卡维地洛
 | |
 | |
| 临床资料 | |
|---|---|
| 商品名 | Coreg及其他 |
| 其他名称 | BM-14190 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a697042 |
| 核准状况 | |
| 给药途径 | 口服给药 |
| ATC码 | |
| 法律规范状态 | |
| 法律规范 |
|
| 药物动力学数据 | |
| 生物利用度 | 25–35% |
| 血浆蛋白结合率 | 98% |
| 药物代谢 | 肝脏 (细胞色素CYP2D6及CYP2C9) |
| 生物半衰期 | 7–10小时 |
| 排泄途径 | 尿液 (16%), 粪便 (60%) |
| 识别信息 | |
| |
| CAS号 | 72956-09-3 |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB配体ID | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.117.236 |
| 化学信息 | |
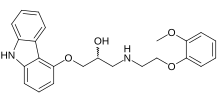
| 化学式 | C24H26N2O4 |
| 摩尔质量 | 406.48 g·mol−1 |
| 3D模型(JSmol) | |
| 手性 | 外消旋体 |
| |
| |
卡维地洛(英语:Carvedilol)以Coreg等商品名于市面贩售,是种用于治疗高血压、郁血性心脏衰竭 (CHF) 和左心室功能障碍的药物。[1]此药物于治疗高血压时通常是作为一种二线药物。[1]
使用后常见的副作用有头晕、疲倦、关节痛、低血压、恶心和呼吸困难。[1]严重的副作用有支气管痉挛。[1]个体于怀孕期间使用对于胎儿的安全,或个体进行母乳哺育时对于婴儿的安全尚未有充分的数据以供研究。[2]不建议罹患肝病的人使用。[3]卡维地洛是一种非选择性β受体阻滞剂,并具有选择性α-1受体阻滞剂的活性。[1]此药物发生作用的机制尚未被完全了解,但涉及的可能是血管舒张的结果。[1]
卡维地洛于1978年获得专利,并于1995年被美国食品药物管理局(FDA)核准作医疗用途。[1][4]它已被列入世界卫生组织基本药物标准清单中。[5]目前市面上有通用名药物贩售。[1]它于美国2021年最常使用处方药中排名第26,开立的处方笺数量超过2,100万张。[6][7]
医疗用途
[编辑]卡维地洛适用于郁血性心脏衰竭 (CHF)的治疗,通常作为血管张力素转化酶抑制剂 (ACE抑制剂) ,及利尿剂的辅助药物。临床证明它可降低CHF患者的死亡率和住院率。[8]卡维地洛治疗心脏衰竭的机制在于它能抑制交感神经系统中的受体(此系统会释放正肾上腺素至全身,包括心脏)。[9]正肾上腺素是一种可使心脏跳动更快、更努力运作的激素。[9]阻断正肾上腺素与心脏中受体的结合可导致血管舒张,降低心率和血压,并改善心肌收缩力,[10]最终把心脏的负荷降低。[9]
卡维地洛可降低心脏病发作后患者因心脏功能下降而致的死亡、住院和心脏病复发的风险。[11][12]卡维地洛也被证明可减少严重心脏衰竭患者的死亡和住院率。[13]
卡维地洛在一般医疗过程中已被用于治疗单纯性高血压,但研究显示它与其他降血压药物或是其他β受体阻滞剂相比,降血压的效果会相对较低。[14]
卡维地洛也具有预防肝硬化患者因食道静脉曲张发生流血的功效。[15]
配方形式
[编辑]卡维地洛的配方形式有:
禁忌症
[编辑]患有支气管气喘或支气管痉挛的患者不应使用卡维地洛,因为此药物会升高支气管收缩的风险。[18][19]患有二度或三度房室传导阻滞、窦房结功能障碍(心脏传导疾病 )、严重心跳过缓(除非个体安装有永久性心律调节器)或失代偿性心脏病(即心脏衰竭)的患者也不应使用此药物。有严重肝功能损害的患者应谨慎使用。[20][21][22]
副作用
[编辑]卡维地洛导致的副作用中最常见的(发生率 >10%)有:[16]
不建议患有恶化型支气管痉挛疾病(例如目前有气喘症状)的人使用卡维地洛,因为它会阻断有助于打开气道的受体。[16]
卡维地洛可能会将低血糖症状掩盖,[16]导致糖尿病低血糖症发生却不自觉的情况(低血糖无自觉症状)。这情况被称为β受体阻滞剂引起的低血糖无自觉症状。糖尿病低血糖症是指糖尿病患者的血糖水平低于正常范围(低血糖),它是急诊室和医院最常遇到的低血糖原因之一。根据美国国家电子伤害监测系统 - 全方位伤害程序 (National Electronic Injury Surveillance System-All Injury Program, NEISS-AIP) 的数据,美国在2004年至2005年之间抽样调查的案例中,估计有55,819起病例 (占总住院人数的8.0%) 与胰岛素使用有关联,其中严重低血糖症可能是最常见的一种结果。[23]
与其他药物交互作用
[编辑]如果将此药物与胺碘酮、地高辛、地尔硫䓬、伊伐布雷定或维拉帕米一起使用,会增加心跳过慢的风险。[24]此外,卡维地洛与非1,4-二氢吡啶类钙通道阻滞剂(包括地尔硫䓬和维拉帕米)组合使用,可增强其心脏抑制作用。[24]
药理学
[编辑]药效学
[编辑]卡维地洛既是一种非选择性β受体阻滞剂(β1与β2),也是一种选择性α-1受体阻滞剂(α1)。[1]
卡维地洛可阻断α-1受体,导致血管舒张。这种抑制作用造成周边血管阻力降低,而产生抗高血压作用。由于卡维地洛会阻断心脏中的β1受体,而停止产生反射性心跳过速反应。[25]
药物动力学
[编辑]口服卡维地洛后,由于广泛的首过代谢,药物的生物利用度约为25%至35%。饮食期间服用会将药物吸收减慢,但生物利用度无显著差异。给药期间同时进食可降低姿位性低血压的风险。[16]
大部分卡维地洛与血浆蛋白结合(主要是人类血清白蛋白),可达98%。卡维地洛是一种脂溶性药物,在动物实验中容易穿过血脑屏障。因此它不像是一些只会作用于外周组织(人体中枢神经系统以外的所有组织和器官)的药物。[26][27]
参考文献
[编辑]- ^ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 Carvedilol Monograph for Professionals. Drugs.com. AHFS. [2018-12-24]. (原始内容存档于2011-01-20).
