是在眼科領域,但由於其興奮性而通常在治療上並未開處方。古柯鹼的大多數使用是娛樂性的,其濫用潛力很高(高於苯丙胺),因此在大多數轄區都嚴格控制其銷售和擁有。其他與古柯鹼有關的莨菪烷衍生物藥物也眾所周知,例如troparil和lometopane,但尚未廣泛銷售或用於娛樂。[70]
尼古丁
[編輯]尼古丁是菸草中的活性化學成分,有多種形式,包括香菸、雪茄、咀嚼菸草和戒菸輔助劑,例如尼古丁貼片、尼古丁口香糖和電子香菸。尼古丁具有刺激和放鬆作用,因此在世界範圍內得到廣泛使用。尼古丁通過菸鹼乙醯膽鹼受體的激動作用發揮其作用,從而導致多種下游效應,例如中腦獎賞系統中多巴胺能神經元活性的增加,其中一種菸葉乙醛降低了大腦中單胺氧化酶的表達。[71]尼古丁會上癮並形成依賴性。菸草是尼古丁最常見的來源,對使用者和自己的總體危害比古柯鹼低3%,比苯丙胺高13%,在通過多標準決策分析確定的20種藥物中,危害最大的是第六位。[72]
醫療用途
[編輯]中樞神經刺激劑在醫學上用來治療肥胖、睡眠疾患、嗜睡症(narcolepsy)、情感性疾患、注意力不足過動症、頑固型憂鬱症、頑固型強迫症、氣喘、鼻塞等[3][73]。
用來治療 ADHD(注意力不足過動症)的興奮劑包括哌甲酯、苯丙胺、右旋安非他命、二甲磺酸賴右苯丙胺等[3]。
安全性
[編輯]只要按照指示使用,中樞神經刺激劑如同其他藥品一樣安全,不會導致藥物濫用或成癮。
研究顯示,以中樞神經興奮劑治療注意力不足過動症的患者,其往後將比沒有以中樞神經興奮劑治療的注意力不足過動症患者享有明顯更低的藥物濫用風險[3]。
副作用
[編輯]如同其他藥物,中樞神經刺激劑也有副作用產生的可能,然而不是每個服用興奮劑的人都會有副作用。這些副作用大都是輕微的,並且在劑量降低或與其他藥物併用、調整服藥時間等調適後消失。
較常見的副作用[註 2]包含:
- 難以入睡或難以維持睡眠。
- 胃口降低。
- 胃部不適。
- 頭疼。
- 肢體抽動或聲音抽動。(突然的、重複的動作或聲音)(抽搐)
備註
[編輯]參考文獻
[編輯]- ^ stimulant - definition of stimulant in English | Oxford Dictionaries. Oxford Dictionaries | English. [2017-04-15]. (原始內容存檔於2017-02-26).
- ^ Treatment, Center for Substance Abuse. Chapter 2—How Stimulants Affect the Brain and Behavior. Substance Abuse and Mental Health Services Administration (US). [2017-04-15]. (原始內容存檔於2017-02-19) (英語).
- ^ 3.0 3.1 3.2 3.3 3.4 3.5 Mental Health Medications.. National Institute of mental health. (tertiary source). October 2016 [2017-04-15]. (原始內容存檔於2019-04-06).
- ^ Spencer RC, Devilbiss DM, Berridge CW. The Cognition-Enhancing Effects of Psychostimulants Involve Direct Action in the Prefrontal Cortex. Biol. Psychiatry. June 2015, 77 (11): 940–950. PMID 25499957. doi:10.1016/j.biopsych.2014.09.013.
The procognitive actions of psychostimulants are only associated with low doses. Surprisingly, despite nearly 80 years of clinical use, the neurobiology of the procognitive actions of psychostimulants has only recently been systematically investigated. Findings from this research unambiguously demonstrate that the cognition-enhancing effects of psychostimulants involve the preferential elevation of catecholamines in the PFC and the subsequent activation of norepinephrine α2 and dopamine D1 receptors. ... This differential modulation of PFC-dependent processes across dose appears to be associated with the differential involvement of noradrenergic α2 versus α1 receptors. Collectively, this evidence indicates that at low, clinically relevant doses, psychostimulants are devoid of the behavioral and neurochemical actions that define this class of drugs and instead act largely as cognitive enhancers (improving PFC-dependent function). This information has potentially important clinical implications as well as relevance for public health policy regarding the widespread clinical use of psychostimulants and for the development of novel pharmacologic treatments for attention-deficit/hyperactivity disorder and other conditions associated with PFC dysregulation. ... In particular, in both animals and humans, lower doses maximally improve performance in tests of working memory and response inhibition, whereas maximal suppression of overt behavior and facilitation of attentional processes occurs at higher doses.
- ^ Ilieva IP, Hook CJ, Farah MJ. Prescription Stimulants' Effects on Healthy Inhibitory Control, Working Memory, and Episodic Memory: A Meta-analysis. J. Cogn. Neurosci. January 2015: 1–21. PMID 25591060. doi:10.1162/jocn_a_00776.
Specifically, in a set of experiments limited to high-quality designs, we found significant enhancement of several cognitive abilities. ... The results of this meta-analysis ... do confirm the reality of cognitive enhancing effects for normal healthy adults in general, while also indicating that these effects are modest in size.
- ^ Long-term & Short-term effects, depressants, brand names: Foundation for a drug free work. [2017-04-30]. (原始內容存檔於2020-11-27).
- ^ Top 100 Drugs for Q4 2013 by Sales - U.S. Pharmaceutical Statistics. www.drugs.com. [2017-04-15]. (原始內容存檔於2013-08-14).
- ^ Docherty, J R. Pharmacology of stimulants prohibited by the World Anti-Doping Agency (WADA). British Journal of Pharmacology. 7 January 2017, 154 (3): 606–622. ISSN 0007-1188. PMC 2439527
 . PMID 18500382. doi:10.1038/bjp.2008.124.
. PMID 18500382. doi:10.1038/bjp.2008.124.
- ^ Caffeine for the Sustainment of Mental Task Performance: Formulations for Military Operations.. Washington (DC): National Academies Press (US). 2001 [2020-11-07]. (原始內容存檔於2017-10-09) (英語).
- ^ 10.0 10.1 10.2 10.3 Adderall XR Prescribing Information (PDF). United States Food and Drug Administration: 11. June 2013 [7 January 2014]. (原始內容存檔 (PDF)於2014-10-06).
- ^ 11.0 11.1 Liddle DG, Connor DJ. Nutritional supplements and ergogenic AIDS. Prim. Care. June 2013, 40 (2): 487–505. PMID 23668655. doi:10.1016/j.pop.2013.02.009.
Amphetamines and caffeine are stimulants that increase alertness, improve focus, decrease reaction time, and delay fatigue, allowing for an increased intensity and duration of training...
Physiologic and performance effects
· Amphetamines increase dopamine/norepinephrine release and inhibit their reuptake, leading to central nervous system (CNS) stimulation
· Amphetamines seem to enhance athletic performance in anaerobic conditions 39 40
· Improved reaction time
· Increased muscle strength and delayed muscle fatigue
· Increased acceleration
· Increased alertness and attention to task - ^ 12.0 12.1 12.2 Malenka RC, Nestler EJ, Hyman SE. Chapter 13: Higher Cognitive Function and Behavioral Control. Sydor A, Brown RY (編). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience 2nd. New York: McGraw-Hill Medical. 2009: 318. ISBN 978-0-07-148127-4.