- ^ Carvedilol Use During Pregnancy. Drugs.com. [2018-12-24]. (原始内容存档于2009-12-23).
- ^ British national formulary : BNF 76 76. Pharmaceutical Press. 2018: 147. ISBN 9780857113382.
- ^ Fischer J, Ganellin CR. Analogue-based Drug Discovery. John Wiley & Sons. 2006: 463. ISBN 9783527607495.
- ^ World Health Organization. World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. hdl:10665/345533
 . WHO/MHP/HPS/EML/2021.02.
. WHO/MHP/HPS/EML/2021.02.
- ^ The Top 300 of 2021. ClinCalc. [2024-01-14]. (原始内容存档于2024-01-15).
- ^ Carvedilol - Drug Usage Statistics. ClinCalc. [2024-01-14]. (原始内容存档于2020-04-11).
- ^ Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, Wilkoff BL. 2013 AHA Guidelines for the Management of Heart Failure (PDF). Circulation. 2013-10-15, 128 (16): e240–327 [2024-05-17]. PMID 23741058. doi:10.1161/CIR.0b013e31829e8776. (原始内容存档 (PDF)于2016-01-14). 已忽略未知参数
|collaboration=(帮助) - ^ 9.0 9.1 9.2 Ogbru O. Shiel Jr WC , 编. carvedilol (Coreg): Heart Failure, Side Effects, Uses & Dosage. MedicineNet. 4 November 2022 [2024-05-01]. (原始内容存档于2024-05-01) (英语).
- ^ Kubon C, Mistry NB, Grundvold I, Halvorsen S, Kjeldsen SE, Westheim AS. The role of beta-blockers in the treatment of chronic heart failure. Trends in Pharmacological Sciences. April 2011, 32 (4): 206–212. PMID 21376403. doi:10.1016/j.tips.2011.01.006.
- ^ Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. May 2001, 357 (9266): 1385–1390. PMID 11356434. S2CID 1840228. doi:10.1016/s0140-6736(00)04560-8.
- ^ Huang BT, Huang FY, Zuo ZL, Liao YB, Heng Y, Wang PJ, Gui YY, Xia TL, Xin ZM, Liu W, Zhang C, Chen SJ, Pu XB, Chen M, Huang DJ. Meta-Analysis of Relation Between Oral β-Blocker Therapy and Outcomes in Patients With Acute Myocardial Infarction Who Underwent Percutaneous Coronary Intervention. The American Journal of Cardiology. June 2015, 115 (11): 1529–1538. PMID 25862157. doi:10.1016/j.amjcard.2015.02.057.
- ^ Cleland JG, Bunting KV, Flather MD, Altman DG, Holmes J, Coats AJ, Manzano L, McMurray JJ, Ruschitzka F, van Veldhuisen DJ, von Lueder TG, Böhm M, Andersson B, Kjekshus J, Packer M, Rigby AS, Rosano G, Wedel H, Hjalmarson Å, Wikstrand J, Kotecha D. Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. European Heart Journal. January 2018, 39 (1): 26–35. PMC 5837435
 . PMID 29040525. doi:10.1093/eurheartj/ehx564.
. PMID 29040525. doi:10.1093/eurheartj/ehx564.
- ^ Wong GW, Laugerotte A, Wright JM. Blood pressure lowering efficacy of dual alpha and beta blockers for primary hypertension. The Cochrane Database of Systematic Reviews. August 2015, 2015 (8): CD007449. PMC 6486308
 . PMID 26306578. doi:10.1002/14651858.cd007449.pub2.
. PMID 26306578. doi:10.1002/14651858.cd007449.pub2.