Therapeutic (relatively low) doses of psychostimulants, such as methylphenidate and amphetamine, improve performance on working memory tasks both in individuals with ADHD and in normal subjects...it is now believed that dopamine and norepinephrine, but not serotonin, produce the beneficial effects of stimulants on working memory. At abused (relatively high) doses, stimulants can interfere with working memory and cognitive control, as will be discussed below. It is important to recognize, however, that stimulants act not only on working memory function, but also on general levels of arousal and, within the nucleus accumbens, improve the saliency of tasks. Thus, stimulants improve performance on effortful but tedious tasks...through indirect stimulation of dopamine and norepinephrine receptors.
- ^ 13.0 13.1 Montgomery KA. Sexual desire disorders. Psychiatry. June 2008, 5 (6): 50–55. PMC 2695750
 . PMID 19727285.
. PMID 19727285.
- ^ Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, Utzinger L, Fusillo S. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J. Am. Acad. Child Adolesc. Psychiatry. January 2008, 47 (1): 21–31. PMID 18174822. doi:10.1097/chi.0b013e31815a56f1.
Stimulant misuse appears to occur both for performance enhancement and their euphorogenic effects, the latter being related to the intrinsic properties of the stimulants (e.g., IR versus ER profile)...
Although useful in the treatment of ADHD, stimulants are controlled II substances with a history of preclinical and human studies showing potential abuse liability. - ^ Convention on psychotropic substances. United Nations Treaty Collection. United Nations. [7 January 2014]. (原始內容存檔於2016-03-31).
- ^ Methamphetamine facts. DrugPolicy.org. [7 January 2014]. (原始內容存檔於2018-04-17).
- ^ 17.0 17.1 Chawla S, Le Pichon T. World Drug Report 2006 (PDF). United Nations Office on Drugs and Crime: 128–135. 2006 [7 January 2014]. (原始內容存檔 (PDF)於2013-05-30).
- ^ 18.0 18.1 Heal DJ, Smith SL, Gosden J, Nutt DJ. Amphetamine, past and present – a pharmacological and clinical perspective. J. Psychopharmacol. June 2013, 27 (6): 479–496. PMC 3666194
 . PMID 23539642. doi:10.1177/0269881113482532.
. PMID 23539642. doi:10.1177/0269881113482532.
- ^ Rasmussen N. Making the first anti-depressant: amphetamine in American medicine, 1929–1950. J. Hist. Med. Allied Sci. July 2006, 61 (3): 288–323. PMID 16492800. doi:10.1093/jhmas/jrj039.
- ^ Adderall IR Prescribing Information (PDF). United States Food and Drug Administration: 5. March 2007 [2 November 2013]. (原始內容存檔 (PDF)於2013-09-26).
- ^ Miller GM. The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity. J. Neurochem. January 2011, 116 (2): 164–176. PMC 3005101
 . PMID 21073468. doi:10.1111/j.1471-4159.2010.07109.x.
. PMID 21073468. doi:10.1111/j.1471-4159.2010.07109.x.
- ^ Adderall XR Prescribing Information (PDF). United States Food and Drug Administration: 4–8. June 2013 [7 October 2013]. (原始內容存檔 (PDF)於2014-10-06).
- ^ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 Westfall DP, Westfall TC. Miscellaneous Sympathomimetic Agonists. Brunton LL, Chabner BA, Knollmann BC (編). Goodman & Gilman's Pharmacological Basis of Therapeutics 12th. New York: McGraw-Hill. 2010 [2020-11-05]. ISBN 978-0-07-162442-8. (原始內容存檔於2013-11-10).
- ^ 24.0 24.1 Shoptaw SJ, Kao U, Ling W. Treatment for amphetamine psychosis (Review). Cochrane Database of Systematic Reviews. 2009, (1): CD003026. PMC 7004251
 . PMID 19160215. doi:10.1002/14651858.CD003026.pub3.
. PMID 19160215. doi:10.1002/14651858.CD003026.pub3.
- ^ Lovett R. Coffee: The demon drink?. New Scientist. 24 September 2005, (2518) [3 August 2009]. (原始內容存檔於2008-10-11).

- ^ Nehlig, A.; Daval, J. L.; Debry, G. Caffeine and the central nervous system: mechanisms of action, biochemical, metabolic and psychostimulant effects. Brain Research. Brain Research Reviews. 1 August 2016, 17 (2): 139–170. PMID 1356551. doi:10.1016/0165-0173(92)90012-b.
- ^ Bjorness, Theresa E; Greene, Robert W. Adenosine and Sleep. Current Neuropharmacology. 8 January 2017, 7 (3): 238–245. ISSN 1570-159X. PMC 2769007
 . PMID 20190965. doi:10.2174/157015909789152182.
. PMID 20190965. doi:10.2174/157015909789152182.
- ^ Solinas, Marcello; Ferré, Sergi; You, Zhi-Bing; Karcz-Kubicha, Marzena; Popoli, Patrizia; Goldberg, Steven R. Caffeine Induces Dopamine and Glutamate Release in the Shell of the Nucleus Accumbens. Journal of Neuroscience. 1 August 2002, 22 (15): 6321–6324. ISSN 0270-6474. PMC 6758129
 . PMID 12151508. doi:10.1523/JNEUROSCI.22-15-06321.2002 (英語).
. PMID 12151508. doi:10.1523/JNEUROSCI.22-15-06321.2002 (英語).
- ^ Kamiya T, Saitoh O, Yoshioka K, Nakata H. Oligomerization of adenosine A2A and dopamine D2 receptors in living cells. Biochemical and Biophysical Research Communications. Jun 2003, 306 (2): 544–9. PMID 12804599. doi:10.1016/S0006-291X(03)00991-4.
- ^ Fishchman, N; Mello, N. Testing for Abuse Liability of Drugs in Humans (PDF). 5600 Fishers Lane Rockville, MD 20857: U.S. Department of Health and Human Services Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse. : 179 [2020-11-05]. (原始內容 (PDF)存檔於2016-12-22).
- ^ Temple JL. Caffeine use in children: what we know, what we have left to learn, and why we should worry. Neuroscience and Biobehavioral Reviews. 2009, 33 (6): 793–806. PMC 2699625
 . PMID 19428492. doi:10.1016/j.neubiorev.2009.01.001.
. PMID 19428492. doi:10.1016/j.neubiorev.2009.01.001.
- ^ Nkondjock A. Coffee consumption and the risk of cancer: an overview. Cancer Lett. May 2009, 277 (2): 121–5. PMID 18834663. doi:10.1016/j.canlet.2008.08.022.
- ^ 33.0 33.1 Arab L. Epidemiologic evidence on coffee and cancer. Nutrition and Cancer. 2010, 62 (3): 271–83. PMID 20358464. doi:10.1080/01635580903407122.
- ^ Santos C, Costa J, Santos J, Vaz-Carneiro A, Lunet N. Caffeine intake and dementia: systematic review and meta-analysis. J. Alzheimers Dis. 2010,. 20 Suppl 1: S187–204. PMID 20182026. doi:10.3233/JAD-2010-091387.
- ^ Marques S, Batalha VL, Lopes LV, Outeiro TF. Modulating Alzheimer's disease through caffeine: a putative link to epigenetics. J. Alzheimers Dis. 2011, 24 (2): 161–71. PMID 21427489. doi:10.3233/JAD-2011-110032.
- ^ Arendash GW, Cao C. Caffeine and coffee as therapeutics against Alzheimer's disease. J. Alzheimers Dis. 2010,. 20 Suppl 1: S117–26 [2020-11-05]. PMID 20182037. doi:10.3233/JAD-2010-091249. (原始內容存檔於2020-10-30).
- ^ Ding M, Bhupathiraju SN, Satija A, van Dam RM, Hu FB. Long-term coffee consumption and risk of cardiovascular disease: a systematic review and a dose-response meta-analysis of prospective cohort studies.. Circulation. 11 February 2014, 129 (6): 643–59. PMC 3945962
 . PMID 24201300. doi:10.1161/circulationaha.113.005925.