- ^ Reiberg, T, Ulbrich, G, et al. Carvedilol for primary prophylaxis of variceal bleeding in cirrhotic patients with haemodynamic non-response to propranolol. Gut. November 2013, 62 (11): 1634–1641. PMID 23250049. doi:10.1136/gutjnl-2012-304038
 .
.
- ^ 16.0 16.1 16.2 16.3 16.4 16.5 Coreg - Food and Drug Administration (PDF). [2024-05-17]. (原始内容存档 (PDF)于2016-03-04).
- ^ Drug Approval Package. www.accessdata.fda.gov. [2015-11-05]. (原始内容存档于2015-08-10).
- ^ Morales DR, Lipworth BJ, Donnan PT, Jackson C, Guthrie B. Respiratory effect of beta-blockers in people with asthma and cardiovascular disease: population-based nested case control study. BMC Medicine. January 2017, 15 (1): 18. PMC 5270217
 . PMID 28126029. doi:10.1186/s12916-017-0781-0
. PMID 28126029. doi:10.1186/s12916-017-0781-0  .
.
- ^ Kotlyar E, Keogh AM, Macdonald PS, Arnold RH, McCaffrey DJ, Glanville AR. Tolerability of carvedilol in patients with heart failure and concomitant chronic obstructive pulmonary disease or asthma. The Journal of Heart and Lung Transplantation. December 2002, 21 (12): 1290–5. PMID 12490274. doi:10.1016/s1053-2498(02)00459-x.
- ^ Sinha R, Lockman KA, Mallawaarachchi N, Robertson M, Plevris JN, Hayes PC. Carvedilol use is associated with improved survival in patients with liver cirrhosis and ascites (PDF). Journal of Hepatology. July 2017, 67 (1): 40–46. PMID 28213164. doi:10.1016/j.jhep.2017.02.005. hdl:20.500.11820/7afe3b88-1064-4da1-927e-4d4e867387eb.
- ^ Zacharias AP, Jeyaraj R, Hobolth L, Bendtsen F, Gluud LL, Morgan MY. Carvedilol versus traditional, non-selective beta-blockers for adults with cirrhosis and gastroesophageal varices. The Cochrane Database of Systematic Reviews. October 2018, 2018 (10): CD011510. PMC 6517039
 . PMID 30372514. doi:10.1002/14651858.CD011510.pub2.
. PMID 30372514. doi:10.1002/14651858.CD011510.pub2.
- ^ Lo GH, Chen WC, Wang HM, Yu HC. Randomized, controlled trial of carvedilol versus nadolol plus isosorbide mononitrate for the prevention of variceal rebleeding. Journal of Gastroenterology and Hepatology. November 2012, 27 (11): 1681–7. PMID 22849337. S2CID 23494154. doi:10.1111/j.1440-1746.2012.07244.x.
- ^ Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. October 2006, 296 (15): 1858–66. PMID 17047216. doi:10.1001/jama.296.15.1858.
- ^ 24.0 24.1 Koshman SL, Paterson I. Heart Failure. Canadian Pharmacists Association (CPS). 2023-03-15 [2024-04-29].
- ^ Ruffolo RR, Gellai M, Hieble JP, Willette RN, Nichols AJ. The pharmacology of carvedilol. European Journal of Clinical Pharmacology. 1990, 38 (Suppl 2): S82–S88. PMID 1974511. S2CID 2901620. doi:10.1007/BF01409471.
- ^ Wang J, Ono K, Dickstein DL, Arrieta-Cruz I, Zhao W, Qian X, Lamparello A, Subnani R, Ferruzzi M, Pavlides C, Ho L, Hof PR, Teplow DB, Pasinetti GM. Carvedilol as a potential novel agent for the treatment of Alzheimer's disease. Neurobiol Aging. December 2011, 32 (12): 2321.e1–12. PMC 2966505
 . PMID 20579773. doi:10.1016/j.neurobiolaging.2010.05.004.
. PMID 20579773. doi:10.1016/j.neurobiolaging.2010.05.004.
- ^ Bart J, Dijkers EC, Wegman TD, de Vries EG, van der Graaf WT, Groen HJ, Vaalburg W, Willemsen AT, Hendrikse NH. New positron emission tomography tracer [(11)C]carvedilol reveals P-glycoprotein modulation kinetics. Br J Pharmacol. August 2005, 145 (8): 1045–51. PMC 1576233
 . PMID 15951832. doi:10.1038/sj.bjp.0706283.
. PMID 15951832. doi:10.1038/sj.bjp.0706283.
延伸阅读
[编辑]- Chakraborty S, Shukla D, Mishra B, Singh S. Clinical updates on carvedilol: a first choice beta-blocker in the treatment of cardiovascular diseases. Expert Opinion on Drug Metabolism & Toxicology. February 2010, 6 (2): 237–50. PMID 20073998. S2CID 25670550. doi:10.1517/17425250903540220.
- Dean L. Carvedilol Therapy and CYP2D6 Genotype. Pratt VM, McLeod HL, Rubinstein WS, et al (编). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). 2018 [2024-05-17]. PMID 30067327. Bookshelf ID: NBK518573. (原始内容存档于2020-10-26).