. PMID 24201300. doi:10.1161/circulationaha.113.005925.
- ^ van Dam RM. Coffee consumption and risk of type 2 diabetes, cardiovascular diseases, and cancer. Applied Physiology, Nutrition, and Metabolism. 2008, 33 (6): 1269–1283. PMID 19088789. doi:10.1139/H08-120.
- ^ Zhang Z, Hu G, Caballero B, Appel L, Chen L. Habitual coffee consumption and risk of hypertension: a systematic review and meta-analysis of prospective observational studies. Am. J. Clin. Nutr. June 2011, 93 (6): 1212–9. PMID 21450934. doi:10.3945/ajcn.110.004044.
- ^ Li M, Wang M, Guo W, Wang J, Sun X. The effect of caffeine on intraocular pressure: a systematic review and meta-analysis. Graefes Arch. Clin. Exp. Ophthalmol. March 2011, 249 (3): 435–42. PMID 20706731. doi:10.1007/s00417-010-1455-1.
- ^ Muriel P, Arauz J. Coffee and liver diseases. Fitoterapia. 2010, 81 (5): 297–305. PMID 19825397. doi:10.1016/j.fitote.2009.10.003.
- ^ O'Connor A. Never shower in a thunderstorm : surprising facts and misleading myths about our health and the world we live in 1st. New York: Times Books. 2007: 144 [15 January 2014]. ISBN 978-0-8050-8312-5. (原始內容存檔於2020-02-12).
- ^ Gilmore B, Michael M. Treatment of acute migraine headache. Am Fam Physician. February 2011, 83 (3): 271–80. PMID 21302868.
- ^ Hackett PH. Caffeine at high altitude: java at base Camp. High Alt. Med. Biol. 2010, 11 (1): 13–7. PMID 20367483. doi:10.1089/ham.2009.1077.
- ^ Merck Manuals EPHEDrine (頁面存檔備份,存於網際網路檔案館) Last full review/revision January 2010
- ^ Meyer, Jerrold S. 3,4-methylenedioxymethamphetamine (MDMA): current perspectives. Substance Abuse and Rehabilitation. 21 November 2013, 4: 83–99. ISSN 1179-8467. PMC 3931692
 . PMID 24648791. doi:10.2147/SAR.S37258.
. PMID 24648791. doi:10.2147/SAR.S37258.
- ^ Nutt, David; King, Leslie A.; Saulsbury, William; Blakemore, Colin. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 24 March 2007, 369 (9566): 1047–1053. ISSN 1474-547X. PMID 17382831. doi:10.1016/S0140-6736(07)60464-4.
- ^ Editor, Christopher Hope. Ecstasy 'no more dangerous than horse riding'. Telegraph.co.uk. 2009-02-07 [4 December 2015]. (原始內容存檔於2015-12-10).
- ^ Simmler, L. D.; Buser, T. A.; Donzelli, M.; Schramm, Y; Dieu, L-H.; Huwyler, J.; Chaboz, S.; Hoener, M. C.; Liechti, M. E. Pharmacological characterization of designer cathinones in vitro. British Journal of Pharmacology. 2012, 168 (2): 458–470. ISSN 0007-1188. PMC 3572571
 . PMID 22897747. doi:10.1111/j.1476-5381.2012.02145.x.
. PMID 22897747. doi:10.1111/j.1476-5381.2012.02145.x.
- ^ US Patent 3478050 – 1-(3,4-methylenedioxy-phenyl)-2-pyrrolidino-alkanones
- ^ Abuse Of Fake 'Bath Salts' Sends Dozens To ER. KMBC.com. 23 December 2010 [2020-11-06]. (原始內容存檔於2011-07-13).
- ^ MDPV Bath Salts Drug Over The Counter. [2020-11-06]. (原始內容存檔於2011-03-10).
- ^ Samantha Morgan. Parents cautioned against over the counter synthetic speed. NBC 33 News. 9 November 2010 [16 May 2011]. (原始內容存檔於2011-09-28).
- ^ Kelsey Scram. Bath Salts Used to Get High. NBC 33 News. 6 January 2011 [16 May 2011]. (原始內容存檔於2011-09-28).
- ^ Cumming, E. Mephedrone: Chemistry lessons. The Daily Telegraph (London). 22 April 2010 [14 September 2010]. (原始內容存檔於2014-01-07).
- ^ Drugs crackdown hailed a success. BBC News. 8 March 2010 [31 March 2010]. (原始內容存檔於2012-08-26).
- ^ 57.0 57.1 57.2 Malenka RC, Nestler EJ, Hyman SE. 15. Sydor A, Brown RY (編). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience 2nd. New York: McGraw-Hill Medical. 2009: 370. ISBN 9780071481274.
Unlike cocaine and amphetamine, methamphetamine is directly toxic to midbrain dopamine neurons.
- ^ 58.0 58.1 58.2 58.3 58.4 58.5 58.6 Desoxyn Prescribing Information (PDF). United States Food and Drug Administration. December 2013 [6 January 2014]. (原始內容存檔 (PDF)於2014-01-02).
- ^ 59.0 59.1 59.2 59.3 Krasnova IN, Cadet JL. Methamphetamine toxicity and messengers of death. Brain Res. Rev. May 2009, 60 (2): 379–407. PMC 2731235
 . PMID 19328213. doi:10.1016/j.brainresrev.2009.03.002.
. PMID 19328213. doi:10.1016/j.brainresrev.2009.03.002. Neuroimaging studies have revealed that METH can indeed cause neurodegenerative changes in the brains of human addicts (Aron and Paulus, 2007; Chang et al., 2007). These abnormalities include persistent decreases in the levels of dopamine transporters (DAT) in the orbitofrontal cortex, dorsolateral prefrontal cortex, and the caudate-putamen (McCann et al., 1998, 2008; Sekine et al., 2003; Volkow et al., 2001a, 2001c). The density of serotonin transporters (5-HTT) is also decreased in the midbrain, caudate, putamen, hypothalamus, thalamus, the orbitofrontal, temporal, and cingulate cortices of METH-dependent individuals (Sekine et al., 2006) ...
Neuropsychological studies have detected deficits in attention, working memory, and decision-making in chronic METH addicts ...
There is compelling evidence that the negative neuropsychiatric consequences of METH abuse are due, at least in part, to drug-induced neuropathological changes in the brains of these METH-exposed individuals ...
Structural magnetic resonance imaging (MRI) studies in METH addicts have revealed substantial morphological changes in their brains. These include loss of gray matter in the cingulate, limbic, and paralimbic cortices, significant shrinkage of hippocampi, and hypertrophy of white matter (Thompson et al., 2004). In addition, the brains of METH abusers show evidence of hyperintensities in white matter (Bae et al., 2006; Ernst et al., 2000), decreases in the neuronal marker, N-acetylaspartate (Ernst et al., 2000; Sung et al., 2007), reductions in a marker of metabolic integrity, creatine (Sekine et al., 2002) and increases in a marker of glial activation, myoinositol (Chang et al., 2002; Ernst et al., 2000; Sung et al., 2007; Yen et al., 1994). Elevated choline levels, which are indicative of increased cellular membrane synthesis and turnover are also evident in the frontal gray matter of METH abusers (Ernst et al., 2000; Salo et al., 2007; Taylor et al., 2007). - ^ 60.0 60.1 Kuczenski R, Segal DS, Cho AK, Melega W. Hippocampus norepinephrine, caudate dopamine and serotonin, and behavioral responses to the stereoisomers of amphetamine and methamphetamine. J. Neurosci. February 1995, 15 (2): 1308–1317. PMC 6577819
 . PMID 7869099. doi:10.1523/JNEUROSCI.15-02-01308.1995.
. PMID 7869099. doi:10.1523/JNEUROSCI.15-02-01308.1995.
- ^ 61.0 61.1 61.2 Mendelson J, Uemura N, Harris D, Nath RP, Fernandez E, Jacob P, Everhart ET, Jones RT. Human pharmacology of the methamphetamine stereoisomers. Clin. Pharmacol. Ther. October 2006, 80 (4): 403–420. PMID 17015058. doi:10.1016/j.clpt.2006.06.013.
- ^ 62.0 62.1 San Francisco Meth Zombies. Drugs, Inc.. 第4季. 第1集. 43 記錄於. 11 August 2013 [2020-11-07]. ASIN B00EHAOBAO. National Geographic Channel. (原始內容存檔於2016-07-08).
- ^ United Nations Office on Drugs and Crime. Preventing Amphetamine-type Stimulant Use Among Young People: A Policy and Programming Guide (PDF). New York: United Nations. 2007 [11 November 2013]. ISBN 9789211482232. (原始內容存檔 (PDF)於2013-10-16).
- ^ List of psychotropic substances under international control (PDF). International Narcotics Control Board. United Nations. August 2003 [19 November 2005]. (原始內容存檔 (PDF)於2005-09-07).
- ^ CFR TITLE 21: DRUGS FOR HUMAN USE: PART 341 – COLD, COUGH, ALLERGY, BRONCHODILATOR, AND ANTIASTHMATIC DRUG PRODUCTS FOR OVER-THE-COUNTER HUMAN USE. United States Food and Drug Administration. April 2015 [7 March 2016]. (原始內容存檔於2015-09-18).
Topical nasal decongestants --(i) For products containing levmetamfetamine identified in 341.20(b)(1) when used in an inhalant dosage form. The product delivers in each 800 milliliters of air 0.04 to 0.150 milligrams of levmetamfetamine.
- ^ Levomethamphetamine. Pubchem Compound. National Center for Biotechnology Information. (原始內容存檔於2014-10-06) 使用
|archiveurl=需要含有|url=(幫助).|section-url=被忽略 (幫助);|section=被忽略 (幫助); - ^ Cruickshank CC, Dyer KR. A review of the clinical pharmacology of methamphetamine. Addiction. July 2009, 104 (7): 1085–1099. PMID 19426289. doi:10.1111/j.1360-0443.2009.02564.x.
- ^ Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K. Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects. JAMA Psychiatry. February 2013, 70 (2): 185–198. PMID 23247506. doi:10.1001/jamapsychiatry.2013.277.
- ^ Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, Faraone SV, Biederman J. Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies. J. Clin. Psychiatry. September 2013, 74 (9): 902–917. PMC 3801446
 . PMID 24107764. doi:10.4088/JCP.12r08287.
. PMID 24107764. doi:10.4088/JCP.12r08287.
- ^ AJ Giannini; WC Price. Contemporary drugs of abuse. American Family Physician. 1986, 33: 207–213.
- ^ Talhouth, Reinskje; Opperhuizen, Antoon; van Amsterdam G. C., Jan. Role of acetaldehyde in tobacco smoke addiction. European Neuropsychopharmacology. October 2007, 17 (10): 627–636. PMID 17382522. doi:10.1016/j.euroneuro.2007.02.013.
- ^ Nutt, David J.; King, Leslie A.; Phillips, Lawrence D. Drug harms in the UK: a multicriteria decision analysis. Lancet. 6 November 2010, 376 (9752): 1558–1565. ISSN 1474-547X. PMID 21036393. doi:10.1016/S0140-6736(10)61462-6.
- ^ Harper, S. J.; Jones, N. S. Cocaine: what role does it have in current ENT practice? A review of the current literature. The Journal of Laryngology and Otology. 1 October 2006, 120 (10): 808–811. ISSN 1748-5460. PMID 16848922. doi:10.1017/S0022215106001459.
